The clinical use of mindfulness has increased recently, and the Mindful Attention Awareness Scale (MAAS) has become one of the most used tools to measure it. The aim of this study was to test the effectiveness of mindfulness training and analyzing the psychometric properties of the MAAS scores in a clinical sample using the Rasch Model.
MethodsOne hundred and ninety-nine participants with mood-anxiety clinical symptoms were recruited. The experimental group (n=103) received mindfulness training, and the control group (n=96) a conventional outpatient treatment for the same duration. The pre–post MAAS scores were analyzed to test the effectiveness of training, the psychometric properties of the scores, and differential item functioning (DIF) using the Rating Scale Model (RSM).
ResultsMisfit in items 9 and 12, DIF in item 9, and Spanish translation problems in the items 5, 9 and 12 were observed. The repetition of the analysis without these items was decided. Appropriate dimensionality, fit and reliability values were obtained with the short version, MAAS-12.
ConclusionsContrary to previous studies, the MAAS was sensitive to treatment-associated change. However, the commonly used MAAS has some translation and metric problems, and should be revised. MAAS-12 is a better scale than MAAS but suffers from construct under-representation. Constructing tools from a coherent theoretical perspective is suggested, so that all mindfulness facets are represented.
El uso clínico del mindfulness ha aumentado en los últimos años, y la Mindful Attention Awareness Scale (MAAS) se ha convertido en uno de los instrumentos más empleados para su medida. El objetivo de esta investigación fue analizar la eficacia del entrenamiento en mindfulness y las propiedades psicométricas de las puntuaciones de la MAAS en una muestra clínica mediante el modelo de Rasch.
MétodosSe seleccionaron 199 sujetos con sintomatología ansioso-depresiva. El grupo experimental (n=103) recibió un entrenamiento grupal en mindfulness y el grupo control (n=96) un tratamiento ambulatorio convencional con la misma duración. Se analizaron las puntuaciones pre y pos en la MAAS para valorar la eficacia del entrenamiento, las propiedades psicométricas de las puntuaciones y el funcionamiento diferencial de los ítems (DIF) usando el Modelo de Escalas de Calificación (MEC).
ResultadosLos ítems 9 y 12 desajustaron, el ítem 9 mostró DIF, y se observaron problemas de traducción al castellano en los ítems 5, 9 y 12. Se decide repetir el análisis eliminándolos. Los resultados de la versión reducida MAAS-12 mostraron valores adecuados en dimensionalidad, ajuste y fiabilidad.
ConclusionesContrariamente a los resultados de otros trabajos, la MAAS fue sensible al cambio producido por el entrenamiento. La versión habitualmente empleada presenta problemas métricos y de traducción y debe revisarse. La escala MAAS-12 es métricamente mejor que la habitualmente empleada, pero adolece de infrarrepresentación del constructo. Se recomienda construir instrumentos desde una perspectiva teórica coherente, de modo que todas las facetas del atributo se vean representadas.
Mindfulness is the term typically used to denote a highly adaptive psychological strategy that helps to decrease anxiety and increase well-being in people who practice it.1 Studies of its clinical applications have significantly increased in recent years despite there still not being a clear definition of the construct or knowledge of the underlying mechanisms involved.2
It is described as the ability to maintain awareness in the present moment, leaving behind all the recurrent and automatic thoughts that do not relate to the here and now. Under this definition, it usually alludes to 4 fundamental elements: (1) awareness of one's own experience, including bodily sensations, thoughts and emotions, as well as external events, images or sounds present,3 (2) sustained attention to these things, (3) centring oneself in the present moment, and (4) acceptance without criticism.4–6 Although these qualities of mindfulness are inherent in all human beings, many studies agree that we can be trained to potentiate its beneficial effects, through either formal (daily body checks, seated or moving meditation, etc.) or informal exercises (eating, showering or driving with full awareness).7
There are several therapeutic interventions, based on mindfulness, that have been shown to be effective for different psychiatric disorders.4,8–16 However, the failure to arrive at a consensus in definition, as well as the lack of widely accepted instruments for measurements (for example, see the case dedicated to this question in the magazine Psychological Inquiry, 2007, vol. 18, 4), have created obstacles in launching tests for these types of interventions.17,18 Furthermore, whether it is really mindfulness that explains the results obtained is still being debated.19 Recent meta-analyses seem to conclude that mindfulness training can help to improve the physical and psychological symptoms of different psychiatric disorders, reduce stress and improve general health in the people affected.20,21
In the field of constructing instruments for measurement, important efforts have been made in recent years in attempts to measure the levels of this construct in people.22–26 The problem has been that each instrument has been constructed using a different definition of mindfulness, with positions that range from those who choose to define it with 1 dimension to those that use 5.26,27 These disparities have brought up the question of whether these instruments are really measuring the same thing.28
One of the instruments generating the most interest is the Mindful Attention Awareness Scale (MAAS).29 This self-report questionnaire was constructed based on cognitive theory and considers mindfulness to be defined using a single dimension: attention-awareness of the present moment. The MAAS is a simple scale and quickly applied, with 15 items that evaluate an individual's general ability to be attentive to and aware of the present moment of his or her daily life. Correlations have been found between scores on this scale and cerebral activity,30 the results of the interventions based on mindfulness,31 and specific32 and general33 benefits of meditation.
Analyses of the original version, using the Classical Test Theory (CTT), show acceptable psychometric properties, and the scale has been adapted to other languages,34,35 including Spanish.36 Given that the MAAS is 1 of the most used tools in literature to assess mindfulness,37–39 it is relevant to analyse the functioning and psychometric properties of its Spanish version using sophisticated psychometric models based on Item Response Theory (IRT), specifically the Rasch model, due to its potential advantages under the CTT analysis.40–42
Due to increasing clinical use of treatment programmes based on mindfulness, it has become pertinent to analyse the functioning of the MAAS in clinical populations, as scientific evaluation of treatments is not possible without appropriate measurements. Therefore, our objective was to perform a Rasch analysis of the psychometric properties of MAAS scores obtained in a clinical sample within the context of studying the effectiveness of mindfulness training.
MethodsParticipantsFirst, 199 subjects with anxious-depressive symptomatology were selected from the mental health area of Badajoz.
Inclusion criteria for study participants were as follows: aged between 18 and 70 years, anxious and/or depressive symptomatology and verbal commitment to attending at least 90% of the group sessions in mindfulness training (for the experimental group) or attending 6 biweekly reviews with his or her referral psychiatrist or psychologist (for the control group). The latter is a timeline equivalent to the duration of the Mindfulness-Based Stress Reduction (MBSR) programme, from Stahl and Goldstein.7 Criteria for exclusion were as follows: acute phase psychiatric illness, or with psychotic symptoms, diagnosis of a psychotic disorder or mental retardation, sensory deficits or language difficulties that did not allow for test completion and, finally, lack of verbal commitment to attending the individual reviews or therapy sessions.
InstrumentsThe Spanish version of the MAAS was used.36 This consisted of 15 items that could be scored with a Likert scale of 1 (almost always) to 6 (almost never) and was presented as a quantitative assessment of a subject's state of mindfulness during his or her daily life. To complete the questionnaire, it was not necessary for the subjects to have previously had specific training. The final score was an arithmetic measurement of the scores given for the items; higher scores would indicate a higher state of mindfulness.
ProcedureCandidates were selected by the mental health teams and from the eating disorder unit, following the inclusion–exclusion criteria previously agreed upon. Diagnostic evaluation of the participants was carried out through a structured clinical interview for mental disorders on Axis 1 of the DSM-IV (SCID-1).43 After a primary selection process, candidates were individually interviewed and informed on the objectives and conditions of the study. Participation was voluntary, without economic incentives, and the information collected was confidential.
The experimental group received group training on mindfulness throughout 12 sessions, 1 per week, lasting 90min, based on a group-adaptation of the MBSR programme.7 Groups were formed by order of participant registration; the highest number of participants in a group was 12. The control group received conventional outpatient treatment throughout 6 review sessions (1 session every 15 days) with their referral psychiatrist or psychologist. The psychiatry reviews consisted of adjustments in drug treatment; the psychology reviews included cognitive-behavioural interventions without mindfulness training. Both the experimental and control groups received treatment for 12 weeks.
The pre-test was carried out individually during the selection interview and after the participant signed his or her informed consent. The post-test was done in a group format in the last therapy session for the experimental group, or during the sixth individual review for the control group.
Data analysisThe variables collected were as follows: sex, age, principal and secondary psychiatric diagnoses (if present), absence or presence of drug treatment, group assignment (experimental or control) and pre and post scores on the MAAS.
First, a factorial ANOVA was performed using the difference between the MAAS scores in the pre- and post-test as the dependent variable (DV), and group assignment (experimental or control) and the absence or presence of drug treatment as the independent variables (IV). This initial assessment of the effectiveness of mindfulness training with direct scores (sum of values from the 15 items) was presented to allow comparison with international studies that use the typical MAAS scoring system.
However, given that the conclusions of any study are conditioned by the measurement adequacy of the instrument, we continued with a psychometric analysis of the scores using the Rasch model (WINSTEPS44 software). This allowed for the joint measurement of people and items, in the same latent variable, with interval properties, including advantages making the software particularly recommendable.45 Due to the instrument's characteristics, we used an extension of the model for polytomous items, the Rating Scale Model (RSM),46 which allowed us to empirically analyse the measurement quality of the response categories. Subsequent to the study of quality of category, the adjustment of the data to the assumption of unidimensionality was analysed using principal component analysis of the residuals. It can be affirmed that the data are essentially one-dimensional if the Rasch measurement realises a moderately high percentage variance (at least 20% in the opinion of Reckase47) and the individual score of the first residuals component is less than 2.44
In addition to quantifying the adjustment of the model items (using infit and outfit statistics), an analysis of its differential functioning (DIF) was carried out, associated with group assignment (experimental or control). This was done to rule out that possible latent factors unrelated to the construct measured were influencing the measurement. In order to detect the DIF, procedures derived from the Rasch and Mantel-Haenszel models were used. The criterion used to consider DIF as present was that the items showed DIF under both the Rasch perspective (significant difference and more than half a logit between the difficulty parameters in both groups) and the Mantel-Haenszel method (type C DIF: delta MH value is greater than 1.5 and is significant). Under both the Rasch contrast and the MH method, the Bonferroni correction was used for the significance level.48
Finally, the ANOVA was repeated, but this time using the differential Rasch score on the MAAS between the pre and post measurements on the logit scale as the DV. Calculating this differential score was justified if the localisation parameters of the items were invariant; that is to say, the order of severity of the items had to be similar in both measurements (which can be verified using the Pearson correlation between the parameters of difficulty for the items in both occasions).
ResultsThe experimental group was composed of 103 subjects (74 women and 29 men) between the ages of 18 and 62 years (mean of 42.35 and standard deviation of 12.40). The control group consisted of 96 subjects (72 women and 24 men) between the ages of 18 and 70 years (mean of 40.5 and standard deviation of 13.07).
The results from the first factorial ANOVA were as follows: F(3,195)=141.54; P<.01, which indicates that only group assignment had significant effects on the differential score on the MAAS, F(1,195)=310.72; P<.01. There were no significant effects found in the drug treatment variable, F(1,195)=1.52; P>.01, or in the interaction variable, F(1,195)=0.20; P>.01.
Regarding the psychometric analysis of the MAAS, testing the adequacy of the response categories using the RSM showed that the Likert scale functioned appropriately both in the pre- and post-test, which agreed with the Linacre49 criteria. The data deviated slightly from unidimensionality, given that the value of the first residuals component was higher than 2, both in the pre- (2.4) and post-test (2.1), despite the fact that the percentage variance explained by the Rasch measurement was sufficiently high in the pre-test (40.7) and the post-test (50.9). This revealed the probable existence of a second dimension.
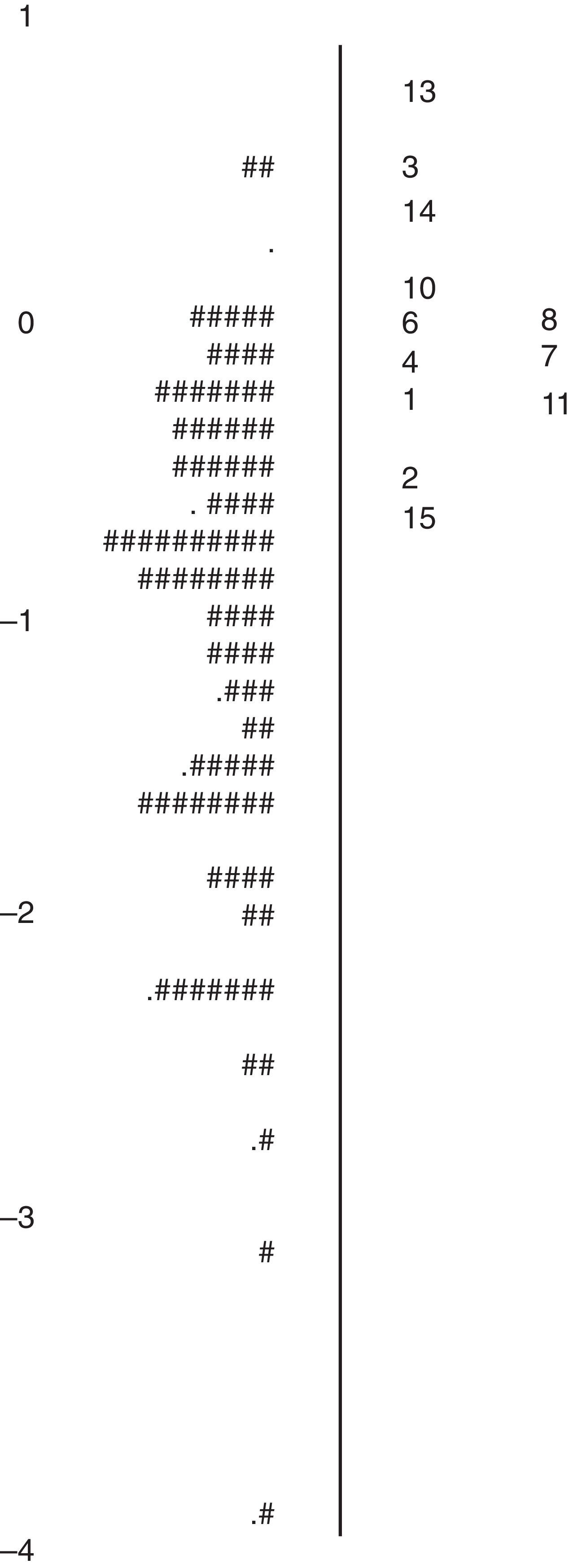
In both applications, the greater part of the items on the MAAS-15 adjusted to the model, except in the case of item 9, which presented moderate imbalance in the pre-test and severe imbalance in the post-test; as well as item 12, which showed moderate imbalance in the pre-test. Table 1 shows the localisation, associated standard error and adjustment statistics for each of the items on the MAAS in the pre- and post-test. The inadequacy of item 9 was also shown in the DIF analysis associated with group assignment, given that its severity parameter differed significantly in 1.04 logit between the control group and experimental group in the pre-test, and in 2.62 logit in the post-test.
Psychometric values from the 15 items on the MAAS in the pre- and post-test.
| Psychometric values from the 15 items on the MAAS | |||||||||
| Item number | Content | Pre-test | Post-test | ||||||
| Level of difficulty (in logit units) | Standard error | Infit | Outfit | Level of difficulty (in logit units) | Standard error | Infit | Outfit | ||
| 1 | I could be experiencing some emotion and not be conscious of it until some time later | −0.04 | 0.06 | 0.85 | 0.80 | −0.12 | 0.07 | 0.87 | 0.87 |
| 2 | I break or spill things because of carelessness, not paying attention, or thinking of something else | −0.35 | 0.06 | 1.00 | 1.06 | −0.31 | 0.07 | 0.87 | 0.87 |
| 3 | I find it difficult to stay focused on what's happening in the present | 0.56 | 0.08 | 0.86 | 0.86 | 0.36 | 0.08 | 0.62 | 0.62 |
| 4 | I tend to walk quickly to get where I’m going without paying attention to what I experience along the way | 0.04 | 0.07 | 1.07 | 0.99 | 0.33 | 0.08 | 1.15 | 1.15 |
| 5 | I tend not to notice feelings of physical tension or discomfort until they really grab my attention | 0.20 | 0.07 | 0.89 | 0.87 | 0.13 | 0.07 | 0.80 | 0.80 |
| 6 | I forget a person's name almost as soon as I’ve been told it for the first time | 0.08 | 0.07 | 1.12 | 1.00 | 0.29 | 0.07 | 1.12 | 1.12 |
| 7 | It seems I am “running on automatic,” without much awareness of what I’m doing | 0.06 | 0.07 | 1.10 | 1.10 | −0.05 | 0.07 | 0.96 | 0.97 |
| 8 | I rush through activities without being really attentive to them | 0.17 | 0.07 | 0.66 | 0.62 | 0.21 | 0.07 | 0.61 | 0.61 |
| 9 | I get so focused on the goal I want to achieve that I lose touch with what I’m doing right now to get there | −1.42 | 0.06 | 1.72a | 1.92a | −1.42 | 0.08 | 2.74a | 2.89a |
| 10 | I do jobs or tasks automatically, without being aware of what I’m doing | 0.22 | 0.07 | 0.55 | 0.52 | 0.13 | 0.07 | 0.59 | 0.59 |
| 11 | I find myself listening to someone with one ear, doing something else at the same time | −0.09 | 0.06 | 0.96 | 1.00 | 0.22 | 0.07 | 0.96 | 0.95 |
| 12 | I drive places on ‘automatic pilot’ and then wonder why I went there | −0.28 | 0.06 | 1.65a | 1.63a | −0.29 | 0.07 | 1.51a | 1.49a |
| 13 | I find myself absorbed in the future or the past | 0.81 | 0.09 | 0.83 | 0.74 | 0.58 | 0.08 | 0.61 | 0.60 |
| 14 | I find myself doing things without paying attention | 0.50 | 0.08 | 0.64 | 0.65 | 0.44 | 0.08 | 0.64 | 0.65 |
| 15 | I snack on foods without being aware that I’m eating | −0.46 | 0.06 | 1.06 | 0.99 | −0.65 | 0.07 | 1.12 | 1.09 |
Finally, the estimations of the subjects were precise, with indexes of overall reliability (Person Separation Index, whose interpretation is analogous to that of Cronbach's alpha) of 0.73 in the pre-test and 0.89 on the post-test.
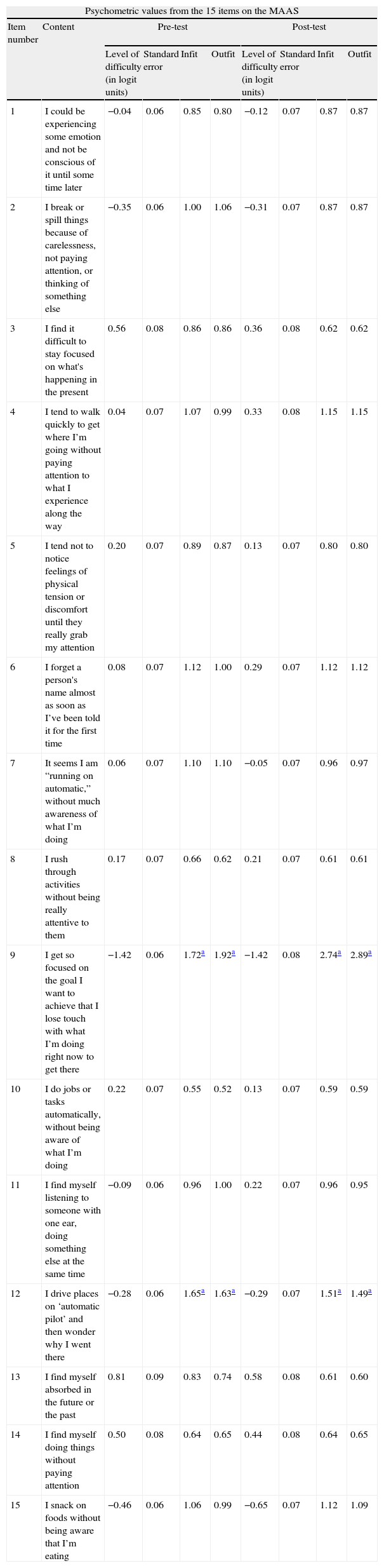
Due to the adjustment problems with items 9 and 12, as well as the presence of DIF in item 9, we opted to calibrate the MAAS by eliminating them. Item 9 (“I get so focused on the goal I want to achieve that I lose touch with what I am doing right now to get there.”) showed an imbalance in both the pre- and post-test. In addition, the translation of this item seemed abstract in relation to the original in English, and its content did not seem essential given its redundancy with other items on the MAAS. In the case of item 12 (“I drive places on “automatic pilot” and then wonder why I went there.”), whose adjustment was less than desired, the Spanish translation was inadequate; it should say: “I go places on autopilot and then wonder why I went there.” The term “drive” also means “direct oneself”, thus making it probable that the authors of the original version intended to imply the more general meaning, while the translation reflected a specific one.
In addition, we decided to forego item 5 (“I tend not to notice feelings of physical tension or discomfort until they really grab my attention.”) because of its semantic ambiguity. In Spanish, you cannot notice something that has not really grabbed your attention: that is what noticing something means. In English, “really” is an emphatic term and the verb “to grab” implies more intensity than captar (“attract” in Spanish), which means the sensation had to be very strong to successfully attract the subject's attention. This nuance is lost in the Spanish translation.
In the calibration using the 12-item RSM version (MAAS-12), the response categories from the Likert scale again worked adequately in both the pre- and post-test. Regarding the unidimensionality of the MAAS-12, the percentage variance explained by the Rasch measurement was 38.2% in the pre-test and 56.6% in the post-test. In addition, the value from the first residuals component was low in both the pre- (1.9) and post-test (1.8). Therefore, the unidimensionality hypothesis for the data is acceptable. Lastly, no DIF associated with group assignment was found in the pre- and post-measurements.
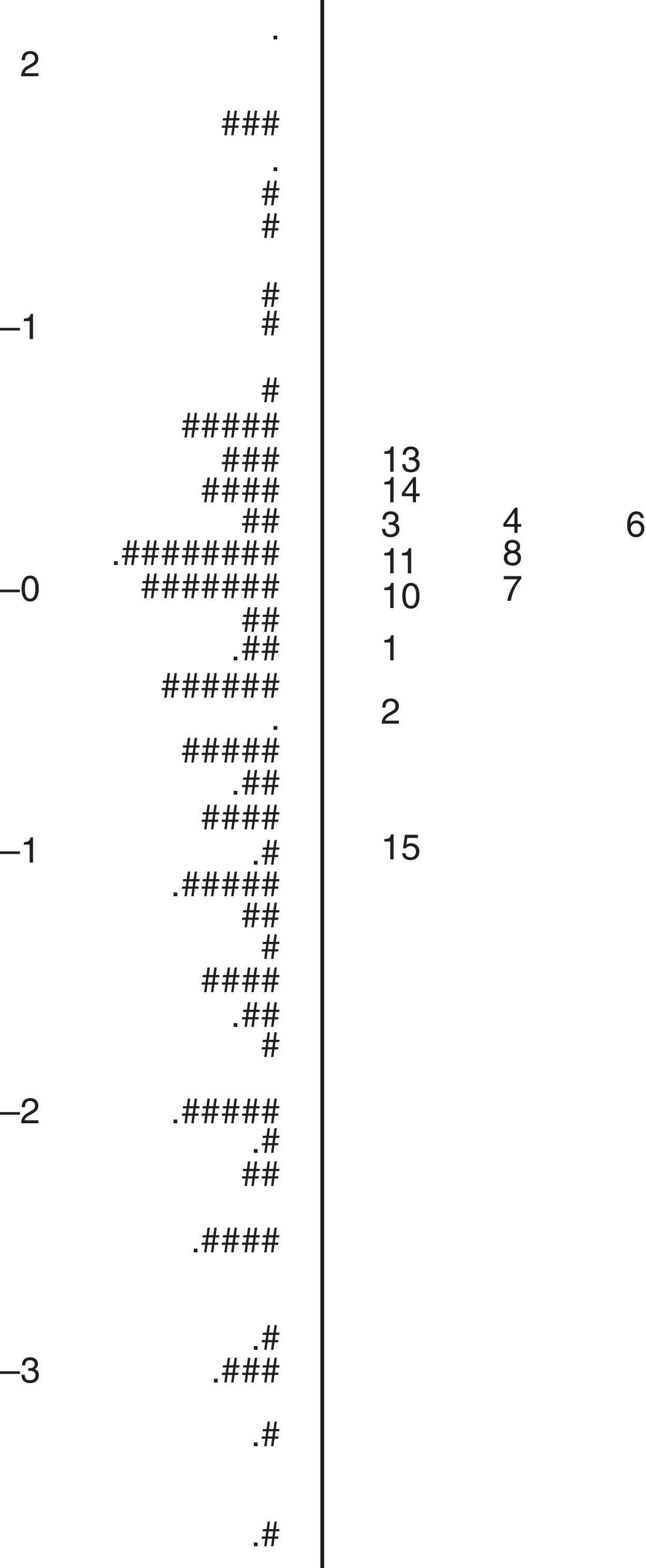
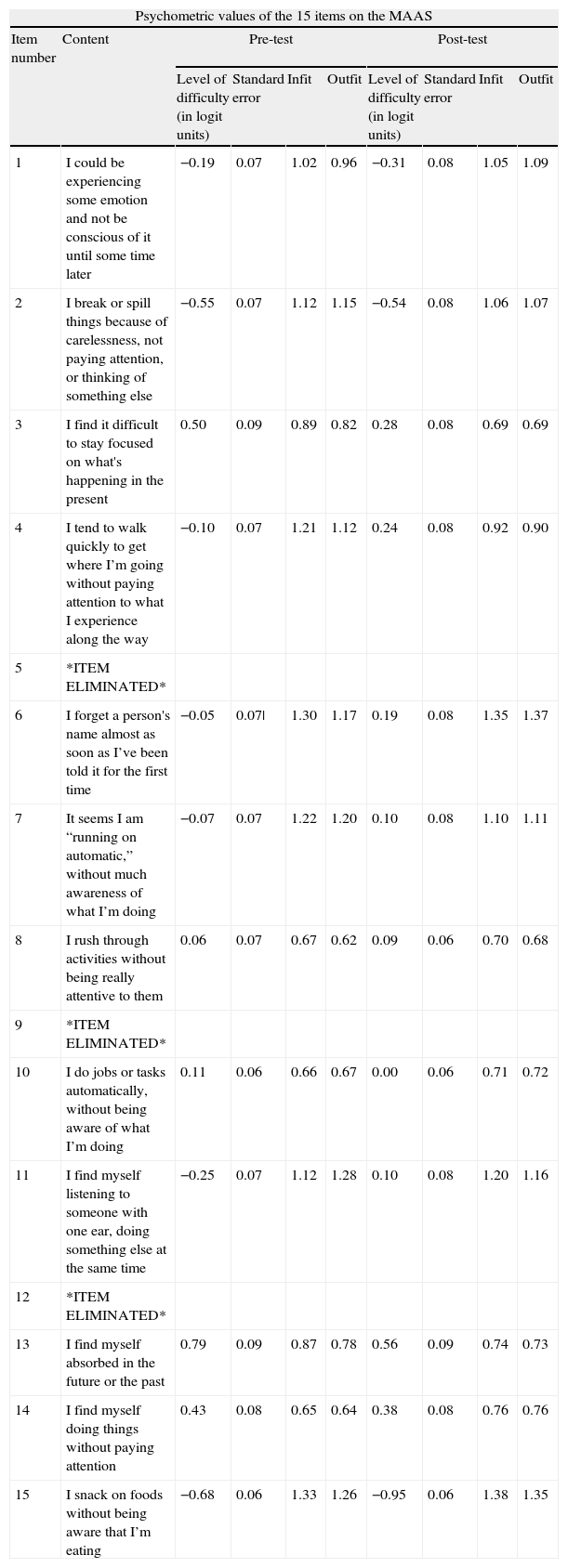
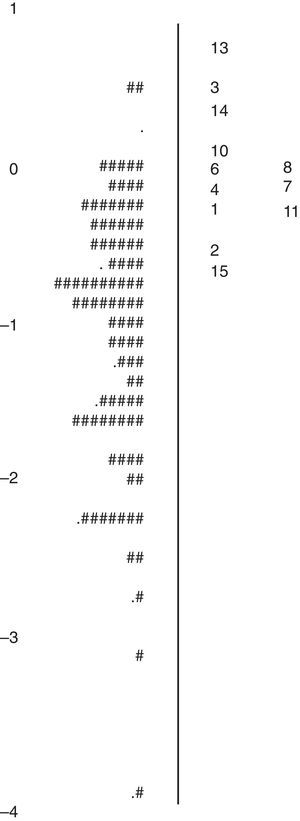
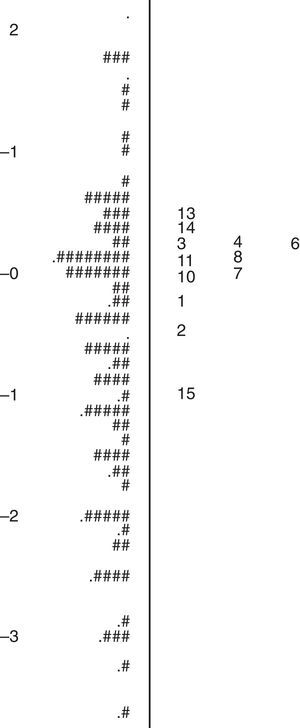
In this case, all the items presented adequate adjustment to the model (see Table 2). Figs. 1 and 2 present the plots of the placement of the 12 items and the 199 subjects along the variable in the pre- and post-test. The estimations of the subjects were reliable, and they even improved slightly with respect to the 15-item version. The overall reliability indexes (Person Separation Index) were 0.79 in the pre-test and 0.90 in the post-test.
Psychometric values of the items on the MAAS-12 in the pre- and post-test once items 5, 9 and 12 had been eliminated.
| Psychometric values of the 15 items on the MAAS | |||||||||
| Item number | Content | Pre-test | Post-test | ||||||
| Level of difficulty (in logit units) | Standard error | Infit | Outfit | Level of difficulty (in logit units) | Standard error | Infit | Outfit | ||
| 1 | I could be experiencing some emotion and not be conscious of it until some time later | −0.19 | 0.07 | 1.02 | 0.96 | −0.31 | 0.08 | 1.05 | 1.09 |
| 2 | I break or spill things because of carelessness, not paying attention, or thinking of something else | −0.55 | 0.07 | 1.12 | 1.15 | −0.54 | 0.08 | 1.06 | 1.07 |
| 3 | I find it difficult to stay focused on what's happening in the present | 0.50 | 0.09 | 0.89 | 0.82 | 0.28 | 0.08 | 0.69 | 0.69 |
| 4 | I tend to walk quickly to get where I’m going without paying attention to what I experience along the way | −0.10 | 0.07 | 1.21 | 1.12 | 0.24 | 0.08 | 0.92 | 0.90 |
| 5 | *ITEM ELIMINATED* | ||||||||
| 6 | I forget a person's name almost as soon as I’ve been told it for the first time | −0.05 | 0.07| | 1.30 | 1.17 | 0.19 | 0.08 | 1.35 | 1.37 |
| 7 | It seems I am “running on automatic,” without much awareness of what I’m doing | −0.07 | 0.07 | 1.22 | 1.20 | 0.10 | 0.08 | 1.10 | 1.11 |
| 8 | I rush through activities without being really attentive to them | 0.06 | 0.07 | 0.67 | 0.62 | 0.09 | 0.06 | 0.70 | 0.68 |
| 9 | *ITEM ELIMINATED* | ||||||||
| 10 | I do jobs or tasks automatically, without being aware of what I’m doing | 0.11 | 0.06 | 0.66 | 0.67 | 0.00 | 0.06 | 0.71 | 0.72 |
| 11 | I find myself listening to someone with one ear, doing something else at the same time | −0.25 | 0.07 | 1.12 | 1.28 | 0.10 | 0.08 | 1.20 | 1.16 |
| 12 | *ITEM ELIMINATED* | ||||||||
| 13 | I find myself absorbed in the future or the past | 0.79 | 0.09 | 0.87 | 0.78 | 0.56 | 0.09 | 0.74 | 0.73 |
| 14 | I find myself doing things without paying attention | 0.43 | 0.08 | 0.65 | 0.64 | 0.38 | 0.08 | 0.76 | 0.76 |
| 15 | I snack on foods without being aware that I’m eating | −0.68 | 0.06 | 1.33 | 1.26 | −0.95 | 0.06 | 1.38 | 1.35 |
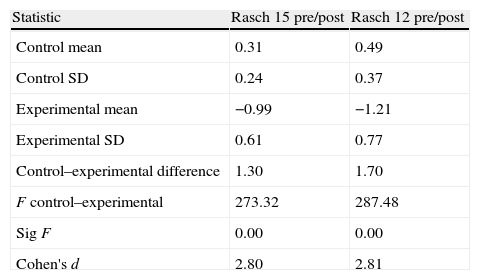
The ANOVA results destined for analysing the effectiveness of the mindfulness training with Rasch scores (pre/post differential) can be seen in Table 3. Both measurements were justified because the order of the severity parameters was similar in the pre- and post-test, as well as in the MAAS-15 (r=0.95) and MAAS-12 (r=0.87).
Results from the ANOVA to analyse the effectiveness of mindfulness training with pre/post differential Rasch scores on the MAAS-15 and the MAAS-12.
| Statistic | Rasch 15 pre/post | Rasch 12 pre/post |
| Control mean | 0.31 | 0.49 |
| Control SD | 0.24 | 0.37 |
| Experimental mean | −0.99 | −1.21 |
| Experimental SD | 0.61 | 0.77 |
| Control–experimental difference | 1.30 | 1.70 |
| F control–experimental | 273.32 | 287.48 |
| Sig F | 0.00 | 0.00 |
| Cohen's d | 2.80 | 2.81 |
SD: standard deviation; Sig: significance.
Based on the results obtained in this study and in others,37,38 the MAAS turned out to be a tool sensitive to change in a Spanish clinical population, able to detect significant improvements in subjects’ ability to be attentive to and aware of the present moment in subjects that underwent mindfulness group training with the MBSR programme. In addition, these changes were independent of the effects of using psychoactive drugs, even though our results are limited in this regard by the fact that no dosage or type of drug was considered.
Our results differed from those obtained in the Spanish MAAS validation study,36 where the authors suggested that the instrument might possibly be insensitive to change, and where these results are especially relevant to the use of the instrument in clinical contexts. Future studies should analyse the implications of mindfulness training in the improvement of clinical symptoms, including other clinical scales. Such studies should also attend to the influence of comorbidity with other psychiatric disorders.
Problems with the Spanish version of the Mindful Attention Awareness ScaleRegarding the results obtained with the Spanish version of the MAAS, adjustment and translation issues with items 5, 9 and 12 led us to suggest that an in-depth review of the instrument would be necessary. In relation to items 8, 10 and 14, which presented low adjustment values, albeit within acceptable limits, they seemed to contain redundant and very general content. They speak of “activities”, “jobs”, “chores”, “things”, which yields certain dependence. However, as van Dam et al.50 suggests, it could be precisely those items that are so general that measure better on the MAAS. In any case, of the 3, item 14 uses the most typical Spanish expression in its translation, thus making the other 2 non-essential.
The results obtained with the MAAS-12 for dimensionality, item adjustment and score reliability suggest that this reduced version is more recommended than the one typically used. However, as shown in the following section, it is necessary to construct instruments from a coherent theoretical perspective, in a way that all the facets of each construct are represented.
Construct validity and dimensionality of the Mindful Attention Awareness ScaleThe authors of the MAAS defined the construct from a one-dimensional perspective, only focusing on characteristics referring to the ability to be fully aware of the present moment. However, as some authors2 have recently suggested, at least 4 abilities seem to be necessary for there to be mindfulness: (1) be fully aware of the internal and external events that occur, (2) have sustained attention, avoiding possible distractions to your awareness, (3) focus on the present moment and (4) accept anything that happens without criticism. These elements would operate reciprocally and interdependently to produce the beneficial results of mindfulness and the training has been shown to have important implications for psychological well-being. Some authors have indicated that the underlying mechanism that explains these effects would be the improvement produced in the ability to self-regulate; that is to say, the ability to reduce (or de-automate) negative cognitions and emotional reactions that would otherwise be automatic.2
In any case, clearly defining the construct to which we are referring is the priority, before addressing the task of constructing appropriate measurement instruments.17 If we define mindfulness from a set of 4 integrated abilities (awareness, attention, focus on the present moment and acceptance), the MAAS would not adequately reflect all the characteristics of the construct, given that its items do not directly allude to acceptance of the present moment without criticism. In this sense, the very authors of the MAAS excluded acceptance in constructing the instrument, considering it functionally redundant.29 However, clinical work suggests that focusing on the present moment does not necessarily mean accepting it. For example, a patient with depressive symptoms may engage in destructive brooding regarding his or her present situation, focusing on it but not accepting it. In this case, it is the act of not accepting the present moment that generates the symptoms of anguish and sadness. On the other hand, in our study, the maximum percentage of variance shown by the MAAS was 56.6% in the post-test, after training the subjects of the experimental group in tasks specifically related to the items on the scale. This leads us to consider that measurement would improve if new facets were included on the scale, in the direction demonstrated in other instruments.26 Dimensionality analysis of the test scores constructed in this way will make it possible to decide whether a scale is enough (in the event that there is essential unidimensionality) or if several scales are necessary to adequately represent the construct.
In conclusion, future studies should take the essential elements of mindfulness into consideration with the goal of creating better measurements and developing clinical treatment programmes whose effectiveness could be adequately evaluated, something that is not possible to do when such measurements are of low psychometric quality.
Ethical disclosuresHuman and animal protectionThe authors declare that the procedures followed conformed to the ethical standards of the committee for responsible human experimentation and are in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that they followed the protocols of their work centre regarding publication of patient data, and that all patients included in the study received sufficient information and gave their written informed consent to participate in said study.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects mentioned in the article. This document is in possession of the corresponding author.
Conflict of interestsThe authors have no conflicts of interests to declare.
Please cite this article as: Inchausti F, Prieto G, Delgado AR. Análisis Rasch de la versión española de la escala Mindful Attention Awareness Scale en una muestra clínica. Rev Psiquiatr Salud Ment (Barc.). 2014;7:32–41.