Prevention of suicidal behaviour is a public health priority in the European Union. A previous suicide attempt is the best risk predictor for future attempts, as well as completed suicides. The primary aim of this article is to describe a controlled study protocol designed for prevention of recurrent suicidal behaviour that proposes case management, and includes a psychoeducation program, as compared with the standard intervention (PSyMAC).
MethodsPatients admitted from January 2011 to June 2013 to the emergency room of the Hospital Universitario Central de Asturias were evaluated using a protocol including sociodemographic, psychiatric, and psychosocial assessment. Patients were randomly assigned to either a group receiving continuous case management including participation in a psychoeducation program (experimental group), or a control group receiving standard care. The primary objective is to examine whether or not the period of time until recurrent suicidal behaviour in the experimental group is significantly different from that of the control group.
ConclusionPSyMAC proposes low cost and easily adaptable interventions to the usual clinical setting that can help to compensate the shortcoming of specific action protocols and suicidal behaviour prevention programs in our country. The evaluation of PSyMAC results will determine their real effectivity as a case-management program to reduce suicidal risk.
La prevención del comportamiento suicida es una prioridad en la salud pública de la Unión Europea. La tentativa suicida previa es el mejor predictor de riesgo de futuras tentativas suicidas y de suicidio consumado. El principal objetivo de este artículo es describir el protocolo de un estudio controlado diseñado para prevenir la recurrencia de comportamientos suicidas que propone el manejo de casos, e incluye un programa psicoeducativo, en comparación con la intervención clínica habitual (PSyMAC).
MétodosSe monitorizó con un protocolo que incluye variables sociodemográficas y evaluación psiquiátrica y psicosocial a los pacientes que, desde enero de 2011 a junio de 2013, acudieron al Servicio de Urgencias del Hospital Universitario Central de Asturias, tras haber realizado una tentativa suicida. Los pacientes se asignaron de manera aleatoria a un grupo que recibía una atención continuada basada en el manejo de casos incluyendo participación periódica en un programa psicoeducativo (grupo experimental) o a un grupo control que recibía los cuidados clínicos habituales. El objetivo principal es determinar si el período de tiempo hasta la recurrencia del comportamiento suicida es significativamente diferente en el grupo experimental y en el grupo control.
ConclusiónEl PSyMAC propone intervenciones de bajo coste y fácilmente adaptables al entorno clínico habitual que pueden ayudar a suplir la carencia de protocolos específicos de actuación y de programas preventivos de comportamiento suicida existente en nuestro país. La evaluación de resultados del PSyMAC permitirá determinar su efectividad real en el manejo y reducción del riesgo de suicidio.
More than 1 million people commit suicide each year in the entire world, making suicide 1 of the most important global public health problems.1 In Spain, the data contributed by the National Institute of Statistics show that suicide has been the number 1 unnatural cause of death since 2008, over traffic accidents. This situation has stayed invariable up until 2012, the year for which the most recent data are available.2 However, the figures could be even higher, as the tendency to underreport is widely known in most countries, including Spain. This is due to the great difficulty in quantifying real suicide data, as there are clear discrepancies between data provided by the National Statistics Institute and the Legal Medicine Institutes. Neither of the 2 sources can be considered the most reliable.3
Currently, the concern is even greater if the alarming data from some countries are taken into account, regarding the influence of the economic crisis on suicidal behaviour.4 Specifically, in Spain, a recent analysis in this regard showed a potential association between loss of employment and increase in suicide rate. During the 2008–2012 period, each 10% annual increase in unemployment was accompanied by a 1.22% increase in the mean number of suicides.5
In the case of suicide attempts, the difficulties in knowing the real magnitude of the problem are even more evident, with official figures being lacking and there being suggestions that their numbers could be 10–20 times higher than the number of completed suicides. In this sense, one must consider that calculating suicide attempts involves many methodological difficulties. The main one is that it concerns a heterogeneous group of patients with respect to planning, degree of fatality, method choice, suicidal intention or the use of different definitions of what constitutes a suicide attempt.6 Therefore, from a preventative standpoint, correct assessment of people that resort to emergency hospital services after a suicide attempt,7 and of those that are hospitalised because of an attempt,8 is fundamental for knowing the true magnitude of the suicidal behaviour problem.
In our environment, we have monitored suicide attempts over the last 5 years attended in the emergency department of the referral hospital in Health Area IV in Asturias (Oviedo), the Central University Hospital of Asturias (HUCA in Spanish). We have been able to establish a suicide attempt rate of 99.1 for every 100,000 inhabitants (men: 69.1; women: 129.1). The most frequently used method was drug overdose (90% of patients).9 It is important to highlight that the percentage of patients that had made previous suicide attempts was high (55.4% of cases). More specifically, 30.1% had attempted suicide in the previous year.
Multiple studies show previous suicide attempts as one of the risk factors that most clearly predict the possibility of a future completed suicide.10,11 Therefore, appropriate examination12 and therapeutic management (both short and long-term) of these patients13 are fundamental in reducing later suicide risk.14
Suicidal behaviour is complex because of the interaction between genetic, biological, psychological and environmental factors; however, psychological autopsy study results indicate that around 90% of the patients that commit suicide could have been diagnosed with a psychiatric disorder that was potentially susceptible to intervention and treatment.15
To date, randomised controlled trials based on intervention with people that have made previous suicide attempts are scarce. It has been shown that programmes potentiating increased adherence to outpatient post-attempt treatment are associated with a significant decrease in the rate of repeating a suicide attempt.16 Specific examples of interventions that promote therapeutic adherence, which have already demonstrated their effectiveness in prevention of suicidal behaviours, would be systematic, intensive follow-up by telephone using “crisis cards”,17 intensive contact through mail18 or psychosocial case management.15 Therefore, the development of case management as a specific intervention method for patients with previous suicide attempts may be an appropriate intervention tool, as it facilitates a multidimensional and comprehensive therapeutic approach that includes continuous follow-up of the patient to support adherence, individualised case treatment and more appropriate coordination of the use of social resources in the community.19
In this article, we describe the PSyMAC protocol, a controlled study designed to prevent the recurrence of suicidal behaviours. It proposes case management, and includes a psychoeducational programme, in comparison with the standard clinical intervention.
This protocol is intended to be an integrating model in which several of the previously mentioned interventions are included, adding group psychoeducation as a novel complementary contribution. The motive for including a psychoeducational programme was based on its effectiveness, already demonstrated in several mental disorders like schizophrenia,20 bipolar disorder21,22 or recurrent depressive disorder.23 However, it should be emphasised that this strategy has not been used as a specific therapeutic instrument in the prevention of suicidal behaviour in people with previous suicide attempts. Consequently, one of the objectives of this present study was to demonstrate its effectiveness or lack thereof.
MethodDesignOpen, controlled, multicentric study to examine the effectiveness of an intervention protocol, centred on case management of patients that request emergency services after making a suicide attempt.
Study subjectsParticipation in the study was offered to all patients that sought out services at the HUCA Emergency Department, referral hospital in Health Area IV in Asturias (Oviedo), between 1 January 2011 and 30 June 2013, after making a suicide attempt.
Inclusion criteria: (1) subjects were older than 18 years; (2) attended the HUCA Emergency Department after making a suicide attempt in the period mentioned; (3) pertained to Health Area IV in Asturias, which includes 5 independent mental health centres; and (4) agreed to participate in the study and signed the corresponding informed consent.
Exclusion criteria: (1) subjects did not comply with all inclusion criteria; or (2) were incapable of understanding the significance or consequences of their actions.
For the definition of “suicide attempt”, the WHO/EURO24 criteria were used: an act whose result is not death, in which an individual, deliberately and without intervention from others, caused harm to herself or ingested a substance at a higher dosage than what is recognised as therapeutic, with the objective of making changes through the anticipated or derived physical consequences of said act. This includes: acts interrupted by others before harm occurs. This excludes: acts carried out by people that do not understand the significance or consequences of their action.
RandomisationPatients that complied with the established criteria were assigned to the experimental (case management) or control groups based on their availability and personal preferences.
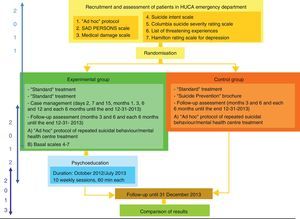
InterventionAll patients that agreed to participate in the study, independently of the group to which they were assigned, received a brochure centred on prevention of suicidal behaviour in the moment they accepted. In Fig. 1, the procedure for action in each of the 2 study groups is summarised.
Experimental group: case managementThe case management activities included:
- (1)
Periodic interviews with patients. The personnel responsible for managing the cases periodically contacted the people assigned to the experimental group (days 2, 7 and 15, months 1, 3, 6 and 12 after signing their informed consent, and then every 6 months until the end of the study). Contact was made preferably in a personal interview, using interview by telephone as a second option.
- (2)
Gathering information about the therapeutic situation in the moment of the interview.
- (3)
Stimulating therapeutic adherence (to their mental health centre and habitual treatment).
- (4)
Coordinating periodic appointments with a referral psychiatrist.
- (5)
Promote the return to therapy of patients who voluntarily stopped treatment.
- (6)
Facilitate contact with existing social resources in the community for patients that need them.
- (7)
In the same vein, patients assigned to this group received the treatment considered most appropriate by their psychiatrist and participated in a psychoeducational programme (based on World Health Organisation and International Association for Suicide Prevention guidelines).
The group psychoeducational programme was specifically developed for this present study. It consists of 10 group sessions (Fig. 2), meeting once a week for 60min each session. In each group, 8–10 people were included and the sessions were conducted by specialised multidisciplinary personnel (psychologists and psychiatrists), with 2 present in each group. Each session featured the following sections: commencement, recapitulation and doubts, new issues, leave-taking and material to develop at home.
During the sessions, the issues addressed were related to the suicidal act, how to prevent it by learning communication skills, strengthening personal abilities in confronting crisis situations, analysing psychological changes that drive us to alarming situations, risk factors and protective factors for suicide, introducing stress management and knowledge of social support and health or social resources, among others.
Control groupPatients assigned to the control group received clinical treatment that their referral psychiatrist considered most opportune. Likewise, they received a brochure centred on prevention of suicidal behaviour upon agreeing to participate in the study.
AssessmentAssessment was performed by psychiatrists or psychologists appropriately trained for it (Fig. 1).
Basal evaluation (performed upon inclusion in the study) which included: (1) sociodemographic data, family background, personal history (including psychopathology, previous psychiatric hospitalisations and history of abuse/mistreatment), current clinical situation (psychiatric disorder and type of treatment and somatic diseases, all gathered from the patients’ clinical histories), psychosocial evaluation and aspects related to the current suicide attempt25; (2) SAD-PERSONS scale26; (3) Medical Damage Scale (MDS)27 for a suicide attempt; (4) Suicide Intent Scale (SIS)28; (5) Columbia Suicide Severity Rating Scale (C-SSRS)29; (6) Brugha List of Threatening Experiences (LTE)30; and (7) Hamilton Rating Scale for Depression (HRDS).31
Follow-up assessment (carried out in months 3, 6 and later, each 6 months until the end of the follow-up period). This included: (1) data relevant to possible later suicide attempts, collected at the moment of being included in the study (or cause of death in the case of a completed suicide); (2) data relevant to clinical treatment followed by the patient in their referral mental health centre (or private psychiatrist, if applicable) and adherence to this treatment; and (3) C-SSRS29; (4) LTE30; and (5) HRDS.31
Control groupBoth the basal evaluation and follow-up assessments were similar to those carried out in the experimental group, except that features 3–5 of the follow-up were not included.
Statistical analysisThe main study variable was time passed until the first instance of suicidal behaviour (attempted or completed suicide) after inclusion in the study. Given that recurrence of a suicidal episode is an elevated risk factor for a later completed suicide, it was considered essential to measure the time passed until the next suicidal behaviour in order to develop effective prevention strategies.
Secondary variables included: (1) mortality rate (experimental and control group); (2) incidence number and rate for recurrent suicidal behaviour, expressed as repeated suicide attempts per person per year (experimental and control group); and (3) HRDS score (experimental group).
Primary analysis: The main objective of this study was to determine if the time period until the recurrence of suicidal behaviour was significantly different in the experimental group compared to the control group. To do this, a stratified log-rank test that included all patients in the study was performed, following the principle of intention to treat. To carry out this analysis, a unilateral test was considered, as it would only be pertinent to know whether the experimental group was higher than the control; the significance level used was 2.5% and the power was 90%.
Secondary analysis: Its objective was to reinforce the findings of the primary analysis. A subgroup analysis was performed (based on sex, age and suicide attempts made prior to inclusion in the study) with the secondary variables. Given that the secondary analysis had an exploratory nature, no adjustment was performed with multiple tests.
Ethical aspectsThe researchers are committed to respecting all the aspects established in existing legislation within the clinical research material available in the Helsinki Declaration, the Council of Europe Convention, relative to human rights and biomedicine, and in the UNESCO Universal Declaration of human rights. They also agree to comply with the requisites established in Spanish legislation within the medical research field, protection of data, personal character and bioethics, with Law 14/2007, of July, on biomedical research, as well as with the rest of the requisites established by Spanish legislation in that respect.
This study was submitted for approval to the HUCA Clinical Research Ethics Committee. Informed consent was obtained from the patients for participation in the study. If a patient refused to continue in the study, the gathering of data referring to that patient was immediately stopped.
Given the harmlessness of the complementary tests performed (psychometric tests) and the absence of interference with treatment guidelines, this was considered a study with minimal risk.
DiscussionThis article describes a programme that would determine the effectiveness of case management in the prevention of recurrent suicidal behaviour. The PSyMAC protocol of action includes the gathering of sociodemographic information, as well as a psychiatric and psychosocial assessment of the patients that go to emergency care services at a regional referral hospital after attempting suicide. Likewise, individualised follow-up of the patients is performed, and participation in a preventative psychoeducational programme is facilitated.
The main objective of the present proposal consisted of the search for useful preventative strategies to avoid the recurrence of suicidal behaviour. Some authors32 have proposed different interventions to reduce the rate of repeated suicide attempts. PSyMAC proposes case management, including a preventative psychoeducational programme, as a potentially effective intervention. Some authors15 have studied case management, proposing integral and multidisciplinary care with outpatient follow-up to increase compliance. In our case, we performed periodic interviews with the patients, collecting information about their clinical situation and therapeutic adherence, coordinating periodic appointments with their referral psychiatrist and fostering a therapeutic environment for the patients that voluntarily ceased treatment. Similarly, contact with existing social resources in the community was facilitated, favouring a biopsychosocial approach. However, the strong point of PSyMAC that distinguishes it may be the inclusion of group psychoeducation in the programme: this is specifically designed for the prevention of suicide risk, consisting of 10 weekly sessions, each lasting 60min, directed by specialised personnel (psychologists and psychiatrists). It is an integrative psychoeducational model that uses a set of tools already mentioned in other studies and metaanalyses10 with satisfactory results, e.g., cognitive behaviour techniques, problem resolution training, communication skills, relaxation techniques, providing an emergency card, prevention and intervention techniques for a crisis, improving therapeutic adherence and compliance, as well as adequate use of sociohealth resources.
Another key characteristic of PSyMAC is the gathering of standardised data, carried out by research team members in situ (HUCA Emergency Department), interviewing the patient directly. Emergency departments are the place where people that attempt suicide typically go to receive the medical care necessary. Therefore, efforts are made to try to reduce patient selection bias, given that a significant tendency to underreport suicide attempts has already been detected. Many patients, once the medical emergency is resolved, do not seek specialised mental health services, and are consequently not detected as cases.
The use of a prospective design is another strong point of the study over other models that gather retrospective data. Many times, the data collected in clinical histories come from incorrect assessment. Specifically, an observational study carried out in 4 public hospitals in the Madrid community demonstrated that the clinical reports of the people that had attended these hospitals after attempting suicide were incomplete.33 Many discharge reports do not show a diagnosis that adequately emphasises suicide risk and the act of self-harm. All of this prevents the existence of longitudinal data, at a national and international level, that is reliable, allows adequate comparisons to be made, reveals the magnitude of the problem and permits the development of specific preventative actions appropriate for the problem.19 Therefore, in our protocol, we gather sociodemographic, clinical and psychometric data that do not routinely appear in emergency department clinical histories.
The main limitation of this study lies in the possible losses (within the experimental group) throughout the period of intervention and follow-up, due to the longitudinal design of the study and the low therapeutic adherence usually detected in patients that attempt suicide. However, incorporating into the study people that work in the centre where the experimental intervention takes place, as well as the experience of group participation, can reduce these losses. In fact, because the gathering of cases has been finalised at this point, we can affirm that this limitation has not existed, as we have been able to recruit patients mentioned a priori. Furthermore, preliminary analysis reveals that the “follow-up” sample is representative of the initial sample from the sociodemographic and clinical points of view, despite the number of withdrawals during the study period. Another possible limitation of the study lies in the way that patient randomisation was carried out, as availability and personal preference were considered, which could have created a self-selection bias.
In conclusion, we can indicate that the PSyMAC proposes low-cost interventions that are easily adaptable in the typical clinical environment and can help to compensate for the lack of specific protocols for action and programmes to prevent suicidal behaviour in our country. It could become an effective programme for management and reduction of suicide risk.
Ethical responsibilitiesHuman and animal protectionThe authors declare that the procedures followed conformed to the standards of the ethics committee for responsible human experimentation, and are in agreement with the World Medical Association and the Helsinki Declaration.
Data confidentialityThe authors declare that they have followed the protocols of their centre regarding publication of patient data and that all patients included in the study have received sufficient information and have given their informed consent in writing to participate in said study.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects referred to in this article. This document is in possession of the corresponding author.
FundingThis study was in part subsidised by the Spanish Ministry of Economy and Competitiveness, the Carlos III Health Institute (reference: PI10/-1632) and the Mental Health Network Research Centre (CIBERSAM in Spanish). Patricia Burón was funded through the predoctoral Severo Ochoa grant from the Asturias Foundation for Promotion of Applied Scientific Research and Technology (FICTY in Spanish).
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Sáiz PA, Rodríguez-Revuelta J, González-Blanco L, Burón P, Al-Halabí S, Garrido M, et al. Protocolo de estudio de un programa para la prevención de la recurrencia del comportamiento suicida basado en el manejo de casos (PSyMAC). Rev Psiquiatr Salud Ment (Barc.). 2014;7:131–138.