A hospital legal medicine department, to advice and consult on the legal, ethical and deontological aspects of healthcare practice, has been implemented in our centre, Hospital Clínico San Carlos (Madrid, Spain). A simple service portfolio based on the prevention of legal risks, has allowed professionals, health service and patients to place their trust in it.
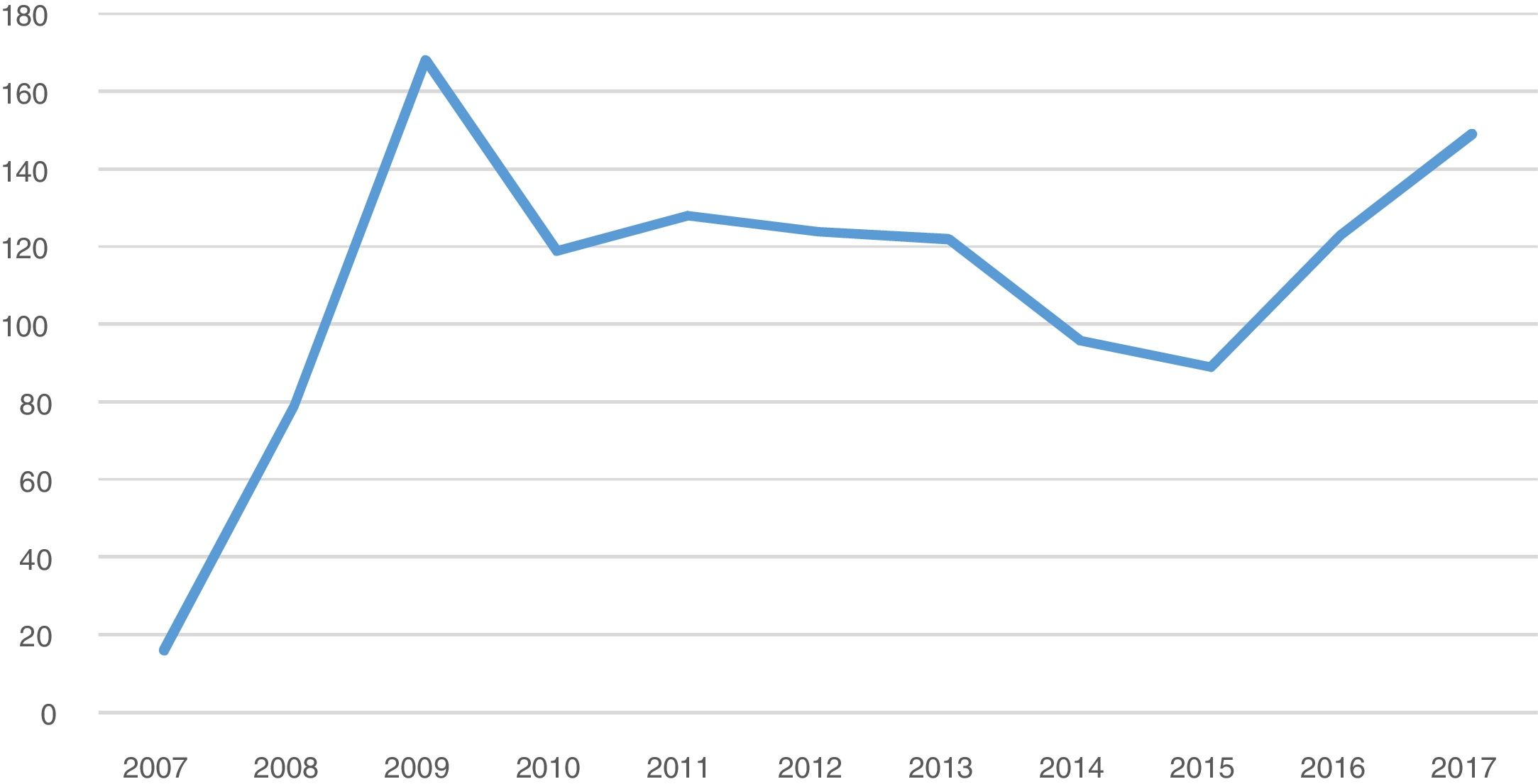
ResultsThe number of cases over the period 2007–2017 reflects major activity, and 2009 and 2017 are highlighted with 13.8% and 12.3% of the total activity respectively. The units that consulted the most were the management team 158 (13%), the Institute for Women's Affairs 144 (11.9%) and the Patient Care Service 116 (9.6%).
Discussion and conclusionsThe department participates in multiple committees and working groups preparing guidelines, documents and protocols, addressing conflicts, regulatory doubts, training deficiencies, recommending courses of action, and mediating with patients and family members to reduce professional uncertainty.
La implantación de un Servicio de medicina legal hospitalaria, como asesor y consultor en aspectos médico-legales, éticos y deontológicos de la práctica asistencial, se ha consolidado en el Hospital Clínico de San Carlos de Madrid. Una cartera de servicios sencilla basada en la prevención de riesgos legales, ha permitido que los profesionales, la administración sanitaria y los propios pacientes confíen en él.
ResultadosEn el período 2007-2017 se gestionaron 1.213 expedientes, aumentando de forma progresiva y destacando los años 2009 y 2017 con un 13,8 y 12,3% de la actividad total, respectivamente. Las unidades que más consultaron fueron el equipo directivo 158 (13%), el Instituto de la Mujer 144 (11,9%) y el Servicio de Atención al Paciente 116 (9,6%).
Discusión y conclusionesEl servicio participa en múltiples comisiones y grupos de trabajo elaborando guías, documentos y protocolos, abordando conflictos, dudas normativas, deficiencias formativas, recomendando cursos de acción, e intermediando con pacientes y familiares para disminuir la incertidumbre del profesional.
The creation of the legal medicine service in the Hospital Clínico de San Carlos in Madrid in 1983 and the appointment of a forensic medicine professor to this centre,1 provided a solution to a need by professionals to obtain advisory and consultation services in legal medical, deontological and ethical matters and at the time was a major novelty on a national level. Similar services were also created in the Hospital Puerta de Hierro in Madrid, Hospital Valle de Hebrón in Barcelona and Reina Sofía in Murcia with a similar intent.
The medico-legal aspects of healthcare2 affect a cross-section of all areas, including any medical specialty and of course any professional action, be it by healthcare staff or otherwise.
Over this period, the advisory and consultancy services have become practically essential. In daily practice we see how doctors are very frequently immersed in medico-legal problems, and which also occasionally affect medical students who are initiating their profession.3 The most common conflictive situations are complaints regarding malpractice (due to carelessness or negligence), problems with diagnosis or treatment and problems derived from an inappropriate doctor-patient relationship. Lack of familiarity with legal regulations and ethical principals in medical practice do not exempt us from liability in the face of courts or society.
With the upgrading of the legal medicine hospital service in 2007 following the retirement of the person in charge, a new stage was initiated which focused on the “Prevention and Management of Medico-Legal Risks”,4 on the understanding that prevention should be the philosophy around which all lines of action in medico-legal aspects of healthcare should be built. The service is also working closely with the hospital's patient safety strategy and management of healthcare risks, providing support from a medico-legal viewpoint, as other authors have already reported.5
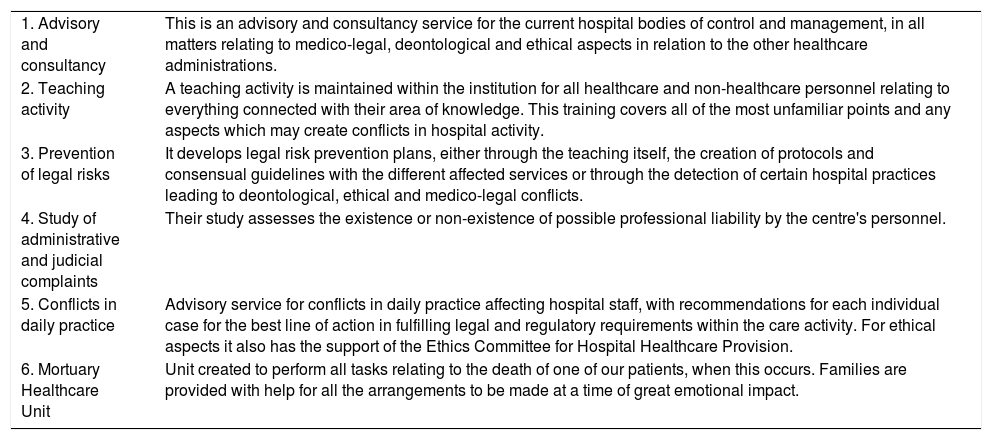
The list of easily implemented services (Table 1) is an attempt to bring to the attention of the professional and management team an area of previously unexplored knowledge.
List of hospital legal medicine services.
| 1. Advisory and consultancy | This is an advisory and consultancy service for the current hospital bodies of control and management, in all matters relating to medico-legal, deontological and ethical aspects in relation to the other healthcare administrations. |
| 2. Teaching activity | A teaching activity is maintained within the institution for all healthcare and non-healthcare personnel relating to everything connected with their area of knowledge. This training covers all of the most unfamiliar points and any aspects which may create conflicts in hospital activity. |
| 3. Prevention of legal risks | It develops legal risk prevention plans, either through the teaching itself, the creation of protocols and consensual guidelines with the different affected services or through the detection of certain hospital practices leading to deontological, ethical and medico-legal conflicts. |
| 4. Study of administrative and judicial complaints | Their study assesses the existence or non-existence of possible professional liability by the centre's personnel. |
| 5. Conflicts in daily practice | Advisory service for conflicts in daily practice affecting hospital staff, with recommendations for each individual case for the best line of action in fulfilling legal and regulatory requirements within the care activity. For ethical aspects it also has the support of the Ethics Committee for Hospital Healthcare Provision. |
| 6. Mortuary Healthcare Unit | Unit created to perform all tasks relating to the death of one of our patients, when this occurs. Families are provided with help for all the arrangements to be made at a time of great emotional impact. |
The total number of open files during the 2007–2017 periods was 1,213. With regard to the activity developed by the service, there was a notable increase in activity in 2009 and 2017 at 13.8% and 12.3%, respectively (Fig. 1). This increase does not respond to any factor which we have been able to discern, since it does not respond to organizational or functional service affairs.
The files were classified according to the main reason for consultation (since they frequently appear combined), with the most frequent medico-legal cause (1,109 cases 91.4%), followed by ethical (62 cases 5.1%) and deontological (42 cases 3.4%). The most common causes for consultation were questions referring to patient autonomy, the ability to make decisions, clinical documentation, data protection and professional responsibility requesting professionals to have integral consultancy to provide responses both to purely administrative claims and those of a judicial nature.
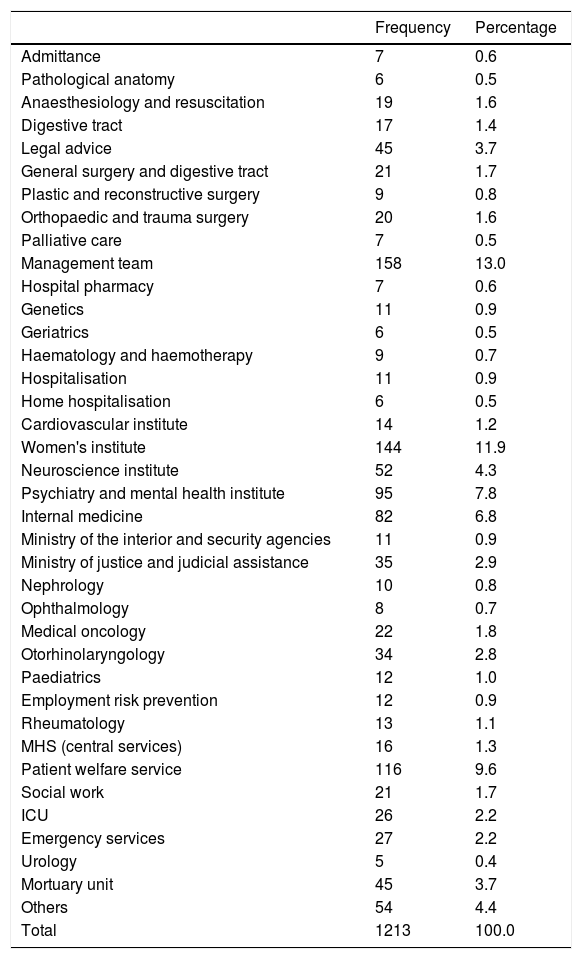
With regard to services and units that carried out consultancy, distribution may be found in Table 2, where the management team with 158 (13%), the institute for Women's affairs with 144 (11.9%) and the Patient Care Service with 116 (9.6%) were of note.
Service or unit requesting advice by alphabetic order.
| Frequency | Percentage | |
|---|---|---|
| Admittance | 7 | 0.6 |
| Pathological anatomy | 6 | 0.5 |
| Anaesthesiology and resuscitation | 19 | 1.6 |
| Digestive tract | 17 | 1.4 |
| Legal advice | 45 | 3.7 |
| General surgery and digestive tract | 21 | 1.7 |
| Plastic and reconstructive surgery | 9 | 0.8 |
| Orthopaedic and trauma surgery | 20 | 1.6 |
| Palliative care | 7 | 0.5 |
| Management team | 158 | 13.0 |
| Hospital pharmacy | 7 | 0.6 |
| Genetics | 11 | 0.9 |
| Geriatrics | 6 | 0.5 |
| Haematology and haemotherapy | 9 | 0.7 |
| Hospitalisation | 11 | 0.9 |
| Home hospitalisation | 6 | 0.5 |
| Cardiovascular institute | 14 | 1.2 |
| Women's institute | 144 | 11.9 |
| Neuroscience institute | 52 | 4.3 |
| Psychiatry and mental health institute | 95 | 7.8 |
| Internal medicine | 82 | 6.8 |
| Ministry of the interior and security agencies | 11 | 0.9 |
| Ministry of justice and judicial assistance | 35 | 2.9 |
| Nephrology | 10 | 0.8 |
| Ophthalmology | 8 | 0.7 |
| Medical oncology | 22 | 1.8 |
| Otorhinolaryngology | 34 | 2.8 |
| Paediatrics | 12 | 1.0 |
| Employment risk prevention | 12 | 0.9 |
| Rheumatology | 13 | 1.1 |
| MHS (central services) | 16 | 1.3 |
| Patient welfare service | 116 | 9.6 |
| Social work | 21 | 1.7 |
| ICU | 26 | 2.2 |
| Emergency services | 27 | 2.2 |
| Urology | 5 | 0.4 |
| Mortuary unit | 45 | 3.7 |
| Others | 54 | 4.4 |
| Total | 1213 | 100.0 |
MHS: Madrid Health Service; ICU: intensive care unit.
For somewhat over 10 years the service has borne fruit and successfully established a climate of trust for those requesting advice, whether they be healthcare or non-healthcare professionals of many different services and units. The prevention of legal risks, as a general service strategy, means that regular risk manoeuvres may be identified in both clinical practice and doctor-patient relationships, and mechanisms have been put into place which minimize the medico-legal uncertainty often facing the profesional.6
Inclusion in numerous working groups has led to the ability to coordinate or collaborate in the creation of different guides, manuals and protocols which are of great use in the activity of the institution. Several of these documents have served as references for the Madrid Health Service and even on a national level.7,8
The incorporation into multiple hospital commissions or committees (Commission against Violence, Information Security Committee, Documentation Commission, new Products Commission, Ethical Committee for Healthcare, Innovation Committee, Training Commission, Governing Board) has led to a complementary vision and even guarantee of certain aspects of healthcare. For example, of note is the close relationship with the commission charged with patient safety, and the health risk management (Functional Unit of Healthcare Risk Management), although with highly differentiated competences, due to the important medico-legal implications which this activity encounters, particularly in several care areas, such as the emergency services, the intensive care unit or the maternal and child areas.9 Collaboration with other health institutions has also been significant during this period. Our hospital has thus been able to establish useful mechanisms of cooperation (such as that established with the National Institute of Toxicology and Forensic Sciences, for analysis on suspicion of chemical submission).
Another aspect to emphasize is the confidence afforded to healthcare staff by the provision of a medico-legal service to treat relatively frequent and conflictive situations, such as the rejection by certain collectives of certain treatments,10 to dispel doubts regarding regulatory framework, to compensate for several training deficiencies or even facilitate communication with patients and family members for the resolution of conflicts.
The Medico-Legal Service is perceived by professionals of the centre as a trustworthy advisory service, with no intention to control and the main objective of which is to help overcome the obstacles and uncertainties in legal, ethical and deontological aspects which continuously arise in the health service.
Lastly, anticipation of modification of Royal Decree 1277/2003, of 10th October, by which the general bases on authorization of centres, services and healthcare establishments are established, intends to extend the healthcare offered by health centres to include a new unit, the “U.102. Legal and forensic medicine”, defined as the “healthcare unit in which a doctor/specialist in legal and forensic medicine is responsible for providing technical assistance to the bodies for control and management of a health centre, in everything relating to the medico-legal, deontological and ethical aspects of the centre and the other healthcare administrations”. An opportunity therefore arises to create new services or units which drive healthcare quality through the prevention and management of medico-legal risks and which will count on the support and collaboration of a consolidated service such as ours. Furthermore, these services may become reference units for the training of new specialists in legal and forensic medicine which are to be incorporated into the upcoming appointments for resident doctors.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Santiago-Sáez A, Perea-Pérez B, Olivares Pardo E, Pinto Pastor P, García Martín AF. Actividad de un Servicio de Medicina Legal Hospitalaria del siglo XXI. Rev Esp Med Legal. 2020;46:71–74.