Comorbidity between depression and physical illnesses is very common and has a significant impact on the health and management of the patient. With the support of the Sociedades Españolas de Psiquiatría y Psiquiatría Biológica and Sociedad Española de Médicos de Atención Primaria (SEMERGEN) a consensus was prepared on physical health in patients with depression and it is summarised in the present work. The literature review highlighted the high frequency of cardiovascular and endocrine–metabolic disorders in patients with depression such as diabetes and obesity, thus making the primary and secondary prevention recommendations for patients with cardiovascular or metabolic risk applicable to patients with depression. Comorbidity between depression and chronic pain is also frequent, and requires an integrated therapeutic approach. The presence of physical illness in patients with depression may condition, but not preclude, the pharmacological treatment; drug selection should take into account potential side effect and drug–drug interactions. On the other hand, psychotherapy may contribute to the patient's recovery. Overall, coordination between the primary care physician, the psychiatrist and other health professionals involved is essential for the management of patients with depression and concomitant physical illness.
La comorbilidad entre depresión y enfermedades físicas es muy frecuente y tiene un impacto importante en el deterioro de la salud así como en la atención y tratamiento recibidos. Impulsado por las Sociedades Españolas de Psiquiatría y Psiquiatría Biológica, y la Sociedad Española de Médicos de Atención Primaria (SEMERGEN) se realizó un consenso sobre la salud física en el paciente con depresión, que de forma resumida se expone en el presente trabajo. La revisión de la literatura puso de manifiesto la elevada frecuencia en pacientes con depresión de trastornos cardiovasculares y trastornos endocrinometabólicos como la obesidad y la diabetes, de tal modo que en pacientes con depresión serían aplicables las recomendaciones de prevención primaria y secundaria establecidas para los individuos con riesgo cardiovascular o metabólico. También es frecuente la comorbilidad entre depresión y dolor crónico, que obliga a la detección activa de ambos trastornos y a una intervención terapéutica integral. La presencia de esta comorbilidad puede condicionar, aunque no impedir el tratamiento farmacológico en cuya elección se deberá tener en cuenta los efectos secundarios y las interacciones de los distintos antidepresivos. Por su parte, la psicoterapia puede contribuir a la recuperación integral del enfermo. Globalmente, en el proceso de atención al paciente con depresión y enfermedades físicas comórbidas es fundamental la coordinación del médico de atención primaria, el psiquiatra y otros especialistas o profesionales implicados.
In Spain majority of depression is because of the most frequently occuring mental disorder, with a prevalence/year of 4% in the general population.1,2 Depression is linked to a significant degree of disability. In the world population, neuropsychiatric illnesses constitute 28% of the disability-adjusted life years, and unipolar affective disorder contributes an important percentage of this (10%).3 Even subclinical depression is associated with significant deterioration in health.4 It is estimated that the burden of this illness, including the risk of suicide, will continue increasing in the coming years.5
As will be indicated later in this article, depression and medical illnesses are very frequently comorbid and this association is bidirectional, so depression may be the cause or the consequence of these 2 conditions.6 The possible mediators of this relationship range from biological factors (for example, immune, neuroendocrine or inflammatory) to specific life styles (i.e., a sedentary lifestyle or inadequate diet). In addition, there are common determining factors that could increase the risk that depression and medical comorbidity will appear. Socioeconomic level, psychosocial problems, childhood traumas, certain psychological features or genetic characteristics are found among such factors.7
Regardless of the direction of the relationship between depression and medical illnesses, the effect of such comorbidity is impactful. When depression presents together with other physical illnesses, the reduction in health is greater than that of only depression or isolated physical illnesses and even than that of chronic physical illnesses combined without depression. The presence of this comorbidity makes looking for help and diagnosing more difficult, and affects the quality of the care received as well as the treatment and adherence to it; it also affects the results of treatment of physical illnesses negatively, including an increase in disease-related mortality.7
Spanish psychiatrists are becoming ever more interested in the physical health of the patient with mental disorders.8–10 The project presented in this article was promoted by the Sociedades Españolas de Psiquiatría and Psiquiatría Biológica (Spanish Societies of Psychiatry and Biological Psychiatry) and the Sociedad Española de Médicos de Atención Primaria (Spanish Society of Primary Care Physicians) (SEMERGEN); the objective was to achieve consensus on physical health in the patient with depression. Consequently, a literature review was carried out and experts met to establish final Decalogue of recommendations on prevention, diagnosis and intervention in medical diseases associated with depression. By disseminating this Decalogue, it is hoped that treatment and health care quality will improve for patients with depression and associated medical comorbidity in our environment.
Materials and methodsThis consensus document has been backed by the Sociedad Española de Psiquiatría, Sociedad Española de Psiquiatría Biológica and Sociedad Española de Médicos de Atención Primaria, with the participation of the Fundación Española de Psiquiatría y Salud Mental (Spanish Foundation of Psychiatry and Mental Health). For its preparation, the societies that participated, through their representatives (JB, JG, JSR, FL and EZB), proposed and formed a multidisciplinary Scientific Committee; this was constituted by 6 psychiatrists, 5 primary care physicians, a pharmacologist and a psychologist. The Scientific Committee then selected a group of 25 experts, specialists in psychiatry (13), primary care (10) and research epidemiology/methodology (2). The participating psychiatrists and primary care physicians were chosen based on their experience and interest in the physical health of patients with a mental disorder and in mental disorders, respectively.
Review of the specialised literatureTo help to prepare the consensus document, a review of the specialised medical literature related to depression as a risk factor in the development of different physical illnesses was carried out.
The reference search was performed using the Medline database and included studies published through May 2011. To be included in the review, the criteria were: studies that were longitudinal, comparative and assessed the role of depression in the development of medical comorbidity.
Multidisciplinary consensus meetingsUsing the literature review performed as a base, the experts evaluated the impact of depression and associated medical comorbidity, the possible pathogenic mechanisms that explain such comorbidity and the implications there might be in diagnostic and therapeutic behaviour with these patients. With this information, the Scientific Committee established a series of recommendations to improve the health care quality for the patients with depression and medical diseases. These were presented to the task force in a multidisciplinary consensus meeting, during which work groups were organised to discuss the evidence and recommendations presented by the Scientific Committee. In the plenary session closing the meeting, the work groups presented their conclusions, which were debated with the rest of the participants and incorporated into a first draft of the consensus document.
In a second meeting, the Scientific Committee discussed the first draft of the consensus document, which they summarised in a Decalogue. This guide was reviewed again by the task force, and their commentaries were incorporated by the Scientific Committee in the final version. This article summarises the review carried out by the Scientific Committee that was used as the basis for establishing the final conclusions, which are presented as a Decalogue of recommendations.
ResultsMedical diseases and associated depressionThe prevalence of depression in patients with medical illnesses is greater than in the general population, reaching overall percentages higher than 20%.11 This elevated prevalence can be explained, at least in part, by the secondary effects of some treatments or by the negative effect that the disability associated with some illnesses has on the state of mind. The physiopathology of some medical illnesses can also play a role in the development of depression, as is found with some neuroendocrine or autoimmune disorders.12 All of this would explain the increase in the risk of depression observed in patients with medical illnesses, especially those that suffer chronic processes such as diabetes, cancer and osteoarthritis.13–15
Depression in patients with medical illnesses strongly affects the worsening of the prognosis of the associated somatic illness, as has been seen in metabolic, cardiovascular and neurological illnesses.12 In addition, depression negatively affects treatment adherence, functional capacity and the patient's quality of life. All of this means that, many times, hospital stay and the use of other health resources increase, which translates into an increase in health cost.12
In the context of primary health care, depression is underdiagnosed. Some studies in our environment indicate that only 20% of patients with major depression are identified as such in the primary care setting.16 The fact that psychological symptoms are omitted from normal examinations, that there is a lack of resources for taking a complete case history and that a stigma is often associated with depression, as well as that depressive symptoms overlap with specific medical disorders, complicates diagnosing depression in primary care.12
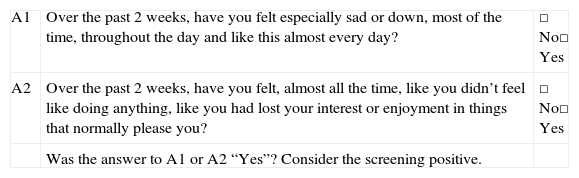
To improve the identification of depression in primary care, it would be a good idea to carry out a screening of depression adapted to the resources and time available in this setting. To do so, the task force proposes a brief 2-question survey based on the Mini-International Neuropsychiatric Interview (MINI), which explores the 2 main symptoms of depression (Table 1). A positive result in either of these could be considered enough for a high degree of suspicion of depression. In severe chronic illnesses, such as cancer or degenerative neurological diseases, the importance of monitoring the risk of suicide as well is emphasised.12 The appearance of new classification systems, such as the CIE-11, can also contribute to greater detection of depression in primary care.17
Depression screening questionnaire.
| A1 | Over the past 2 weeks, have you felt especially sad or down, most of the time, throughout the day and like this almost every day? | □ No□ Yes |
| A2 | Over the past 2 weeks, have you felt, almost all the time, like you didn’t feel like doing anything, like you had lost your interest or enjoyment in things that normally please you? | □ No□ Yes |
| Was the answer to A1 or A2 “Yes”? Consider the screening positive. |
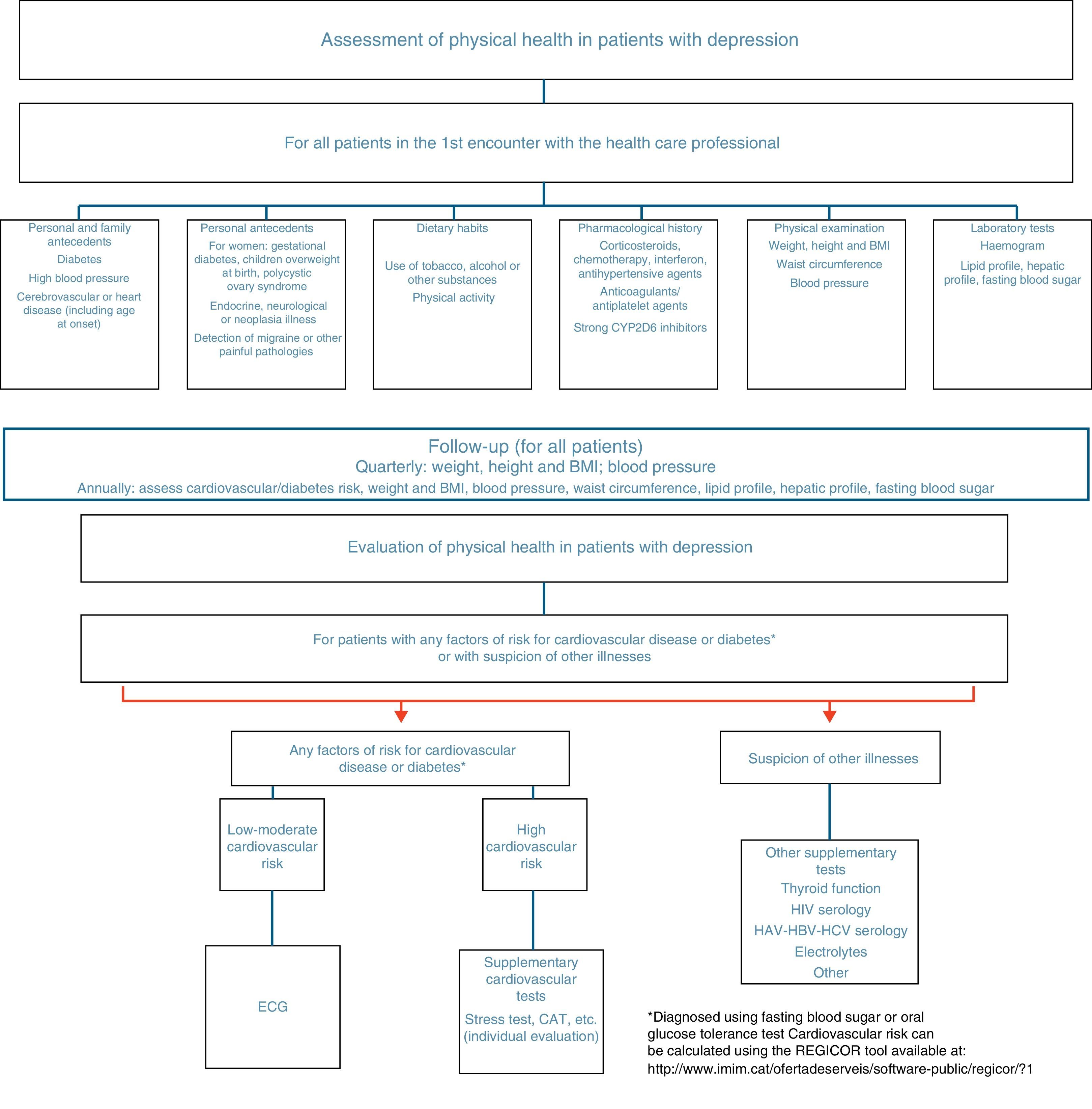
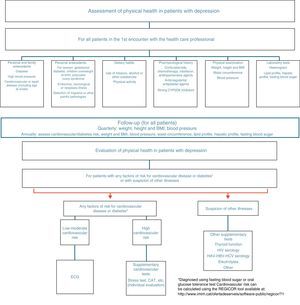
As has been commented previously, the prevalence of patients with depression and medical illnesses is very high and the association between both of them is bidirectional. Although studies on depression as a consequence of chronic illnesses are more common, the inverse relationship has also become seen in longitudinal population-based studies in which patients with a diagnosis of depression presented a greater level of disability and risk of suffering certain medical illnesses in comparison with the general population without depression.18–21 To detect the medical disorders that are most often associated with depression or its factors of risk, it is suggested that a somatic study should be carried out in patients with depression (Fig. 1). In the following sections we break down the role of depression as a factor of risk for medical illnesses, focusing on the pathologies in which the relationship is well established: cardiovascular diseases, metabolic alterations and chronic pain.
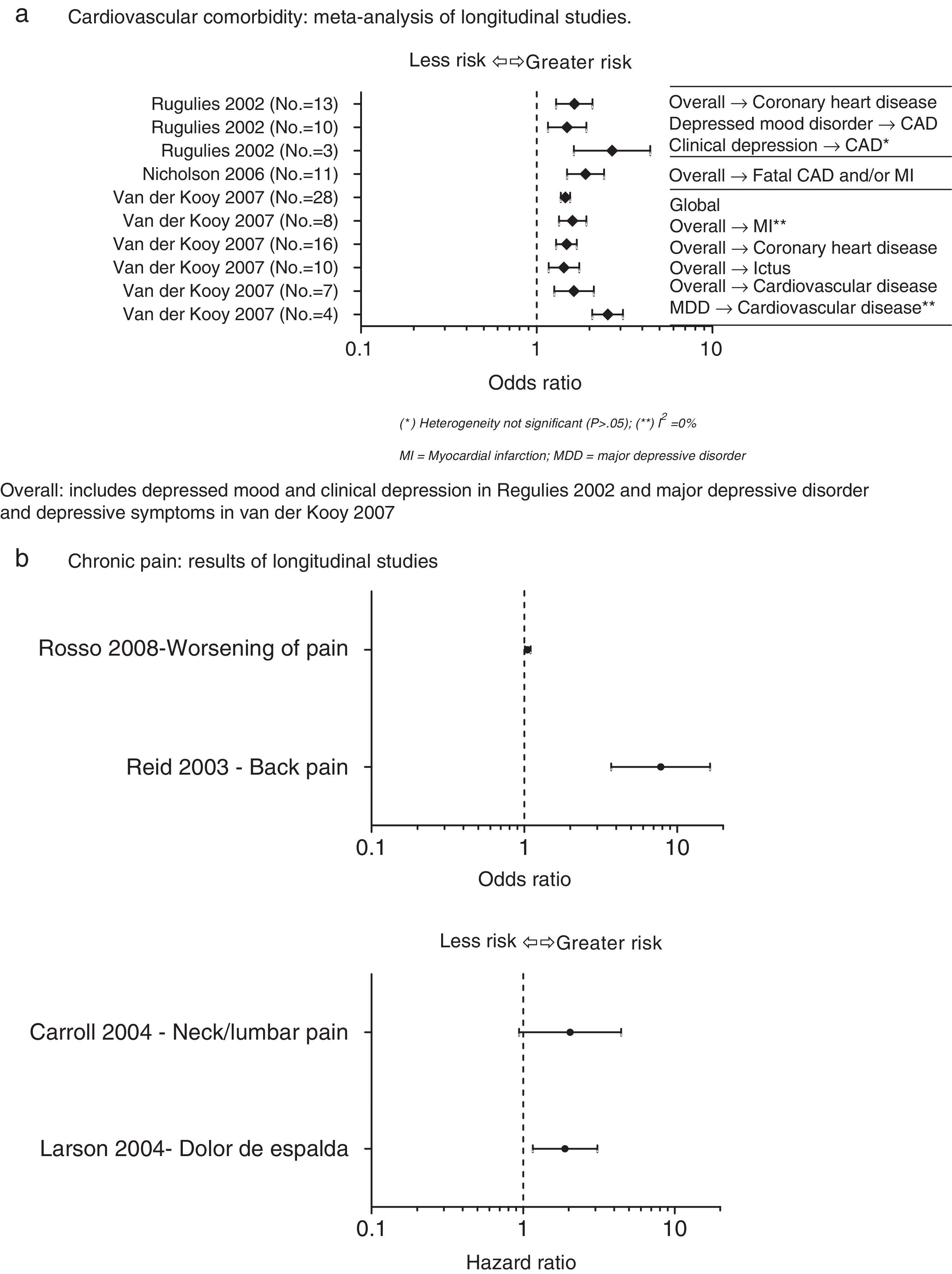
Depression as a cardiovascular risk factorThe prevalence of depression in patients with cardiovascular disease is disproportionately high in comparison with general population, reaching 50% in patients recently admitted for coronary by-pass surgery or for acute coronary syndrome.22 The results of various longitudinal studies reveal that depression is an independent cardiovascular risk factor. Fig. 2 shows the results of the longitudinal study meta-analyses identified in the references review that assess the relationship between depression and cardiovascular disease (Fig. 2a)23–25.
Depression as a factor of risk for medical illnesses. (A) Cardiovascular comorbidity: meta-analysis of longitudinal studies. Overall: includes depressed mood and clinical depression as in Regulies 2002 and major depressive disorder and depressive symptoms as in van der Kooy 2007. (B) Chronic pain: results of longitudinal studies. CAD, coronary artery disease; CV, cardiovascular; MDD, major depressive disorder; MI, myocardial infarction.
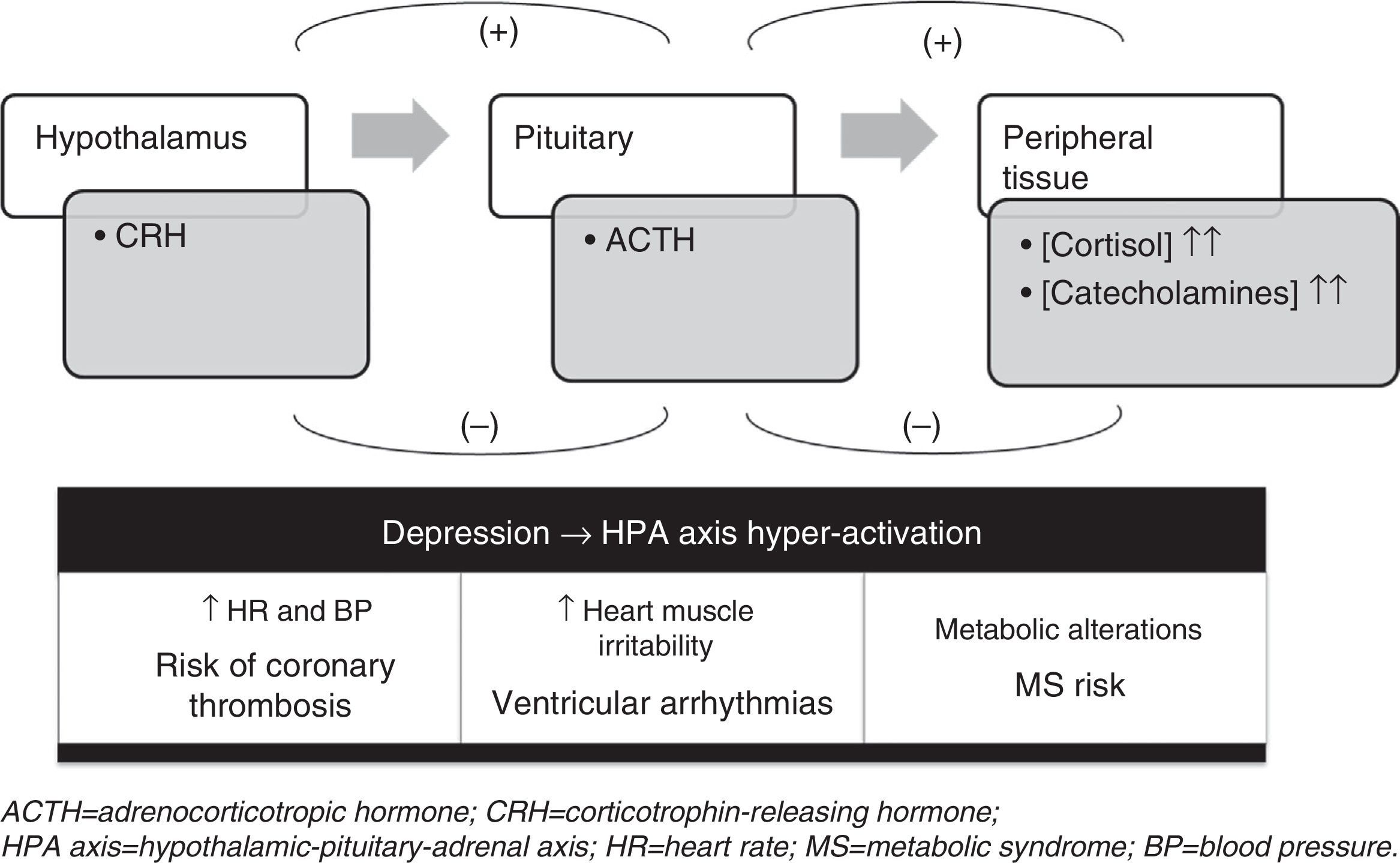
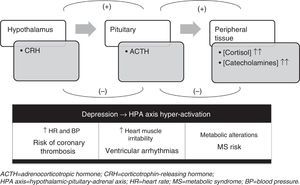
The possible reasons for the comorbidity of depression and cardiovascular disease fall into three types of mechanisms: biological, psychosocial and lifestyle. Within the biological mechanisms, hypothalamic–pituitary–adrenal (HPA) axis alterations seem to play a key role. In periods of stress and in depression, hyperactivity of the HPA axis occurs, stimulating the sympathetic nervous system and increasing the levels of circulating catecholamines (adrenaline and noradrenaline) and of serum cortisol. All of this provokes an imbalance between the sympathetic and parasympathetic activity, which translates in the cardiovascular system to an increase in heart rate, blood pressure, cardiac muscle irritability and metabolic alterations (Fig. 3).22 Besides the HPA axis alterations, there are other biological mechanisms that might be related with the link between depression and cardiovascular disease, such as the following: the alterations in platelet function described in patients with depression (which could be involved in the pathogenesis of acute manifestations of cardiovascular disease) and increases in plasma inflammatory factors (interleukin 6, anti-TNF-alpha and C-reactive protein).22
The comorbidity between depression and cardiovascular disease has a negative impact, not only from its repercussions on patient's quality of life and disability, but also from factors related with survival and mortality after acute cardiovascular events and from the possible risk that new cardiovascular events will appear. In addition, depression makes treatment adherence and rehabilitation programme follow-up more difficult and limits patient reincorporation to daily life activities. All of this involves an increase in the use of health care resources and associated costs.22
For all these reasons, as we have previously indicated, depression has to be considered an independent cardiovascular risk factor; this makes it necessary to assess cardiovascular risk in patients with depression. Such evaluation should be performed using existing clinical guidelines and protocols to assess cardiovascular risk and should be aimed at both primary prevention of cardiovascular disease and secondary prevention of post-event complications.22
Endocrine and metabolic disorders secondary to depressionThe prevalence of depression associated with endocrine/metabolic disorders (such as, for example, diabetes) is high and above the prevalence of depression in the general population.26 Specifically, the prevalence of depression in patients with diabetes is 2–3 times greater than in the general population, and, once again, the relationship between both conditions seems to be bidirectional.26In a meta-analysis performed with nine longitudinal studies that assessed the risk of diabetes in patients with depression, a moderate but significant increase was found in the risk of diabetes associated with depression (relative risk=1.37; confidence interval [CI] 95%: 1.14–1.63).27 Nevertheless, the heterogeneity among studies was significant (Q=18.3; P=.02), so it cannot be concluded that the studies included in the meta-analysis represent a single population.27
In the case of metabolic syndrome, there was also variability in the longitudinal studies carried out, among other reasons for the different definitions of metabolic syndrome used.28–31 In spite of this, none of these individual studies revealed a clear increase in the risk of metabolic syndrome associated with depression; there was only a certain increase in the risk of metabolic syndrome (defined with the criteria of the National Cholesterol Education Program Adult Panel III in the women with depression [odds ratio=2.5; CI 95%: 1.2–5.2]).30
As concerns the risk of obesity, the results of a meta-analysis with 4 studies associated depression with a greater possibility of developing (odds ratio=1.40; CI 95%: 1.15–1.71)]. Although the heterogeneity among studies was not significant (P=.19), it is impossible to rule out that this absence of statistical significance was from the lack of power (only 4 studies were included).32 In another meta-analysis that included a greater number of studies (n=22), a similar size of effect for the association between depression and obesity was also obtained (odds ratio=1.47; CI 95%: 1.16–1.85), with significant heterogeneity among studies (P<.01).33
Besides the neuro-hormonal alterations measured by the HPA axis dysregulation, already described earlier, and the unhealthy lifestyle of patients with depression, the secondary effects of the antidepressant treatments can also contribute to an increase in the risk of metabolic/endocrine alterations.26,34,35 In this context, the weight increase caused by certain antidepressants should be taken into consideration and the use of interventions for metabolic/endocrine diseases that prevent such weight increase should be evaluated, such as prescribing metformin for treating diabetes.26
Depression as a factor of risk for chronic painThe prevalence of depression and chronic pain is high in the primary care setting (56%) and reaches even higher figures in settings of specialised attention (50–69%).36
Although the existence of a relationship between pain and depression is clear, there are various hypotheses about the direction of this relationship. Some believe that depression could be an antecedent of pain, although there are few studies that have been able to validate this theory. In fact, in our literature review, longitudinal studies with contradictory results were identified. In some of these, there was a strong (although not very precise) association37; in others, the association was more moderate although the estimation was more precise;38 and, finally, in others no association at all was found39,40 (Fig. 2b). In contrast, the opposite hypothesis (that depression is a consequence of pain) was demonstrated in a meta-analysis in which it was confirmed that depression occurs more frequently in patients with chronic pain than in healthy controls.36 Lastly, there is a third hypothesis that suggests that there are common pathogenic mechanisms. This hypothesis considers that pain and depression are independent processes that share a common mechanism that can lead to the appearance of either of the 2 conditions without any causal relationships between them. Most of the theories that lean in this direction include the mechanisms of HPA axis action.36
Given the very high level of disability associated to the comorbidity of chronic pain and depression, and regardless of the direction of this association, we would recommend carrying out an objective assessment of pain in patients with depression using appropriate instruments (for example, visual analogue scales). In addition, a comprehensive therapeutic intervention evaluating the different possibilities of drug and non-drug treatment should be considered.36
Depression and other health problemsDepression has been linked to other physical health problems. In the case of osteoporosis, the evidence available on the role of depression as a causal factor is heterogeneous and inconclusive.41 The same is true of the effect of maternal depression as a factor of risk factor for perinatal complications.42–46 With respect to cancer, none of the longitudinal studies identified in the review demonstrated that depression plays a clear role as a factor of risk for the appearance of cancer.47–55
Turning to another subject, there is growing interest in the relationship between depression and inflammation. In 2 recent meta-analyses it was found that individuals with depression presented an increase in some inflammatory markers such as C-reactive protein, interleukin 6 and TNF-alpha, in comparison with non-depressed individuals.56,57 The presence of this immune dysregulation could explain the comorbidity between depression and some physical illnesses such as cardiac alterations or diabetes.58 Various factors can affect this relationship between depression and inflammatory alterations. Men having a later onset of depression might present a greater risk,59 although some other studies indicate that the role of sex is not completely clear.57,60 Patients with a more serious or a chronic disorder could also show a greater level of inflammation.61,62 Finally, antidepressant treatment could affect inflammation levels differentially, with selective serotonin reuptake inhibitors being associated with a reduction in some of these markers,63 and serotonin and noradrenalin reuptake inhibitors and tricyclic antidepressants associated with increased inflammation.58,59,64
To approach the subject of medical comorbidity associated with depression in the primary care setting, we discussed the stigma attached to depression and to the various aspects of its treatment. To attempt to eliminate this stigma, it is important to heighten the awareness of the professionals and to encourage communication between psychiatrists and primary care physicians. Likewise, it is important to improve doctor–patient communication through an appropriate clinical interview and facilitate techniques of coping and positive reinforcement for patients who need them.65
Antidepressant treatment and physical healthWhen choosing an antidepressant treatment for patients with associated medical comorbidity, 2 key aspects should be considered: on the one hand, the secondary effects of the antidepressant in relation with this somatic illness and, on the other, the possible interactions of the antidepressant with the drugs for treating the physical illness. It is important to emphasise that this situation can condition the choice of the antidepressant, but it does not prevent the use of a drug treatment when considered necessary.
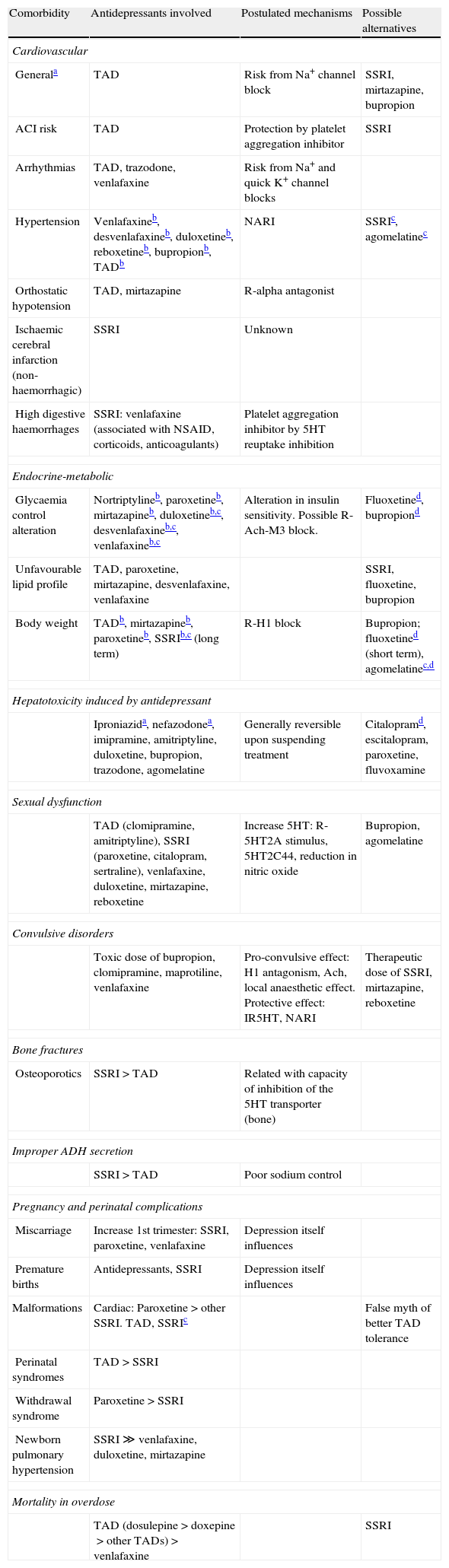
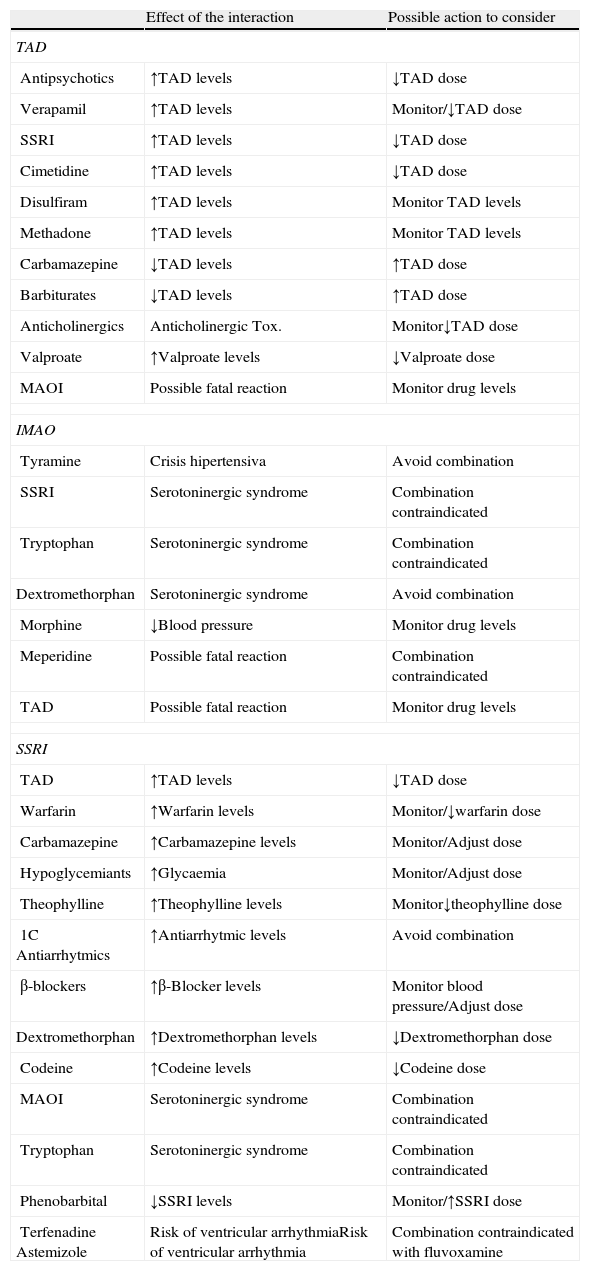
Table 2 presents a summary of the secondary effects of the most common antidepressants based on the associated comorbid pathology. When there is sufficient evidence available, we have also included the possible mechanisms involved and the various alternatives that could be considered for each case.66 As far as possible interactions between the antidepressant treatments with other drugs, Table 3, represent a summary of the effect of the most relevant interactions seen with tricyclic antidepressants, monoamine oxidase inhibitors and selective serotonin reuptake inhibitors, as well as the alternatives to be considered in these situations.66
Secondary effects of antidepressants.
| Comorbidity | Antidepressants involved | Postulated mechanisms | Possible alternatives |
| Cardiovascular | |||
| Generala | TAD | Risk from Na+ channel block | SSRI, mirtazapine, bupropion |
| ACI risk | TAD | Protection by platelet aggregation inhibitor | SSRI |
| Arrhythmias | TAD, trazodone, venlafaxine | Risk from Na+ and quick K+ channel blocks | |
| Hypertension | Venlafaxineb, desvenlafaxineb, duloxetineb, reboxetineb, bupropionb, TADb | NARI | SSRIc, agomelatinec |
| Orthostatic hypotension | TAD, mirtazapine | R-alpha antagonist | |
| Ischaemic cerebral infarction (non-haemorrhagic) | SSRI | Unknown | |
| High digestive haemorrhages | SSRI: venlafaxine (associated with NSAID, corticoids, anticoagulants) | Platelet aggregation inhibitor by 5HT reuptake inhibition | |
| Endocrine-metabolic | |||
| Glycaemia control alteration | Nortriptylineb, paroxetineb, mirtazapineb, duloxetineb,c, desvenlafaxineb,c, venlafaxineb,c | Alteration in insulin sensitivity. Possible R-Ach-M3 block. | Fluoxetined, bupropiond |
| Unfavourable lipid profile | TAD, paroxetine, mirtazapine, desvenlafaxine, venlafaxine | SSRI, fluoxetine, bupropion | |
| Body weight | TADb, mirtazapineb, paroxetineb, SSRIb,c (long term) | R-H1 block | Bupropion; fluoxetined (short term), agomelatinec,d |
| Hepatotoxicity induced by antidepressant | |||
| Iproniazida, nefazodonea, imipramine, amitriptyline, duloxetine, bupropion, trazodone, agomelatine | Generally reversible upon suspending treatment | Citalopramd, escitalopram, paroxetine, fluvoxamine | |
| Sexual dysfunction | |||
| TAD (clomipramine, amitriptyline), SSRI (paroxetine, citalopram, sertraline), venlafaxine, duloxetine, mirtazapine, reboxetine | Increase 5HT: R-5HT2A stimulus, 5HT2C44, reduction in nitric oxide | Bupropion, agomelatine | |
| Convulsive disorders | |||
| Toxic dose of bupropion, clomipramine, maprotiline, venlafaxine | Pro-convulsive effect: H1 antagonism, Ach, local anaesthetic effect. Protective effect: IR5HT, NARI | Therapeutic dose of SSRI, mirtazapine, reboxetine | |
| Bone fractures | |||
| Osteoporotics | SSRI>TAD | Related with capacity of inhibition of the 5HT transporter (bone) | |
| Improper ADH secretion | |||
| SSRI>TAD | Poor sodium control | ||
| Pregnancy and perinatal complications | |||
| Miscarriage | Increase 1st trimester: SSRI, paroxetine, venlafaxine | Depression itself influences | |
| Premature births | Antidepressants, SSRI | Depression itself influences | |
| Malformations | Cardiac: Paroxetine>other SSRI. TAD, SSRIc | False myth of better TAD tolerance | |
| Perinatal syndromes | TAD>SSRI | ||
| Withdrawal syndrome | Paroxetine>SSRI | ||
| Newborn pulmonary hypertension | SSRI≫venlafaxine, duloxetine, mirtazapine | ||
| Mortality in overdose | |||
| TAD (dosulepine>doxepine>other TADs)>venlafaxine | SSRI | ||
ACI, acute myocardial infarction; NARI, noradrenaline reuptake inhibition; NSAIDs, nonsteroidal anti-inflammatory drugs; SSRI, selective serotonin uptake inhibitors; TAD, tricyclic antidepressant.
Interactions of antidepressant treatments.
| Effect of the interaction | Possible action to consider | |
| TAD | ||
| Antipsychotics | ↑TAD levels | ↓TAD dose |
| Verapamil | ↑TAD levels | Monitor/↓TAD dose |
| SSRI | ↑TAD levels | ↓TAD dose |
| Cimetidine | ↑TAD levels | ↓TAD dose |
| Disulfiram | ↑TAD levels | Monitor TAD levels |
| Methadone | ↑TAD levels | Monitor TAD levels |
| Carbamazepine | ↓TAD levels | ↑TAD dose |
| Barbiturates | ↓TAD levels | ↑TAD dose |
| Anticholinergics | Anticholinergic Tox. | Monitor↓TAD dose |
| Valproate | ↑Valproate levels | ↓Valproate dose |
| MAOI | Possible fatal reaction | Monitor drug levels |
| IMAO | ||
| Tyramine | Crisis hipertensiva | Avoid combination |
| SSRI | Serotoninergic syndrome | Combination contraindicated |
| Tryptophan | Serotoninergic syndrome | Combination contraindicated |
| Dextromethorphan | Serotoninergic syndrome | Avoid combination |
| Morphine | ↓Blood pressure | Monitor drug levels |
| Meperidine | Possible fatal reaction | Combination contraindicated |
| TAD | Possible fatal reaction | Monitor drug levels |
| SSRI | ||
| TAD | ↑TAD levels | ↓TAD dose |
| Warfarin | ↑Warfarin levels | Monitor/↓warfarin dose |
| Carbamazepine | ↑Carbamazepine levels | Monitor/Adjust dose |
| Hypoglycemiants | ↑Glycaemia | Monitor/Adjust dose |
| Theophylline | ↑Theophylline levels | Monitor↓theophylline dose |
| 1C Antiarrhytmics | ↑Antiarrhytmic levels | Avoid combination |
| β-blockers | ↑β-Blocker levels | Monitor blood pressure/Adjust dose |
| Dextromethorphan | ↑Dextromethorphan levels | ↓Dextromethorphan dose |
| Codeine | ↑Codeine levels | ↓Codeine dose |
| MAOI | Serotoninergic syndrome | Combination contraindicated |
| Tryptophan | Serotoninergic syndrome | Combination contraindicated |
| Phenobarbital | ↓SSRI levels | Monitor/↑SSRI dose |
| TerfenadineAstemizole | Risk of ventricular arrhythmiaRisk of ventricular arrhythmia | Combination contraindicated with fluvoxamine |
MAOI, monoamine-oxidase inhibitor; SSRI, selective serotonin reuptake inhibitor; TAD, tricyclic antidepressants; ↑, increase; ↓, reduce.
It is important to bear in mind that some adverse effects of antidepressants are difficult to diagnose, especially during the acute period of the episode, given that it might also be somatic symptoms of the illness that are being dealt with. In the case of sexual dysfunction, which is more frequent in patients with depression,67 can be aggravated by the treatment, given that some antidepressants (especially selective serotonin reuptake inhibitors and serotonin and noradrenalin reuptake inhibitors) are associated with a very high frequency of sexual dysfunction.68
Besides drug treatment, the use of psychotherapy in patients with depression and medical comorbidity has also been studied, principally in the areas of cardiovascular problems, oncology and chronic pain. The efficacy of psychotherapy, alone or in combination with drug treatment, has been demonstrated in patients with slight to moderate depression associated with this type of physical illnesses. The techniques shown to have greater efficacy in this type of patients have been cognitive behavioural strategies.69
Consensual decalogue- 1
Depression and certain physical illnesses present a bidirectional relationship that makes diagnosis more difficult, affects prognosis negatively and brings up specific requirements for intervention and follow-up.
- 2
Patients with a diagnosis of depression should be screened for physical illnesses or factors of risk. Likewise, patients with physical illnesses should receive a screening for depression.
- 3
Patients with depression and physical illness require investigation as to the presence of suicide ideation or risk. If they are present, urgent referral to mental health services should be considered.
- 4
The presence of physical illnesses in patients with depression can condition, although not prevent, the choice of antidepressant treatment. The best drug alternative should take into consideration the type of comorbid physical illness and the secondary effects and interactions of the different antidepressants.
- 5
Psychotherapy, alone or in combination with psychotropic drugs, has been shown to be effective in slight to moderate depression in most patients with comorbid physical illness and contributes to comprehensive patient recovery. The psychotherapies that have demonstrated the greatest efficacy in this type of patients have been those with a cognitive-behavioural orientation.
- 6
Depression should be considered an independent factor of cardiovascular and metabolic risk; consequently, for these patients, the recommendations of primary or secondary prevention established for individuals with cardiovascular or metabolic risk should be applied.
- 7
The high comorbidity of depression and pain worsens the prognosis of the 2 clinical entities and makes active detection of both of them obligatory, using appropriate instruments and a comprehensive therapeutic intervention (pharmacological as well as non-pharmacological).
- 8
Patients with depression and physical illness often require the shared care of the primary care physician, the psychiatrist and, sometimes, of other specialists and professionals. It is essential to facilitate appropriate channels of communication to achieve flexible, efficient coordination throughout the entire process.
- 9
The stigma associated with mental illness carries a disadvantageous situation and poorer opportunities of receiving appropriate diagnosis and treatments, both in the case of the mental illness as in that of physical illness.
- 10
Public health care actions need to recognise and emphasise how important the association between depression and physical illness is, facilitating early detection and appropriate care.
Dr. Bobes has received research funding and/or has participated as a consultant and/or speaker at activities organised by the following companies: Adamed, Almirall, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Glaxo-Smith-Kline, Janssen-Cilag, Lundbeck, Merck, Novartis, Organon, Otsuka, Pfizer, Pierre-Fabre, Roche, Sanofi-Aventis, Servier, Shering-Plough, and Shire.
Teresa Hernando has provided consultant services for the following companies: Adamed, AstraZeneca, Lilly, Pfizer, Roche, Rovi and Servier.
Dr. Ángela Ibáñez has received funding for teaching and research activities and for attending congresses and scientific meetings (from Servier, Otsuka Pharmaceutical SA, Bristol-Myers Squibb, Lündbeck, Pfizer, Ferrer and Adamed) but this has not affected her contributions to the content of this article.
Dr. Diego Palao has received funding for educational programmes or courses from Janssen, Lundbeck, Otsuka, Pfizer, Almirall, GSK, Lilly, Rovi and Servier; research assistance from Fundación Astra-Zeneca; fees for consultant services or presenter from Lundbeck and Servier; and funding for meetings and congresses from Lilly.
Dr. Rico-Villademoros has provided consultant services for the following companies: Adamed, Almirall, AstraZeneca, Bristol-Myers Squibb, Lilly, Pfizer, Roche, Rovi and Servier.
Dr. Saiz-Ruiz has participated as a consultant and/or speaker at activities organised by Lilly, GlaxoSmithKline, Lundbeck, Janssen, Servier and Pfizer; and has received research funding from Lilly, Astra-Zeneca, Bristol-Myers and Wyeth.
The rest of the authors have no conflicts of interest pertinent to this article to declare.
We thank Laboratorios Rovi for their sponsorship and support of this project. No Laboratorios Rovi employee participated in the technical development of the project in general or of this manuscript in particular.
Scientific committee: Bobes, Julio; Giner, José; López, Francisco; Saiz Ruiz, Jerónimo; Zamorano, Enric. Coordinators: Álamo, Cecilio; Cervilla, Jorge A.; Ibáñez Cuadrado, Ángela; Ibáñez Guerra, Elena; López, Silvia; Morán, Pedro; Palao, Diego J.; and Romacho, Montserrat. Participating experts: Agüera Ortiz, Luis F.; Aguilar García-Iturrospe, E. Jesús; Caballero, Luis; Cano Espín, Agustina; Carrasco, José Luis; Casquero, Rafael; Franco, M. Paines; García Campayo, Javier; Gasull, Vicente; Hernando, Teresa; Iglesias, Celso; Martín Carrasco, Manuel; Menchón Magrina, José Manuel; Montes, José Manuel; Moriñigo Domínguez, Ángel; Montejo González, Ángel Luis; Paramo, Mario; Ramírez, Raquel; Reviriego, Germán; Rico-Villademoros, Fernando; Rojo, Luis; Sáiz, Pilar A.; Vaz Leal, Francisco J.; Vidal Pardo, Francisco; and Villamarín, José Ramón.
Please cite this article as: Giner J, Saiz Ruiz J, Bobes J, Zamorano E, López F, Hernando T, et al. Consenso español de salud física del paciente con depresión. Rev Psiquiatr Salud Ment (Barc.). 2014;7:195–207.
The names of the members of the Group for the Development of Recommendations on Physical Health in Patients with Depression are listed in Appendix 1.