To determine the influence of propofol and thiopental as anaesthetics in electroconvulsive therapy (ECT), as regards, seizure duration, electrical charge, clinical efficacy, cardiovascular profile, and presence of adverse cognitive effects.
MethodsA retrospective design including 127 patients who received bilateral ECT for the treatment of a major depressive episode.
ResultsThe mean seizure duration in the propofol group was significantly shorter than in the thiopental group (21.23±6.09 versus 28.24±6.67s, P<0.001). The mean stimulus charge was 348.22mC in the propofol group, and 238mC in the thiopental group (P<0.001). Propofol was associated with a lower increase in blood pressure. There were no differences between groups in treatment response or presence of adverse effects.
ConclusionsThe anaesthetic agent used in ECT might determine differences in parameters such as seizure duration or electrical charge. However, this does not seem to be translated into differences in clinical efficacy or the pattern of adverse effects observed.
Determinar la influencia de la utilización de propofol y pentotal como anestésicos en la terapia electroconvulsiva (TEC), en relación con la duración de la crisis, la dosis eléctrica, la eficacia clínica, el perfil cardiovascular y la aparición de efectos cognitivos.
MétodoEstudio retrospectivo sobre 127 pacientes que recibieron TEC bilateral como tratamiento de un episodio depresivo mayor.
ResultadosLa duración media de la convulsión eléctrica en el grupo de propofol fue significativamente más corta que en el de pentotal (21,23±6,09 versus 28,24±6,67s; p<0,001). La dosis de estímulo media fue de 348,22 mC en el grupo de propofol y de 238 mC en el grupo de pentotal (p<0,001). Propofol se asoció a un menor incremento de la tensión arterial. No se encontraron diferencias en la respuesta clínica al tratamiento ni en la aparición de otros efectos adversos.
ConclusionesEl anestésico utilizado en la TEC puede determinar diferencias en parámetros como la duración de la crisis o la carga eléctrica aplicada. Sin embargo, estas diferencias no parecen traducirse en la eficacia clínica ni en el patrón de efectos adversos.
Electroconvulsive therapy (ECT) requires sedation with a short-term anaesthetic that interferes as little as possible in the convulsive threshold and in the duration and quality of the convulsion, while simultaneously guaranteeing haemodynamic stability of the patient.1 It is accepted in guidelines, despite being a cause for controversy, that the therapeutic effect of ECT depends on the production of a generalised convulsion of an appropriate duration.2,3 It has been postulated that the choice of anaesthetic could have significant consequences in the performance of ECT, as it might affect the convulsive threshold and modify the duration of the seizure.4,5
Various anaesthetic agents such as methohexital, thiopental, propofol, etomidate and ketamine, characterised by short-term action, are used as inductors in ECT. In spite of the fact that there is no anaesthetic of choice, methohexital seems to be the one with the most generalised use3,6,7; however, it is unavailable in Spain, where propofol and thiopental are the ones used.2,8,9
Propofol has been shown to have a better haemodynamic profile and to facilitate more rapid post-crisis recovery.10–14 However, it could shorten the seizures4,10,15–25 and increase the convulsive threshold,17 which would lead to applying greater electrical stimulation.15,17,20 Consequently, the use of propofol might be associated with a greater number of ECT sessions, as well as with differences in clinical efficacy and increased appearance of adverse effects.26,27
The objective of the study was to analyse any possible differences between propofol and thiopental with respect to ECT parameters, clinical response and adverse effects.
MethodSampleA total of 196 patients were recruited among patients admitted to the psychiatric services at the Hospital Universitari de Bellvitge (thiopental) and the Hospital de Sabadell (propofol) during the 2005–2010 period. They fulfilled DSM-IV-TR diagnostic criteria for major depressive disorder (MDD) and had received an acute course of ECT. We excluded patients having another Axis I disorder (except for nicotine dependence) or Axis II disorder. The final subject count for analysis was 127 patients (32.3% received propofol and 67.7% thiopental).
Variables collectedThrough revising case histories, we collected demographic variables, information on the course of the disorder and that relative to the event. During the hospital stay, psychometric scales–21-item Hamilton Depression Rating Scale (HDRS21) and Global Assessment of Function (GAF)–were administered before the commencement and the end of the course of ECT.
With respect to ECT, we collected the number of sessions, stimulus dose, duration of convulsion per session and accumulated duration (clinical and electroencephalographic), need for restimulation, impedance, cardiovascular parameters (blood pressure and heart rate) and the appearance of other acute adverse effects (headache and cognitive effects).
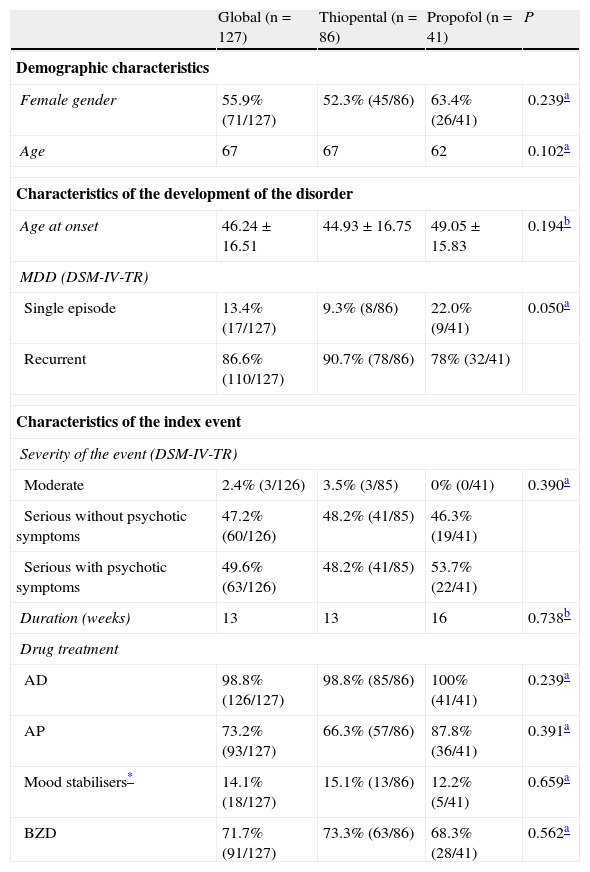
The demographic, clinical and treatment characteristics are presented in Table 1.
Characterisation of the sample.
| Global (n=127) | Thiopental (n=86) | Propofol (n=41) | P | |
| Demographic characteristics | ||||
| Female gender | 55.9% (71/127) | 52.3% (45/86) | 63.4% (26/41) | 0.239a |
| Age | 67 | 67 | 62 | 0.102a |
| Characteristics of the development of the disorder | ||||
| Age at onset | 46.24±16.51 | 44.93±16.75 | 49.05±15.83 | 0.194b |
| MDD (DSM-IV-TR) | ||||
| Single episode | 13.4% (17/127) | 9.3% (8/86) | 22.0% (9/41) | 0.050a |
| Recurrent | 86.6% (110/127) | 90.7% (78/86) | 78% (32/41) | |
| Characteristics of the index event | ||||
| Severity of the event (DSM-IV-TR) | ||||
| Moderate | 2.4% (3/126) | 3.5% (3/85) | 0% (0/41) | 0.390a |
| Serious without psychotic symptoms | 47.2% (60/126) | 48.2% (41/85) | 46.3% (19/41) | |
| Serious with psychotic symptoms | 49.6% (63/126) | 48.2% (41/85) | 53.7% (22/41) | |
| Duration (weeks) | 13 | 13 | 16 | 0.738b |
| Drug treatment | ||||
| AD | 98.8% (126/127) | 98.8% (85/86) | 100% (41/41) | 0.239a |
| AP | 73.2% (93/127) | 66.3% (57/86) | 87.8% (36/41) | 0.391a |
| Mood stabilisers* | 14.1% (18/127) | 15.1% (13/86) | 12.2% (5/41) | 0.659a |
| BZD | 71.7% (91/127) | 73.3% (63/86) | 68.3% (28/41) | 0.562a |
AD: antidepressants; AP: antipsychotics; BZD: benzodiazepines; MDD: major depressive disorder.
The data are presented as medians±standard deviation for continual variables, or as median when necessary, and as percentages for categorical variables (number/total number).
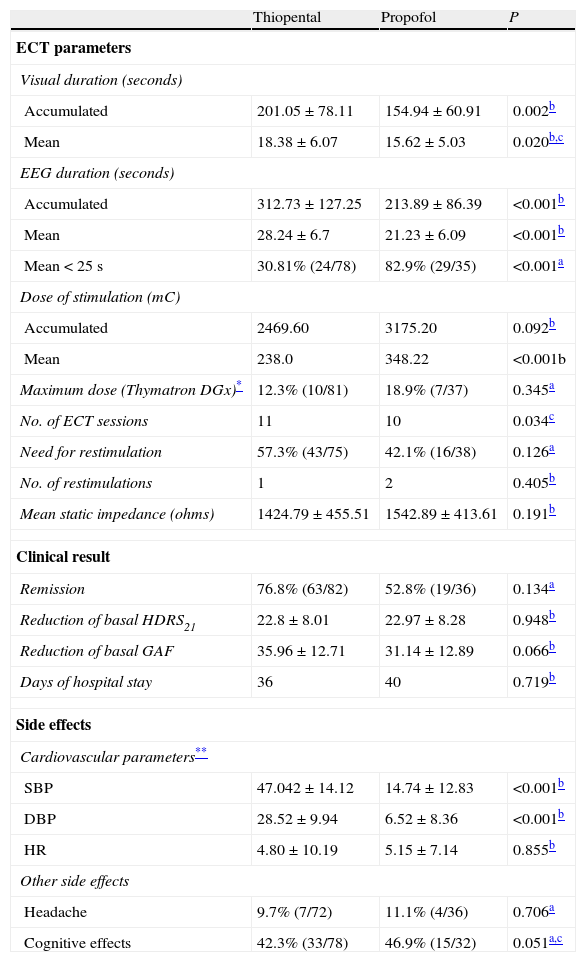
The ECT was administered using Thymatron™ DGx and System IV (DGx and 2× dose/double dose stimulation programmes) following the clinical guidelines.2,3 The anaesthesia included thiopental (1.5–2.5mg/kg) or propofol (0.75–1.5mg/kg) and succinylcholine (0.5mg/kg). The patients were preoxygenated and ventilated manually. The electrode placement was bifrontotemporal.3 The data corresponding to ECT are described in Table 2.
Electroconvulsive therapy parameters, clinical results and side effects.
| Thiopental | Propofol | P | |
| ECT parameters | |||
| Visual duration (seconds) | |||
| Accumulated | 201.05±78.11 | 154.94±60.91 | 0.002b |
| Mean | 18.38±6.07 | 15.62±5.03 | 0.020b,c |
| EEG duration (seconds) | |||
| Accumulated | 312.73±127.25 | 213.89±86.39 | <0.001b |
| Mean | 28.24±6.7 | 21.23±6.09 | <0.001b |
| Mean<25s | 30.81% (24/78) | 82.9% (29/35) | <0.001a |
| Dose of stimulation (mC) | |||
| Accumulated | 2469.60 | 3175.20 | 0.092b |
| Mean | 238.0 | 348.22 | <0.001b |
| Maximum dose (Thymatron DGx)* | 12.3% (10/81) | 18.9% (7/37) | 0.345a |
| No. of ECT sessions | 11 | 10 | 0.034c |
| Need for restimulation | 57.3% (43/75) | 42.1% (16/38) | 0.126a |
| No. of restimulations | 1 | 2 | 0.405b |
| Mean static impedance (ohms) | 1424.79±455.51 | 1542.89±413.61 | 0.191b |
| Clinical result | |||
| Remission | 76.8% (63/82) | 52.8% (19/36) | 0.134a |
| Reduction of basal HDRS21 | 22.8±8.01 | 22.97±8.28 | 0.948b |
| Reduction of basal GAF | 35.96±12.71 | 31.14±12.89 | 0.066b |
| Days of hospital stay | 36 | 40 | 0.719b |
| Side effects | |||
| Cardiovascular parameters** | |||
| SBP | 47.042±14.12 | 14.74±12.83 | <0.001b |
| DBP | 28.52±9.94 | 6.52±8.36 | <0.001b |
| HR | 4.80±10.19 | 5.15±7.14 | 0.855b |
| Other side effects | |||
| Headache | 9.7% (7/72) | 11.1% (4/36) | 0.706a |
| Cognitive effects | 42.3% (33/78) | 46.9% (15/32) | 0.051a,c |
DBP: diastolic blood pressure; ECT: electroconvulsive therapy; EEG: electroencephalograph; HDRS21: Hamilton Depression Rating Scale; HR: heart rate; GAF: global assessment of function; mC: millicoulombs; SBP: systolic blood pressure.
The patients who did not complete treatment were excluded (n=7). The data are presented as means±standard deviation for continual variable, or as medians when necessary, and as percentages for variable categories (number/total number).
All of the patients received concomitant drug treatment during ECT (Table 1).
Development measurementAs the measure of clinical efficacy, we used the difference between the scores on the clinical scales (HDRS21 and GAF) before and after the course of ECT. Remission was considered a HDRS21≤7.28
Cognitive measurement and other adverse effectsA qualitative (yes/no) evaluation was carried out on acute cognitive compromise (subjective memory complaints, non-quantified memory deficits and delirium) and other adverse effects (headaches), using the information noted in the case histories. Cardiovascular parameters were collected before and after each ECT session.
Statistical analysisThe data were analysed using SPSS for Windows, v. 15.0 (SPSS, Chicago, USA). A descriptive analysis of the variables was performed. The potential differences between groups were evaluated using means or medians and (χ2 test or Fisher's exact test and Student's t-test or Mann–Whitney U). The variables that showed an association in the univariate analysis and those considered clinically relevant were included in a multiple regression model (successive steps). Statistical significance was established as P<0.05 (bilateral). The Bonferroni correction was applied for multiple comparisons.
ResultsElectroconvulsive therapy parametersThe propofol group required a mean dose of greater stimulus (P<0.001) and presented shorter seizures (P<0.001). No significant differences were found in the number of ECT sessions received or the need or number of restimulations (Table 2).
To confirm the results, a multiple regression model was performed that included gender, age, impedance and use of hypnotic, benzodiazepine, antiseizure and antipsychotic drugs as variables of interest. The analysis revealed that the use of propofol and, to a lesser degree, greater age and use of benzodiazepines explained up to 34% of the variance associated to the shorter duration of the electric convulsion (corrected R2=0.336, F=19.228; P=0.011). The use of propofol and antiseizure drugs and, to a lesser degree, greater age explained almost 20% of the variance associated to a greater dose of electrical stimulation (corrected R2=0.191; F=9.521; P=0.009).
Clinical response and adverse effectsNo significant differences were found in the clinical response to ECT between the 2 groups, in the percentage of patients that presented remission or in days of hospital stay (Table 2).
Patients treated with propofol presented a lower increase in blood pressure (P<0.001). No differences were found in heart rate or in the presence of headache or cognitive effects (Table 2).
DiscussionThe use of propofol and thiopental as anaesthetic agents during ECT has been evaluated retrospectively. Our results, in agreement with published literature, suggest that the use of propofol is associated to a shorter duration of the seizure and to the need for greater electric stimulation.4,10,15–25 Along the same line, the differences observed between both anaesthetics had no effect on treatment duration, number of sessions administered or clinical response,11,15,20,21,29 the last factor being of marked relevance at a practical level. Only 1 study reported differences in clinical efficacy favourable to thiopental; however, these were only detected in the first 6 sessions of ECT and disappeared at the end of treatment.30
In our study, we did not find any repercussion on the clinical response attributable to a shorter duration of the seizure associated with propofol. This fact, assed to the finding that a high percent of patients show a seizure duration less than 25s, corroborates the current opinion that the duration of the convulsion is not the only indicator of therapeutic efficacy of ECT.3,15,31 Other parameters of convulsion quality, more directly related with the intensity of seizure generalisation than with its duration (such as the postictal suppression index) have been proposed as markers of efficacy.32–36
Another controversial aspect of the anaesthetics used as inductors in ECT is that of cognitive repercussion. There are results favourable to propofol,18,37,38 despite the fact that this anaesthetic requires larger doses of electrical stimulation, a factor that has been related directly to greater cognitive compromise.39 However, this has not been confirmed by other studies11,13,29,40–43 and even a better cognitive profile has been described with thiopental.15,30 The retrospective nature of our study and especially the absence of assessment of cognitive function with specific instruments prevents us from reaching conclusions about this.
Lastly, in our study propofol was associated with a better haemodynamic profile (with respect to increasing blood pressure). The fact had been reported in various studies13,14 and has led to the suggestion that propofol would be preferable in patients with greater cardiovascular risk. In addition, various authors have indicated that the smaller increase in blood pressure associate with propofol could translate into less cognitive compromise.18,37,38
At the practical level, we could conclude that: (1) both anaesthetics seem to be equivalent with respect to clinical ECT efficacy in spite of the differences in the convulsion and need for charge; (2) propofol would present advantages for patients at greater cardiovascular risk; (3) other parameters, beyond just seizure duration, seem to affect the efficacy of the technique; and (4) there are no consistent data as to cognitive compromise associated with using these anaesthetics.
Nonetheless, our results should be interpreted with caution due to the limitations derived from the methodological approach. The main limitations arise from its retrospective nature and the possible bias from the use of each anaesthetic agent in a different centre. However, the significant differences centre on aspects consistently associated with the influence of the anaesthetic agent (duration of the seizure, intensity of electrical stimulation required and adverse cardiovascular effects10,13–25). New controlled random studies that make it possible to increase knowledge on the possible effects of the anaesthetics on clinical efficacy and adverse effects are necessary.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflicts of interests to declare.
The authors wish to thank Eva Aguilar, Noelia Ortuño, Marta Carulla and Joan Carles Oliva for their contributions in the preparation of the study.
Please cite this article as: Martínez-Amorós E, Gálvez Ortiz V, Porter Moli M, Llorens Capdevila M, Cerrillo Albaigés E, Garcia-Parés G, et al. Propofol y pentotal como agentes anestésicos en la terapia electroconvulsiva: un estudio retrospectivo en el trastorno depresivo mayor. Rev Psiquiatr Salud Ment (Barc.). 2014;7:42–47.