Metastases to the breast from an extra-mammary malignancy are extremely rare. Lymphomas and melanomas are the most commonly reported secondary tumors in the breast. Breast metastasis from an esthesioneuroblastoma is extremely rare and only 3 cases are described in the literature. We herein report another case of 31 year-old woman diagnosed with an esthesioneuroblastoma since two years, who presented to our hospital for a breast rapidly growing mass in the right upper inner quadrant. On physical examination, this mass measured 3cm, was firm with no skin retraction and no nipple discharge. Imaging features revealed multiples nodules with irregular border. A fine needed biopsy was performed. On pathological examination, the tumor was arranged in nests and lobules of monotonous tumor cells with round nuclei, indistinct nucleoli and scanty cytoplasm. On immunohistochemistry, the tumor cells were positive for chromogranin. Estrogen and progesterone receptors were negative as well as mammaglobin. Based on the pathological features and clinical history in conjunction with the immunohistochemical finding, the diagnosis of a metastasis of the esthesioneuroblastoma to the breast was made.
Our case highlighted the importance of clinical history and imaging features when dealing with a breast lump.
La metástasis en la mama de tumores extramamarios son muy poco frecuentes. La metástasis más frecuente es seguida de la leucemia, melanoma y linfoma. La metástasis mamaria de un estesioneuroblastoma olfatorio (ENO) es excepcional, encontrando en solo tres casos publicados. Presentamos un nuevo caso de metástasis en mama de un estesioneurbolastoma olfatorio con una revisión de la literatura. Paciente de 31 años con antecedentes de un ENO diagnosticada hace dos años tratada previamente con radiación y cirugía. La paciente refiere la aparición de una tumoración en el cuadrante superior de la mama derecha, de crecimiento progresivo e indoloro, apareció en el post-parto. A la exploración clínica se identifica dicha tumoración en el cuadrante superior interno de 3 cm de diámetro máximo y consistencia firme, sin alteraciones cutáneas ni del complejo aréola-pezón. La mamografía muestra numerosas zonas, mal delimitadas, de la mama derecha. Se le realiza una punción para biopsia aspiración con aguja fina. En el estudio anatomopatológico reporta una neoplasia neuroendocrina de aspecto uniforme con proliferación de células sin atipia con positividad inmunohistoquímica para cromogranina y negatividad para para receptores de estrógenos, progesterona y mammaglobin. La anatomía patológica definitiva reporta una metástasis mamaria del ENO.
Metastases to the breast from a non-mammary tumor are uncommon, accounting for 0.2–l.1°/o of all breast malignancies.1 Most of these tumors are part of a disseminated lymphoma or melanoma.2 Involvement of the breast with a metastatic esthesioneuroblastoma (ENB) is a very rare finding and only 3 cases are described in the literature.3–5 Herein, we present another case of mammary metastasis from an ENB and discuss the importance of a multidisciplinary approach when dealing with breast tumors.
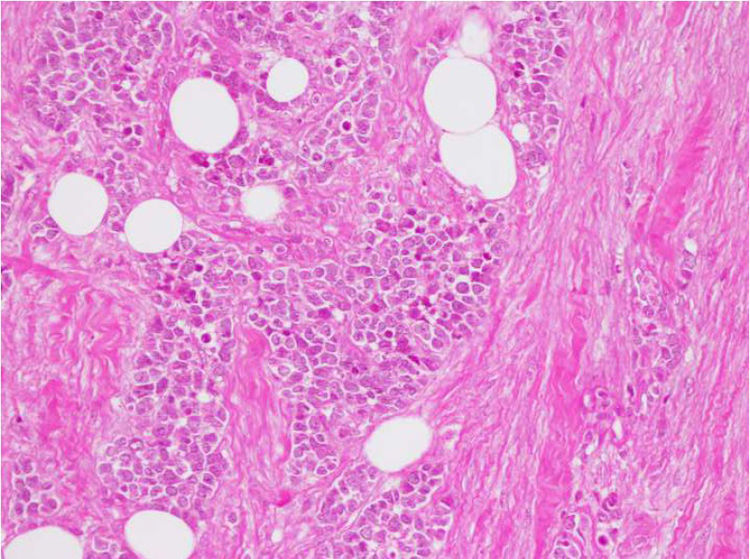
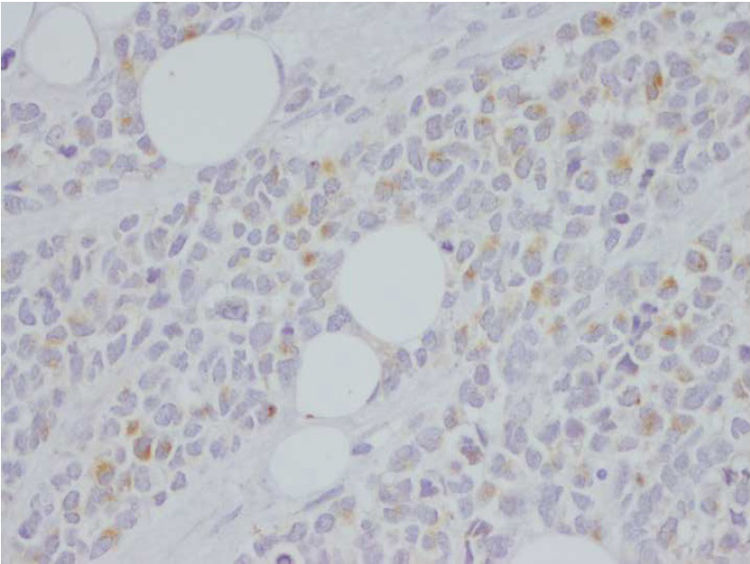
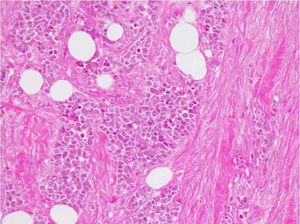
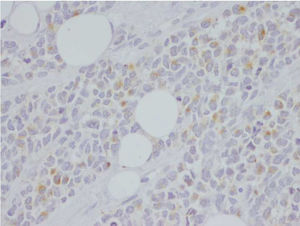
Clinical caseA 31 year old female, with a medical history of a Hyam's grade I olfactory neuroblastoma, confined to the nasal cavity and previously treated with surgery and radiotherapy was considered in remission since two years. She presented with a rapidly growing nodule of the right breast developed at two months after delivery. Physical examination revealed a palpable 3cm, firm nodule in the right upper inner quadrant, with no skin retraction and no nipple discharge. Breast ultrasound revealed multiple bilateral ill-defined multiple nodules, with irregular margins and heterogenous echogenicity. A fine needle aspiration biopsy of the largest nodule was performed. Pathological examination revealed nests and lobules of monotonous tumor cells with round uniform nuclei, indistinct nucleoli and scanty cytoplasm (Fig. 1). The mitotic index was very low. The stroma was hyalinized. Focal areas of necrosis and crash artifact were observed. The pathological features were clearly suggestive of a neuroendocrine origin. On immunohistochemistry, tumor cells were positive for chromogranin (Fig. 2). CD56 and synaptophysin were negative. Estrogen and progesterone receptors were negative as well as mammaglobin.
Considering the characteristic pathologic features suggestive of neuro-enodcrine/neuroectodermal origin, the positive staining for chromogranin, the negative staining for hormonal receptor and mammaglobin antibody and clinical history of ENB, the diagnosis of breast metastasis of the known ENB was made. Unfortunately, the patient denied the diagnosis and refused complementary imaging to assess extra-mammary tumor extension. Surgical removal of the right breast with adjuvant radiation therapy was considered; however the patient refused to consent for treatment. Six months later, she was admitted to our emergency department because of liver failure and seizures. She passed away within few days.
DiscussionENB is an uncommon malignant neuroectodermal tumor originating from the olfactory membrane of the sinonasal tract. There is male preponderance and mostly occurs in patients at the 5th or 6th decade.6,7 It is somewhat striking that all described cases in our paper occurred in young (20–31 years-old). Complete surgical resection followed by radiation therapy is the standard method of treatment. Chemotherapy is employed in patients with advance or recurrent disease. Local spread is not uncommon; however distant metastatic dissemination is rare mostly involving brain, lung and bone.6,7 Breast metastasis from ENB is extremely rare, to the best of our knowledge, only four cases (included ours) were reported in the literature (Table 1).3–5 The mean age of patients ranges from 3 to 90 years old. The average time for developing the metastasis varies from 7 to 24 months. Clinically, patients present with palpable rapidly growing lump. The tumor was right-sided in all cases. Imaging features may be confused with any benign or malignant primary neoplasm. They include: (a) a well-defined nodule with smooth border mimicking a benign lesion, (b) multiple irregular and diffuse lesions, (c) diffuse skin thickening.8 Magnetic resonance imaging (MRI) is useful in evaluating metastatic lesions to the breast. Such lesions may be single or multiple and circumscribed, round in shape. At MRI, most metastatic lesions show intermediate signal on T2 weighted sequences and low signal on T1 weighted sequences, with the exception of melanoma metastases, which may show high signal on T1 weighted images due to its melanin component. After administration of paramagnetic contrast, intense fast and homogeneous enhancement is usually observed, with a plateau or washout kinetic curve on the delayed phase.9 Fine needle aspirate of metastatic lesions may be contributive to diagnosis with cytological findings most similar to those seen in low-grade neuroendocrine carcinoma aspirates, with nests of somewhat monomorphic, fragile epithelioid cells with delicate chromatin and cytoplasm or show features similar to those seen in small cell neuroendocrine carcinoma in high grade tumors.6 On pathological examination, the most suggestive findings are: monotonous tumor cells population with round nuclei, indistinct nucleoli and salt and pepper chromatin typically set in a vascular-rich to hyalinized stroma. Fibrillary specialized neural matrix may be present. Homer Wright pseudorosettes and Flexner–Wintersteiner rosettes are highly suggestive of ENB. High grade tumors may show marked mitotic activity, nuclear pleomorphism and necrosis.6 The most widely used grading system for ENB is Hyams grading system which is typically made on primary tumors to prognosticate and guide treatment decisions. This system divides the spectrum of ENB maturation into four grades on the basis of tumor architecture, mitotic activity, nuclear pleomorphism, fibrillary matrix and rosettes, necrosis, gland proliferation, and calcifications. Metastatic ENB is often associated with high grade features. The typical immunohistochemical profile includes diffuse staining for neuronspecific enolase, synaptophysin, chromogranin A and CD56 as well as variable staining for PS100 which is typically in a sustentacular cell pattern. In our case, although only chromogranin positivity was found, based on the imaging features suggestive of a secondary tumor, the characteristic pathological findings reminding of neuroendocrine origin, the negative staining for hormonal receptor in conjunction with the patient's medical history, the diagnosis of a breast metastasis from the primary ENB was the most accurate.
Summarized clinical features of patients.
| Authors | Sex | Age | Treatment | Time from primary to metastasis | Breast lesion | Other metastasis | Survival | ||
|---|---|---|---|---|---|---|---|---|---|
| Side | Site | Size (mm) | |||||||
| Shetty et al.3 | F | 33 | Surgery+RT+CT | 12 months | Right | Unknown | Unknown | Bone+ovary | Death during radiation therapy |
| Larbcharoensub et al.5 | F | 30 | Surgery+RT+CT | 7 months | Right | Upper-Outer | 22 | Bone+lymph node+Lung | Death |
| Mrad K et al.4 | F | 20 | Surgery+RT+CT | 24 months | Right | Upper-Inner | 30 | Bone | Death |
| Reported case | F | 31 | No treatment | 22 months | Right | Upper-Inner | 35 | Unknown | Death |
F: female.
RT: radiotherapy.
CT: chemotherapy.
This reported case raises two concerns: one is related to the primary tumor which was of a low grade and confined to the nasal cavity suggesting that pathological Hyams grading and imaging staging alone are not sufficient stratification tools. Large sampling of the primary tumor is necessary for accurate grading; mitotic activity should be clearly estimated and reported as well as Ki67 proliferative index. However, it is essential that we focus on other immunhistochemical or molecular biomarkers for more accurate prognostic approach. The young age of patient with ENB metastases to the breast may be correlated to more aggressive potential of the primary tumor. However, this need to be confirmed through more case report publications.
The second issue in this report is the importance of clinical history and imaging features in pathological examination. Indeed, one should always keep in mind the possibility of breast metastasis when dealing with mammary malignancies. Pathologist should always ask for patient's history of another malignancy elsewhere and discuss the imaging findings and suspected diagnosis with radiologist. But above all, consider the possibility of a secondary breast lesion when histological features are not reminding of primary specific tumor.
Unfortunately, in our reported case, treatment protocol could not be discussed because the patient denied her disease and refused to consent for treatment and radiologic explorations. The psychological impact of the disease should also be of concern so that we avoid “therapeutic abandonment”.
ConclusionMetastases to the breast from non-mammary malignancies are rare and may be confused with a primary tumor. Combination of the patient's clinical history, pathological findings and the immunohistochemical results are necessary for accurate diagnosis. It is important we continue publishing these rare case reports so that we collect more data concerning clinical and pathological features of such metastasis in order to have a more codified management of the disease.
FundingThis work has not received any funding.
Ethics approval and consentObtained (from the husband).
Conflict of interestThe authors declare that they have no conflict of interest.