The Neuropsychiatric Inventory (NPI) is a scale that assesses psychiatric symptoms in patients with neurological disorders, principally dementia. Despite its advantages, there are few published studies in traumatic brain injury (TBI) patients. With the NPI information we are going to describe the psychopathologic disorders in a group of TBI chronic patients and look for the possible association with psychiatric history and outcome measures.
MethodThe NPI was applied to caregivers of 53 patients with severe TBI in chronic phase. We also collected functional and community integration scales.
Results92.5% of patients had some neuropsychiatric symptoms, according to NPI. The most frequent were irritability/lability, apathy and depression/dysphoria. Those patients with drugs abuse history had more psychiatric symptoms. Presence of agitation/aggression, apathy and disinhibition were correlated with more disabilities.
ConclusionsPsychiatric disorders are common among patients with TBI. The NPI is a scale that systematically assesses the behavioural and emotional disorders more common in these patients. Some of the symptoms negatively influence the degree of disability.
El Inventario Neuropsiquiátrico es una escala que valora la presencia de alteraciones psicopatológicas en pacientes con enfermedades neurológicas, principalmente demencias. A pesar de sus ventajas, existen pocos estudios publicado en pacientes con traumatismo craneoencefálico (TCE). Con la información derivada del NPI pretendemos describir las alteraciones psicopatológicas en un grupo de pacientes con TCE severo en fase crónica y determinar si se correlacionan con antecedentes psiquiátricos y medidas de resultado.
MétodoSe administró el NPI a los informantes de 53 pacientes con traumatismo craneoencefálico grave que se encontraban en fase crónica. Así mismo, se recogieron escalas de funcionalidad y de integración a la comunidad.
ResultadosEl 92.5% de la muestra estudiada presentaba alguna alteración psicopatológica según el NPI, siendo los síntomas más frecuentes la irritabilidad/labilidad, la apatía y la depresión/disforia. El antecedente de consumo habitual de tóxicos mostró una relación significativa con la presencia de psicopatología. Síntomas como la agitación, la apatía y la desinhibición se correlacionaron de forma significativa con el grado de discapacidad.
ConclusionesLas alteraciones psiquiátricas son frecuentes en pacientes con TCE. El Inventario neuropsiquiátrico es una herramienta que recoge de manera sistemática las alteraciones conductuales y emocionales más frecuentes en estos pacientes. Algunos de los síntomas influyen negativamente en el grado de discapacidad.
The illnesses called “organic brain syndromes” have been explored very little in psychiatry at the end of the 20th century. The contemporary approach to these syndromes has been developed with models and “cognitive” language. Consequently, in descriptions of dementia, stroke and other brain illnesses, there are many references to disturbances in subtypes of memory, attention or executive functions. Furthermore, psychopathological descriptions are rare. These disturbances are very prevalent however, and they have a considerable impact on the patients’ social integration as well as the quality of life of their families and caretakers.1
Neuropsychiatry has become aware of this reality and thus has multiplied its efforts over the last 2 decades to develop instruments that help to characterise and measure the psychopathological disturbances in organic brain syndromes. In this sense, the Neuropsychiatric Inventory (NPI) by Cummings et al.2 has likely been the most successful scale. It was initially designed to detect neuropsychiatric symptoms in patients with Alzheimer's disease and other forms of dementia.3 Its use has since been extended to pathologies such as strokes,4–7 multiple sclerosis,8,9 Huntington's disease, Tourette's syndrome and other movement disorders.10–12
Despite its advantages, only 3 studies have been published where the NPI was administered to assess neuropsychiatric disturbances in patients with a traumatic brain injury (TBI).13–15 There were also 2 more that assessed the efficiency of pharmacological treatments in this population.16,17
Compared to other scales that may be used for the same purpose – such as the Neurobehavioural Rating Scale,18 the Frontal Systems Behavioural Scale19 and the Iowa Rating Scales of Personality Change (IRSPC)20 – the NPI has an advantage because its application is simple and its dissemination in literature has been wide. In the Spanish population, the NPI was validated by Vilalta et al.21
ObjectiveUsing information from the NPI, the main objective of this study was to describe the psychopathological disturbances presented by a group of patients in the chronic phase of severe TBI. In addition to this main objective, other aspects would also be evaluated: the relationship between neuropsychiatric disturbances and history of habitual drug and alcohol consumption; the relationship between neuropsychiatric disturbances and global measures of results from scales such as the Glasgow Outcome Scale (GOS) and the Disability Rating Scale (DRS); and finally, the relationship between the NPI results and the degree of social integration measured by the Community Integration Questionnaire (CIQ).
The first of these secondary objectives sought to assess whether or not a history of drug and alcohol consumption influenced the neuropsychiatric pathology present in patients with traumatic brain injury. The second helped to elucidate whether or not the presence of neuropsychiatric disturbances negatively influenced the functional prognosis in the long term. The third analysed the impact of psychopathological disturbances on social integration.
MethodsPatientsThe sample was composed of a consecutive series of patients older than 18 years with a history of severe traumatic brain injury. These patients completed rehabilitative treatment during the subacute phase in the brain injury unit at the Guttmann Institute. These patients also agreed to a follow-up for periodic medical review throughout 2010. The phase was considered chronic 2 years from the time of injury. All participants scored lower than 4 for the mobility item on the Functional Independence Measure (FIM) scale and thus were able to walk independently.
The annual review programme in the brain injury unit included a multidisciplinary assessment, in which global measures of functionality were collected. These included the GOS and DRS, as well as community integration measures such as the CIQ. In addition, a psychiatric interview was performed with a family member or informant, to administer the NPI.
InstrumentsA data collection sheet was drafted for this study, with sociodemographic information about the patients and variables concerning the injury: age, sex, aetiology of the injury, TBI severity according to the Glasgow Coma Scale and initial findings in neuroimaging. Likewise, the patients’ psychiatric and toxicological histories were documented to determine whether or not their substance consumption was habitual. Habitual consumption was considered 1 or 2 times per week, in accordance with the definition from the National Drug Plan.22
- -
Neuropsychiatric Inventory (NPI)2: This instrument allows information to be obtained concerning psychopathology in patients with brain disorders. It includes 12 items (Table 1) and is designed to be completed by a professional on the basis of a semistructured interview. Each item acts as an initial filtering question that identifies whether the symptom was present in the last month. In the case of an affirmative response, the interview follows a series of additional questions that allow information to be obtained concerning the frequency or severity of the symptom. The score for each item is calculated by multiplying the frequency by the intensity; and the total score for the NPI is calculated by adding the scores of all symptoms. Thus, scores may range from 0 to a maximum of 144, where the higher the score, the more severe the psychopathology.
Table 1.Summary table for NPI scores.
Symptom Not assessable Frequency Severity Total (frequency×severity) Delirium 01234 123 Hallucinations 01234 123 Agitation/aggression 01234 123 Depression/dysphoria 01234 123 Anxiety 01234 123 Joy/euphoria 01234 123 Apathy 01234 123 Disinhibition 01234 123 Irritability/lability 01234 123 Abnormal motor behaviour 01234 123 Sleep disorders 01234 123 Eating disorders 01234 123 Total score - -
Glasgow Outcome Scale (GOS)23: This scale is a global measurement of outcome in terms of functionality after a traumatic brain injury. It uses 5 categories: death, vegetative state (unable to act reciprocally with the environment), severe disability (able to follow orders, unable to live independently), moderate disability (able to live independently, unable to return to work or studies) and good recovery (able to return to work or studies).
- -
Disability Rating Scale (DRS)24: This instrument assesses functional recovery in patients with moderate and severe traumatic brain injuries from the point of the coma to their return to the community, taking cognitive function into consideration.25
It assesses 5 categories:
- 1
Waking, consciousness and ability to respond
- 2
Cognitive capacity for self-care activities
- 3
Dependency on others
- 4
Psychosocial adaptation
The score can range from 0 (where no disability is present) to 29 (the maximum level of dependency, corresponding to the clinical situation of a vegetative state).
- -
Community Integration Questionnaire (CIQ)26: This social integration questionnaire was designed to evaluate patients’ integration into the community after a traumatic brain injury. It consists of 15 questions distributed over 3 subscales:
Competency at home: Evaluates autonomy in daily life activities, participation in domestic chores, in finances and in planning social activities.
Social integration: Evaluates activities during leisure time, with family members, with friends and short trips away from their homes.
Productive activities: Evaluates employment status, training and volunteer activities.
The score can range from 0, corresponding to severe impairment, to 25, indicating no impairment.
Statistical analysisThe type of data collected was diverse. For the continuous variables, basic descriptive statistics were presented, such as measurements of central tendency (mean, median) and measurements of distribution (standard deviation, interquartile range, maximum and minimum values). In addition, the Kolmogorov–Smirnov test was performed to identify whether or not the variable followed a normal distribution. The categorical variables were summarised by frequencies and percentages of appearance in each condition of the sample.
Comparisons between groups were performed with parametric (t-test) and non-parametric (Mann–Whitney) tests, as appropriate.
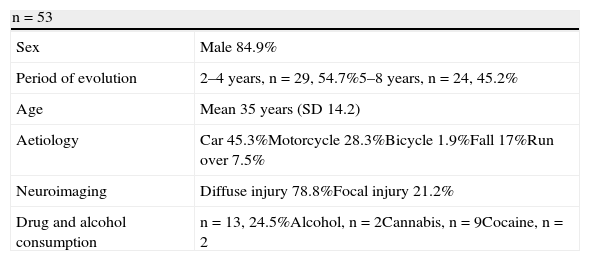
ResultsThe final sample was composed of 53 patients with severe traumatic brain injury, according to the Glasgow Coma Scale, who were between 2 and 8 years of evolution. Of the total, 84.9% were male and the mean age was 35 years (range, 17–69). Of the total, 58.5% were 31 years or younger.
The aetiology of the TBI in order of frequency was as follows: car accident (45.3%), motorcycle accident (28.3%), fall (17%), being run over (7.5%) and bicycle accident (1.9%).
The neuroimaging tests revealed a diffuse injury affecting 2 or more areas of the brain in 78.8% of the cases, and a focal injury in 21.2%.
Only 1 patient (1.9%) had a pre-existing psychiatric pathology (major depression), whilst 13 (24.5%) consumed drugs and alcohol habitually. Cannabis was the substance most consumed, followed by alcohol and cocaine (see Table 2.)
Sample characteristics.
| n=53 | |
| Sex | Male 84.9% |
| Period of evolution | 2–4 years, n=29, 54.7%5–8 years, n=24, 45.2% |
| Age | Mean 35 years (SD 14.2) |
| Aetiology | Car 45.3%Motorcycle 28.3%Bicycle 1.9%Fall 17%Run over 7.5% |
| Neuroimaging | Diffuse injury 78.8%Focal injury 21.2% |
| Drug and alcohol consumption | n=13, 24.5%Alcohol, n=2Cannabis, n=9Cocaine, n=2 |
At the moment of assessment, 28 patients were receiving psychopharmaceuticals for behaviour or emotion control. Of these, 14 were taking antidepressants, 12 antiepileptics, 4 atypical antipsychotics, 3 dopaminergics, 3 benzodiazepines and 2 non-benzodiazepine hypnotics.
NPI resultsOf the total sample, 92.5% presented some psychiatric symptoms according to the NPI, with a mean score of 9.83 (SD 9.17). Only 3 patients out of the 53 studied were free of any psychopathology.
The prevalence data for symptoms are shown in Table 3. More than half of the patients scored on the irritability–lability item (53%), almost half on the apathy item (49%) and 43% on the depression–dysphoria item. These 3 items targeted emotional disorders with their corresponding behavioural manifestation. Behaviours including disproportionate anger, abrupt mood changes, uncontrollable emotions or laughter, decrease in initiative, mitigation of emotional expression or indifference were extraordinarily prevalent. Anxiety was present in 28% of the cases.
Neuropsychiatric disturbances according to the NPI.
| No. of patients | % of patients | |
| Irritability/lability | 30 | 56.6 |
| Apathy | 26 | 49 |
| Depression/dysphoria | 23 | 43.4 |
| Disinhibition | 17 | 32.1 |
| Eating disorders | 17 | 32.1 |
| Anxiety | 15 | 28.3 |
| Sleep disorders | 12 | 22.6 |
| Agitation/aggression | 10 | 18.9 |
| Joy/euphoria | 5 | 9.4 |
| Delirium | 3 | 5.6 |
| Abnormal motor behaviour | 0 | 0 |
| Hallucinations | 0 | 0 |
Verbal, motor or instinctive disinhibition was also frequent (32%). The high frequency of changed eating patterns (32%) referenced by family members stood out. This did not consist of eating disorders such as bulimia or anorexia, but rather changes in speed or in the way patients ate their food, increases and decreases in the quantity ingested and changes in food preferences after the injury.
Sleep disturbances (22%) mainly consisted of insomnia and waking several times throughout the night, with no nocturnal behaviour changes related to dementia. Aggression (19%) was also referenced by informants as self-limited reactive episodes in response to an unpleasant stimulus, or frustration in response to a negative stimulus.
Reactions of persistent and structured delirium or euphoria were not very frequent, being found in less than 10% of the patients. Delirious ideas were present in only 3 patients, all of them with an evolution between 2 and 4 years. No cases were observed with hallucinations or abnormal motor behaviour.
No significant correlation was identified between the injury type (focal or diffuse) and the presence of neuropsychiatric disturbances (P=.645).
To study the “effect” of the period of evolution, the sample was divided into 2 groups: 1 group included patients between 2 and 4 years after their injury (29 patients) and the other, patients between 5 and 8 years (24 patients). Both groups were comparable concerning age and sex. No differences were observed in the total scores or in the individual analysis of each symptom on the NPI (P=.597) (see Figure 1).
Habitual consumption of drugs and alcohol showed a significant correlation with presence of psychopathology. The total score for the consuming group was higher (P=.05). The agitation–aggression (P=.026) and disinhibition (P=.04) items were responsible for this difference. The apathy subscale was close to significance (P=.07).
We found a statistically significant correlation between the presence of psychopathology (as measured with the NPI scale) and treatment with psychopharmaceuticals (P=.008).
Impairment and neuropsychiatric symptomsAccording to the GOS scale, impairment was severe in 5 patients (9.4%) and moderate in 30 cases (56.6%), whilst 18 patients (34%) had good recovery (able to return to work or studies). Similar results were obtained with the Disability Rating Scale: 13% of patients had severe impairment, 60% between partial and moderate impairment and 26% had no impairment.
The presence of agitation and disinhibition was significantly correlated with the degree of impairment measured by the GOS scale (P=.041 and .035, respectively). Apathy was correlated with the DRS-rated degree of impairment (P=.04).
Community integration and neuropsychiatric symptomsThe community integration questionnaire was given to 39 of the 53 patients in the sample (73.6%). Of these patients, 30.8% had a score showing a slight impact on community integration, 41% a moderate impact, 2.6% severe and 25.6% showed no impact.
Competence at home was not impacted in 41% of the cases, and impact was slight or moderate in 33.4%. This may have been due to the fact that the sample consisted of patients with autonomous mobility.
Something similar occurred with the social integration variable. This variable showed no impact in 46.2% of the cases, and the impact was slight or moderate in 51.3%.
In contrast, productive activity was very severely impacted in 53.8% of the cases and severely in 20.5%.
Community integration did not show a correlation with the presence of neuropsychiatric disturbances or the period of evolution. In addition, those patients with a history of alcohol and drug consumption did not show worse community integration according to the CIQ scale (P=.66).
DiscussionWe present a group of 53 patients in the chronic phase of serious TBI and with good physical functionality, of which 92.5% showed some psychopathological disturbance.
The disorders detected with the NPI coincided with the habitual reasons for consultation from the caretakers of these patients, such as irritability, apathy, changes in mood with depression or euphoria and disinhibition. The symptoms assessed using the 12 items on the NPI contributed to the global scores in a very differentiated way.
The mean scores in our sample were all higher than those reported in healthy controls.4,9 In symptoms such as apathy, changes in diet and depression–dysphoria, the scores were similar to those described in a group of 51 patients with moderate and severe TBI that were between their first and second year of evolution.13 The scores obtained in disinhibition, irritability–lability, agitation–aggression and insomnia were lower in our sample, which may have been due to the fact that these symptoms are more frequent in earlier stages of the injury. In addition, our results may also reflect the availability of pharmacological treatments effective in controlling these symptoms.
A common finding of the NPI was the presence of diet changes and eating disorders. These disturbances—which often go unnoticed in the clinical environment—were not the reason for consultation on the part of family members, except when the disorder was very severe, or generated disruptive behaviour or significant changes in weight.
Eating disorders seem to be a frequent disturbance, though rarely diagnosed, in patients with different neurological pathologies such as TBI,13 stroke,4 multiple sclerosis8 and Alzheimer's disease,27 with figures between 1.3% and 2.12% compared to 0.24% for the general population.4,9
In this sample, delirious ideals were infrequent and there were no cases that showed hallucinations or abnormal motor behaviour. Therefore, the characteristic psychopathology of acute psychosis was not present in our patients in the chronic phase of TBI.
A relevant finding was that psychiatric disturbances persisted in patients with traumatic brain injuries until the eighth year of the injury. Comparing the frequency of symptoms according to the period of evolution (2–4 years vs 5–8 years), we did not observe any mitigation of the symptoms over time.
In patients with a history of habitual drug and alcohol consumption, both the total score on the NPI scale and that on the agitation–aggression and disinhibition items were significantly higher.
It should be pointed out that symptoms such as agitation–aggression, disinhibition and apathy negatively influenced the degree of impairment measured by the GOS and DRS scales.
Productive activity was the aspect most affected in community integration in our sample, as competence at home and social integration mainly demonstrated a slight or moderate affectation. In patients with neuropsychiatric disturbances and with a history of drug and alcohol consumption, worse community integration was not observed.
An important variable that was not included in this study, despite it being a known predictive factor, was the duration of post-traumatic amnesia (PTA). Data on this variable were not collected because it did not appear in a significant percentage of the cases. Data regarding the frequency or intensity of each separate symptom on the NPI were not collected either, nor the overburden on the caretaker. The latter variable could have contributed valuable information, considering the direct repercussions that different symptoms could have had for the caretakers.
ConclusionThe NPI is a useful tool that systematically gathers the most frequent behavioural and emotional symptoms in patients with TBI, some of which correspond with the organic personality disorder, such as irritability–lability, apathy, depression–dysphoria and disinhibition. Other less recognised symptoms in these patients include sleep and diet disturbances; these should be included in evaluations, given their elevated frequency.
Psychopathological disturbances in patients with traumatic brain injuries are very prevalent and tend to persist years after the injury. A history of drug and alcohol consumption maintained a relationship with the presence of disinhibition and aggression, whilst other variables such as time passed after the injury or the type of injury (focal or diffuse) did not influence the presence of psychopathological disturbances.
Symptoms such as agitation–aggression, disinhibition and apathy negatively influenced the degree of impairment in patients, measured by the GOS and DRS scales. This emphasises the importance of diagnosing and treating these symptoms in a timely manner.
Ethical responsibilitiesProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors declare that in this article there is no data of patients.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Castaño Monsalve B, et al. Perfil psicopatológico de pacientes con traumatismo craneoencefálico evaluados mediante el Inventario Neuropsiquiátrico. Rev Psiquiatr Salud Ment (Barc). 2012;5:160–6.