Oestrogens have been hypothesized to have a protective effect in psychotic disorders. Women with schizophrenia have a later age of menarche, fewer pregnancies and earlier age of menopause. However, little information is available focusing on delusional disorder (DD). We aimed to evaluate gynaecological variables and psychopathology, and rates of gynaecological service use in female DD outpatients.
MethodsFourty-six outpatients with DD (DSM-IV-TR) were attended at the Hospital Clinic of Barcelona, from 2008 to 2013. Demographic and clinical variables, as well as gynaecological features were recorded in 25 women with DD. Hamilton Rating Scale for Depression-17 for depression, Positive and Negative Syndrome Scale for psychopathology, Personal and Social Performance for functionality, and Columbia Suicide Severity Rating Scale were assessed.
ResultsMean age of menarche (SD) was 12.83(1.54) years, mean age of menopause 48.73(2.69), mean age at onset of DD was 48.70(13.03). 48% of the sample did not receive gynaecological attention in the last 2–3 years. No statistically significant correlations were found between age at menopause and age at onset of DD. Age at menopause showed a tendency to be negatively correlated with Personal and Social Performance total scores (r=−0.431; P=.074), and was positively associated with suicidal ideation intensity (r=0.541; P=.038). However, after controlling for social support variables, this relationship was no longer significant.
ConclusionsAlthough a small sample size, this is the first study to specifically examine gynaecological variables in DD. Low compliance rates in gynaecological service use were found. No correlations between age at menopause and clinical variables were statistically significant.
Se ha formulado la hipótesis de que los estrógenos confieren un efecto protector en los trastornos psicóticos. En las mujeres con esquizofrenia se evidencia una edad de la menarquia más tardía, menos embarazos y una edad más temprana de la menopausia. Sin embargo, hay poca información disponible centrada en mujeres con trastorno delirante (TD). El objetivo del presente estudio fue evaluar las variables ginecológicas y la psicopatología, al igual que el uso de servicios ginecológicos en casos ambulatorios de mujeres con TD.
MétodosEntre 2008 y 2013, en el Hospital Clínic de Barcelona fueron atendidos 46 pacientes con TD (DSM-IV-TR). Se registraron las variables demográficas y clínicas, al igual que las ginecológicas en 25 mujeres con TD. Se administraron las escalas clínicas siguientes: Hamilton de 17 ítems para depresión, escala de evaluación de síntomas negativos y positivos para psicopatología, escala de funcionamiento personal y social para funcionalidad y escala Columbia de evaluación de la severidad suicida.
ResultadosLa edad media (DE) de la menarquia fue de 12,83 (1,54) años, la edad media de la menopausia fue de 48,73 (2,69), y la edad media de inicio del trastorno fue de 48,70 (13,03) años. El 48% de los pacientes de la muestra no había recibido atención ginecológica en los 2-3 últimos años. No se encontraron correlaciones estadísticamente significativas entre la edad de la menopausia y la edad de inicio del trastorno. La edad de la menopausia mostró una tendencia a correlacionarse negativamente con las puntuaciones obtenidas en la escala de funcionamiento personal y social total (r=−0,431; p=0,074), y se asoció positivamente con la intensidad de la ideación suicida (r=0,541; p=0,038). Sin embargo, tras un ajuste para las variables de apoyo social, esta relación dejó de ser significativa.
ConclusionesA pesar del reducido tamaño muestral, el presente estudio es la primera investigación que examina específicamente las variables ginecológicas en el TD. Se encontró una reducida tasa de asistencia en el uso de los servicios ginecológicos. No se encontraron correlaciones estadísticamente significativas entre la edad de la menopausia y otras variables clínicas.
During decades, special attention has been paid to epidemiological and clinical observations about the gender differences in the psychopathology of schizophrenic psychosis. Seeman and Lang (in 1990)1 were the first ones to specifically revise the role of oestrogens in schizophrenia.
Besides, the existence of gender differences related to age at the moment of the beginning of the disease in patients with schizophrenia is well established. In women, a second peak of incidence during menopause is observed, which is associated with an increase of the seriousness of psychopathology and resistance to treatment.2
A hypothesis has been formulated that oestrogens confer a protector effect to women with risk of schizophrenia,3 which has been confirmed with epidemiological and clinical studies carried out in animals.4–6 In the last years, in randomized and controlled trials, it has been investigated the possible antipsychotic effect of oestrogens in the treatment of women who suffer from psychosis, considering that the results have been promising.2 On the other hand, many clinicians have also described that in some women suffering from schizophrenia, chronic signs of hypogonadism and hypostrogenism7 are observed, such as late age of menarche, less pregnancies and deliveries, and earlier age at the moment of menopause, in comparison with healthy women. Nevertheless, it is necessary to take into consideration other aspects in the study of the mentioned hormonal hypofunction. The typical and atypical antipsychotics can induce hyperprolactinaemia, which is associated with infertility in both genders.8
Different published studies suggest that gynaecological problems are the most frequent pathology referred by women with schizophrenia.7 However, only 10% of these alterations have been previously diagnosed.9 Lindamer et al.9 conducted a cross-sectional study in a sample of 65 elderly women with schizophrenia and 51 women without psychiatric diagnosis. In comparison with the control group, the women with schizophrenia received less quantity of gynaecological services and patients showed lower rates of substitute hormonal treatment.
Although in the delusional disorder (DD) gender differences are an undeniable fact,10 the role of oestrogens and reproductive variables has still to be explained on the clinical course and psychopathology of women with DD. No study has specifically investigated the reproductive variables and infertility in a clinical sample of patients with DD. Besides, the utilization rates of gynaecological services among these patients have not been previously investigated either.
We set out the hypothesis of the existence of a relation between the age at the beginning of menopause, the age at the beginning of the disease and the psychopathological symptoms of DD. Moreover, we noticed that women with DD might show lower rates of attendance to their gynaecological visits.
The present study had two main objectives:
- (1)
To assess the gynaecological variables such as mean age of menarche, mean age of menopause and its relation with psychopathology in women with DD.
- (2)
To investigate the utilization rates of gynaecological services in outpatients with DD.
We selected all the consecutive cases of female outpatients with DD assisted in the Psychiatric Service of the Hospital Clínic from Barcelona in a first psychiatry visit, between January 2008 and March 2013.
Patients who complied with the following inclusion criteria were included: (1) Female, (2) age>18 years, (3) DD diagnosis according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), (4) clinical stability, and (5) current antipsychotic treatment for over 6 months. Exclusion criteria were the following: (1) previous schizophrenia diagnosis, schizophrenic disorder, affective disorder or mental retardation, and (2) psychosis clearly due to an organic brain disease or substance abuse.
Study designIn a retrospective design, we conducted a cross-sectional study on demographic and clinical data, and gynaecological variables in outpatients with DD. All patients were systematically assessed through a detailed semistructured interview and by 2 psychiatrists. The adviser responsible for the case also confirmed the DD diagnosis.
The following main socio-demographic and clinical factors were registered: age, age of beginning of DD, marital status, level of education, and employment situation, number of children and other family members, and antipsychotic treatment. We also registered characteristics related to oestrogens, such as age at the moment of menarche, age at menopause, use of contraceptives (currently and throughout life), pattern of menstrual period (duration and regularity of cycles), gynaecological disorders, number of pregnancies, number of abortions and utilization rates of gynaecological service. In clinical practice, the next assessment instruments were used: Hamilton Rating Scale for Depression (HRSD-17), Positive and Negative Syndrome Scale (PANSS) for psychopathology, Personal and Social Performance (PSP) scale for functionality and Columbia Suicide Severity Rating Scale (CC-SSRS).
Statistical analysisThe statistical analysis was conducted using the SPSS statistical programme for Windows (version 19). A descriptive analysis was carried out using average and standard deviation for continuous variables, and percentages for categorical variables. The relation between the age of the beginning of DD, age of menopause and ratings of the psychopathological assessment was made with bivariate correlation coefficients. In a second stage, partial correlation coefficients were used with the number of family members and children as main social factors of confusion. The significance level was established at 0.05 (2 queues).
ResultsSample descriptionOut of 46 outpatients assisted at our Psychiatry Service, 37 (82.22%) were women, and gynaecological variables were obtained from 25 of them.
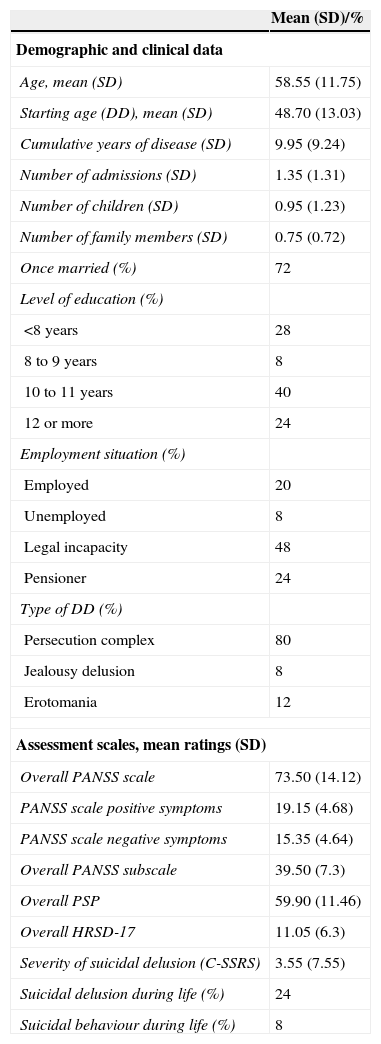
In Table 1, demographic and clinical characteristics of the total sample are shown.
Demographic and clinical data, and ratings obtained in the assessment scales (n=25).
| Mean (SD)/% | |
|---|---|
| Demographic and clinical data | |
| Age, mean (SD) | 58.55 (11.75) |
| Starting age (DD), mean (SD) | 48.70 (13.03) |
| Cumulative years of disease (SD) | 9.95 (9.24) |
| Number of admissions (SD) | 1.35 (1.31) |
| Number of children (SD) | 0.95 (1.23) |
| Number of family members (SD) | 0.75 (0.72) |
| Once married (%) | 72 |
| Level of education (%) | |
| <8 years | 28 |
| 8 to 9 years | 8 |
| 10 to 11 years | 40 |
| 12 or more | 24 |
| Employment situation (%) | |
| Employed | 20 |
| Unemployed | 8 |
| Legal incapacity | 48 |
| Pensioner | 24 |
| Type of DD (%) | |
| Persecution complex | 80 |
| Jealousy delusion | 8 |
| Erotomania | 12 |
| Assessment scales, mean ratings (SD) | |
| Overall PANSS scale | 73.50 (14.12) |
| PANSS scale positive symptoms | 19.15 (4.68) |
| PANSS scale negative symptoms | 15.35 (4.64) |
| Overall PANSS subscale | 39.50 (7.3) |
| Overall PSP | 59.90 (11.46) |
| Overall HRSD-17 | 11.05 (6.3) |
| Severity of suicidal delusion (C-SSRS) | 3.55 (7.55) |
| Suicidal delusion during life (%) | 24 |
| Suicidal behaviour during life (%) | 8 |
C-SSRS: Columbia Suicide Severity Rating Scale; SD: standard deviation; HRSD: Hamilton Rating Scale for Depression; PANSS: Positive and Negative Syndrome Scale; PSP: Personal and Social Performance Scale; DD: delusional disorder.
The mean age of beginning of DD was 48.70 (13.03) years. The most frequent DD type was the persecution complex (80%), followed by erotomania (12%). 24% of the patients of the sample mentioned suicidal delusion throughout their lives, whereas 8% showed suicidal behaviour.
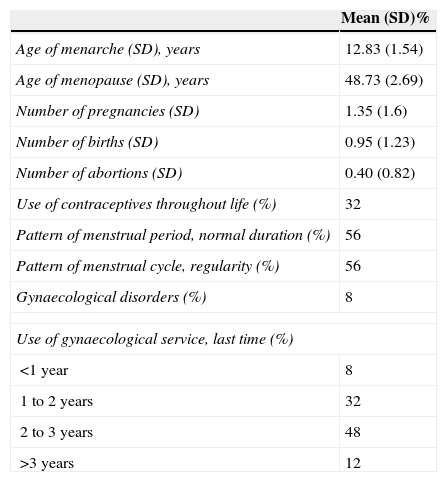
When we pay attention to reproductive and gynaecological variables, the average age of menopause was of 48.73 (2.69) years, and 8% had experienced gynaecological disorders throughout their lives.
Psychopathological assessment of total sampleIn Table 1, psychotic and depressive symptoms, social and personal functioning and severity of suicidal delusion are shown.
Gynaecological variables and use of gynaecological service in total sampleIn Table 2, the mean and standard deviation of continuous gynaecological variables and assistance rates to the gynaecological service are shown in percentages. 48% of outpatients with DD did not visit gynaecological services during 2–3 years.
Gynaecological variables and use of gynaecological service (n=25).
| Mean (SD)% | |
|---|---|
| Age of menarche (SD), years | 12.83 (1.54) |
| Age of menopause (SD), years | 48.73 (2.69) |
| Number of pregnancies (SD) | 1.35 (1.6) |
| Number of births (SD) | 0.95 (1.23) |
| Number of abortions (SD) | 0.40 (0.82) |
| Use of contraceptives throughout life (%) | 32 |
| Pattern of menstrual period, normal duration (%) | 56 |
| Pattern of menstrual cycle, regularity (%) | 56 |
| Gynaecological disorders (%) | 8 |
| Use of gynaecological service, last time (%) | |
| <1 year | 8 |
| 1 to 2 years | 32 |
| 2 to 3 years | 48 |
| >3 years | 12 |
In the overall sample, a reduced assistance rate to the gynaecological service was found.
Analysis of the correlations between age at the moment of menopause, age at the beginning of the delusional disorder and psychopathologyNo statistically significant correlations were found between age of beginning of menopause and age of beginning of DD. Although it was not statistically significant, the age of beginning of menopause showed a trend to negatively correlate with total ratings obtained in the PSP scale (r=−0.431; p=0.074).
Besides, the age of menopause was positively associated with intensity of suicidal delusion (r=0.541; p=0.038). Nevertheless, when in the correlation analysis the mean variables of social support were included, such as number of children and other family members, the age of beginning of menopause stopped relating with the intensity of suicidal delusion.
DiscussionA cross-sectional study was performed in which we included 25 female outpatients with DD. According to our knowledge, the present study is the first research to specifically examine the related reproductive features and the rates of assistance to gynaecological visits in a clinical group of women with delusional disorder. Nevertheless, it is necessary to consider some limitations of the present study, such as the absence of a healthy control group. The design of the present study was retrospective, which could determine a bias of memory, and the size of the sample was small, which has limited the possibility to apply more complex statistical analysis. No statistically significant correlations were found between the age of beginning of menopause and the age of beginning of the disease. However, the findings of the present study should be cautiously interpreted due to the difficulty to determine the age of menopause in women treated with antipsychotics. When it was not corrected for the confusion factors, the age of beginning of menopause was positively related to the severity of the suicidal delusion in the sample of the present study. After the adjustment for the number of children and other family members, no statistically significant correlations were found. For this reason, the absence of a main social network could have influenced the results of the present study.
No statistically significant correlations were found between the age at the moment of menopause and psychopathological symptoms assessed through clinical scales. These findings contrast with the previously published studies about schizophrenia; therefore, additional studies on a broad scale are required to clarify in a better way the role of menopause in psychopathology of women with DD.
A reduced rate of compliance with the gynaecological service visits was found, suggesting it is necessary to direct women with DD to that service. The findings of the present study match with previous studies carried out in the field of schizophrenia.9
Ethical responsibilitiesProtection of people and animalsAuthors state that no experiments were performed on human beings or animals as part of this investigation.
Data confidentialityAuthors state they have followed the protocols of their workplace about the data publication of patients and that all the patients included in the study have received enough information and have given their written informed consent to participate in that study.
Right to privacy and informed consentAuthors have obtained the informed consent from the patients and/or subjects referred to in the article. This document is in possession of the corresponding author.
FundingThe present investigation was partly funded through a scholarship granted to Rosa Catalán from the Health Research Fund (Fondo de Investigaciones Sanitarias, FIS:EC040209).
Conflict of interestDr Alexandre González-Rodríguez has received a research scholarship (Premi Emili Letang) of the Hospital Clínic from Barcelona. Dr. Miquel Bernardo has received fees from Bristol-Meyer-Squibb and Wyeth, Janssen-Cilag, Eli Lilly, Pfizer, Synthelab, Glaxo Smith Kline and Astra-Zeneca, but they are not related to the content of this manuscript. The remaining authors have not declared any conflict of interest.
We want to express our acknowledgement to the Government of Catalonia, Comissionat per Universitats i Recerca del Departament d’Innovació, Universitats i Empresa (DIUE) 2009SGR1295 and to the Institute of Health Carlos III, Mental Health Biomedical Research Networking Centres (Centro de Investigación Biomédica en Red de Salud Mental, CIBERSAM) and all the staff for their help filling in the demographic and clinical data of medical records. Research was (partly) carried out at the Esther Koplowitz Centre, in Barcelona.
Please cite this article as: González-Rodríguez A, Molina-Andreu O, Penadés Rubio R, Catalán Campos R, Bernardo Arroyo M. Variables reproductivas y uso de consulta ginecológica en pacientes con trastorno delirante. Rev Psiquiatr Salud Ment (Barc.). 2015;8:92–96.