Spain is one of the countries most affected by the COVID-19 pandemic. To date, 22% of reported cases are healthcare professionals, and 76% of them are women. Given that many healthcare professionals may have been infected in their workplace, we have reviewed the occupational health challenges posed by COVID-19. The Spanish laws and the recommendations of the International Labor Organization are described. The review covers the classification of SARS-CoV-2 as a biological agent in group 3 and of COVID-19 as an occupational accident or disease, its repercussions in temporary and permanent disabilities, sequelae and death, and the possible claims of those who may have developed the disease due to the lack of preventive measures.
España ha sido uno de los países con mayor afectación por la pandemia COVID-19. Hasta la fecha, un 22% de los casos notificados son personal sanitario, siendo significativamente mayor este porcentaje entre las mujeres (76% del personal sanitario contagiado). Ante la evidencia de que muchos profesionales sanitarios pueden haberse contagiado en su puesto de trabajo, hemos revisado la problemática en el ámbito de la salud laboral que produce el COVID- 19. Se describen los decretos publicados por el Gobierno de España y las recomendaciones de la Organización Internacional del Trabajo. Concretamente se analiza la clasificación del SARS-CoV-2 como agente biológico del grupo 3 y su calificación como accidente de trabajo o enfermedad profesional, y sus repercusiones en las situaciones de incapacidades (temporales y permanentes), secuelas y muerte; así como el estudio de las posibles demandas de aquellos que lo han sufrido como consecuencia de falta de medidas preventivas.
At the end of December in the year 2019 a group of patients were admitted to different hospitals in Wuhan, the capital of Hubei province in the centre of China, with an initial diagnosis of pneumonia with an unknown aetiology. Subsequently, on 7 January 2020 the Chinese authorities identified the first cases of a new disease cause by coronavirus (COVID-19). The origin was detected in the wild animal market of Wuhan. It is thought that the origin of the disease was probably transmission by a yet to be determined mammal to humans. The winter, the influenza season and the ceaseless movement of the population in a globalised world all additionally favoured the spread of SARS-CoV-2 around the whole planet, giving rise to an enormous health crisis.1–3
On 30 January 2020, the World Health Organisation (WHO) declared the outbreak of COVID-19 to be an internationally worrying public health emergency,4 and it officially declared it to be a pandemic on 11 March 2020. Infection by SARS-CoV-2 (COVID-19) seems to cause a wide range of symptoms.5–7 The majority of deaths occur in older adults, many of whom have chronic underlying diseases.8
According to Ministry of Health (MH) data, on 4 May 2020 219,329 confirmed cases have been reported in Spain, with 25,613 deaths. The Autonomous Community of Madrid has had the highest number of cases (62,989), and these figures are rising day by day. According to MH data of 7 May 2020, 22% of the cases reported to the SIVIES (the Spanish monitoring system of the National Epidemiological Centre) correspond to medical personnel, and this percentage is significantly higher for women than it is men (29.1% vs. 11.7%). 76% of medical personnel with COVID-19 are women.8,9
As this disease is infectious-contagious it affects many medical professionals who are in direct contact with COVID-19 while treating patients. Our work has the aim of reviewing the problem which arises in the field of professional health due to COVID- 19. More specifically we analyse its repercussions in the context of healthcare work and most especially in terms of the temporary disabilities (TD), permanent disabilities (PD), sequelae and death, as well as studying lawsuits that could possibly be initiated by those who have suffered as the result of a lack of preventive measures.
Evaluation of temporary disability caused by COVID-19Initially, all of the TD caused by COVID-19 are considered to be common diseases (CD) according to the definitions established by Royal Decree-Law 6/2020, of 10 March, which adopts certain urgent measures in the economic field and to protect public health. Art. 5 of this Law states that “exceptionally, those periods of isolation or contagion of working people caused by the COVID-19 virus will be considered to be industrial accidents, exclusively for the economic compensation of temporary disability in the Social Security system”10.
Subsequently, Royal Decree-Law 13/2020, of 8 April 2020,11 in its first final Regulation, modifies article 5 of Royal Decree-Law 6/2020. As well as generally keeping the consideration of periods of isolation, contagion or restriction of movement outside a municipality as an exceptional situation assimilated under the heading of an industrial accident (IA), this adds the possibility of classification as an IA when it is proven that the disease was caught exclusively while working under the conditions set by article 156 of the rewritten text of the General Social Security Law,12 in which case it will be classified as an IA.
We believe that the situation of infected workers who have been in contact with individuals infected with COVID-19 in their work or suspect that they have been, this should be classified as an occupational disease (OD). This is obvious in the case of medical workers, as is shown by the high percentage of healthcare professionals infected reported in epidemiological monitoring records. 65% of medical professionals had the risk of contact with persons with respiratory infection as an epidemiological antecedent, and 69% had been in close contact with probable or confirmed cases of COVID-19.9
The definition of OD established by Legislative Royal al Decree 8/2015 should be remembered, where it says in art. 157 that “OD will be understood to refer to one contracted as the result of work executed for an employer in the activities specified in the table approved by the applicable regulations and developed by this law, and which is caused by the action of elements or substances which are shown in the said table for each occupational disease”, although it also defines OD for self-employed workers in art. 316, where it says that “Occupational disease will be understood to refer to one contracted as the result of work executed by a self-employed workers that is caused by the action of elements and substances and in the activities specified in the list of occupational diseases with the list of the main activities capable of causing them”.
The reasons why it must be an OD for employed workers and self-employed ones (on condition that they pay contributions for this reason), are as follows:
- a)
This is an Appendix 1 pathology, according to the clear stipulations of Royal Decree 1299/2006, of 10 November, which approved the table of occupational diseases (OD) caused by biological agents (Table 1). It literally states: “Infectious diseases caused by the work of persons who are employed in prevention, medical treatment and activities in which a risk of infection has been proven (excluding the microorganisms included in group 1 of R.D. 664/1997, of 12 May, regulating the protection of workers against risks associated with exposure to biological agents while working.”13
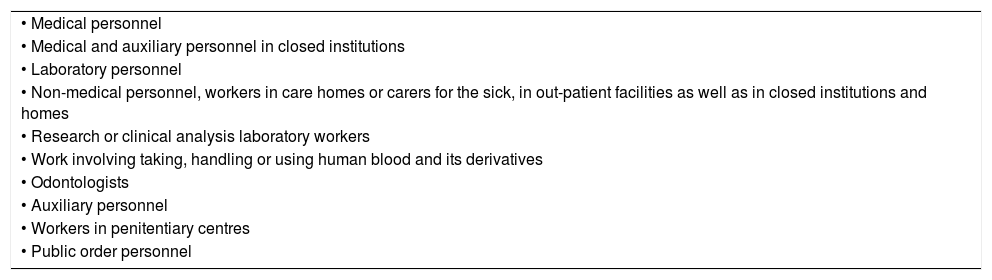
Table 1.Royal Decree 1299/2006, of 10 November, approving the table of occupational diseases.14
• Medical personnel • Medical and auxiliary personnel in closed institutions • Laboratory personnel • Non-medical personnel, workers in care homes or carers for the sick, in out-patient facilities as well as in closed institutions and homes • Research or clinical analysis laboratory workers • Work involving taking, handling or using human blood and its derivatives • Odontologists • Auxiliary personnel • Workers in penitentiary centres • Public order personnel - b)
When they have to issue a medical certificate for sick leave, it is an obligation for family doctors in the National Health System, in compliance with the stipulations of art. 5 of Royal Decree 1299/2006, of 10 November, which approved the table of occupational diseases, as it states “When National Health System doctors, while acting professionally, learn of the existence of a disease included in Appendix 1”… “they are to report this for applicable purposes through the competent body of each autonomous community and the cities with a Statute of Autonomy, to the managing entity, for the purposes of classification defined as criteria to be classified as an OD”.
- c)
Royal Decree 1299/2006 on the protection of workers against the risks associated with exposure to biological agents14 specifies that this classification corresponds to the jobs defined in Table 1, although this list is neither exhaustive nor closed, but rather may be extended to cover other jobs according to the Sentence of the Supreme Court.15
- d)
To be considered an OD, a condition is that the pathology which affects the workers is not one of the pathologies corresponding to microorganisms included in group 1 of the classification of biological agents established by Royal Decree 664/199714 (Table 2) (Table 3).
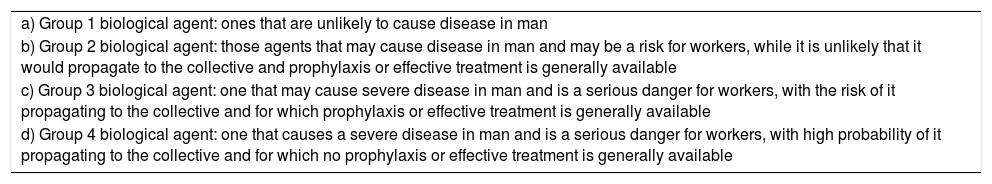
Table 2.Classification of biological agents according to Royal Decree 664/1997.16.
a) Group 1 biological agent: ones that are unlikely to cause disease in man b) Group 2 biological agent: those agents that may cause disease in man and may be a risk for workers, while it is unlikely that it would propagate to the collective and prophylaxis or effective treatment is generally available c) Group 3 biological agent: one that may cause severe disease in man and is a serious danger for workers, with the risk of it propagating to the collective and for which prophylaxis or effective treatment is generally available d) Group 4 biological agent: one that causes a severe disease in man and is a serious danger for workers, with high probability of it propagating to the collective and for which no prophylaxis or effective treatment is generally available Table 3.Differences between common disease, industrial accident and occupational disease.
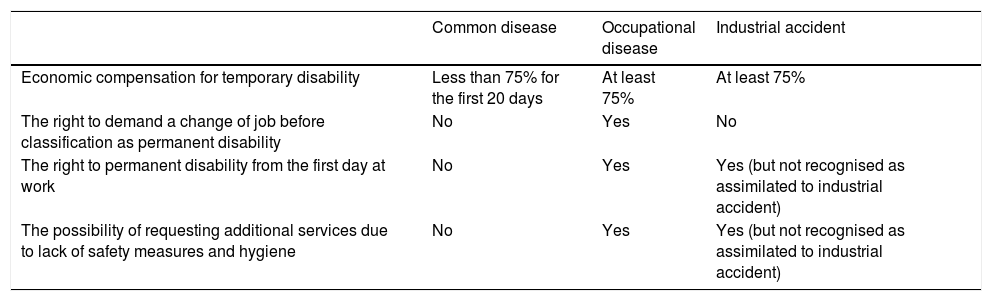
Common disease Occupational disease Industrial accident Economic compensation for temporary disability Less than 75% for the first 20 days At least 75% At least 75% The right to demand a change of job before classification as permanent disability No Yes No The right to permanent disability from the first day at work No Yes Yes (but not recognised as assimilated to industrial accident) The possibility of requesting additional services due to lack of safety measures and hygiene No Yes Yes (but not recognised as assimilated to industrial accident)
The family of coronaviruses was generally included in group 2. The difference between groups 2 and 3 is that those in group 3 place workers in “serious danger”, while those in group 2 only place them in “danger”. In the specific case of the COVID-19 pandemic, based on our current knowledge we believe it should be considered to be a “serious danger”, which would therefore correspond to group 3. Another difference between groups 2 and 3 is the risk that infected workers may propagate the disease to the collective (a public health risk). Group 3 must be considered to be “with a risk of propagation to the collective”. We believe that SARS-CoV-2 would now belong to group 3, as is shown by the lockdown measures and social distancing that have been applied. Group 4 covers those for which there is no prophylaxis or effective treatment. We consider that COVID-19 should belong to group 3, given that although there is now no clearly effective treatment, prophylaxis does exist. The Polytechnic University of Valencia protocol also catalogues it as belonging to the said group 3.16
Prophylaxis in the case of the pandemic caused by SARS CoV-2 consists of the isolation of infected individuals, the use of personal protective equipment (PPE) such as masks, gloves, hand washing and distancing from other people, etc. 17 Unfortunately, there is now no specific vaccine against the COVID-19 virus, and treatment consists of support plus antiviral drugs and other medication, without any clear benefit having been found to date. Some drugs have been shown in phase I to inhibit viral replication in infected cells18 and the multinational company Grifols has commenced the identification, screening and selection of donors who have recovered from COVID-19 so that they can donate plasma to produce a hyperimmune antiSARS-CoV-2 immunoglobulin that, if it is effective, could be used to treat the disease.19
Thus definitively, we believe that SARS-CoV-2 should be classified as a group 3 and not group 4 biological agent, as there is prophylaxis against exposure to it that prevents contagion. However, it is not indispensible to belong to group 3 to be classified as an OD (from which only group 1 diseases are excluded, as we pointed out). Thus as group 2, 3 or 4 it may be an OD, although it should not be a common disease or even an IA for medical personnel.
There are many differences for workers between being in a TD situation due to a professional contingency (IA or OD) or due to a common disease (CD),20 which was the contingency initially established for granted medical leave to individuals infected by COVID-19 or with the suspicion of this. IA has only been considered when it has been proven that transmission of the disease occurred with an “exclusive cause” in the performance of work, which it is often quite difficult to do. Thus the assimilated situation of IA exclusively due to the economic compensation of TD involves certain advantages over CD, including:
- a)
Compensation of at least 75% from the first day of medical leave.
- b)
Access to the said economic compensation for workers who have paid contributions during at least 180 days in the previous years, and who usually do not receive payment during time off work because of a CD.21
However, in cases in which it is classified as an IA, this would have greater advantages, such as:
- a)
Leave due to IA cannot be counted for objective dismissal due to absenteeism (although it is a reason for dismissal that will soon be annulled).
- b)
Consideration of IA would lead to a possible PD, sequelae or compensation for death, without demands of any period of paying contributions.
However, it will almost always be difficult to gain recognition of an IA, as this has to be “with an exclusive cause in the performance of work”. This is simpler when it is the result of trauma that occurred in the context of work, but in practice it is very hard to prove that a virus was exclusively present while working and not in the street or while using public transport.
Classification as OD, which we consider should be when contact has occurred at work with persons infected with COVID-19, will have an additional advantage for workers even greater than corresponds to an IA. This is the right to change jobs, which does not exist in the case of IA. Table 2 shows the differences between CD, OD and IA.
Classification as OD for those professionals who have been in contact with patients with COVID-19 and who are exposed to contagion and in isolation would allow their medical leave to be defined as “a period of observation of OD, while confirmation or not of the said situation is awaited”.
Evaluation of permanent disability, sequelae and death due to COVID-19When PD results from having suffered COVID-19 infection, it is obvious that there will always be the right to economic compensation for the said disability. Although economic payment for TD will consider it to be classified as an IA, this circumstance is not recognised for PD, unless it is classified as an IA when it is proven that the disease was caught due to a cause exclusively associated with the performance of work.
This lack of recognition of PD for this situation of assimilation in IA means that, unlike IA in which all workers have the right to this from the first day at work, when CD is considered a period of paying contributions is necessary to be able to access PD compensation (and this is almost always longer than five years).
Nor will there be the right to compensation for non-invaliding sequelae deriving from COVID -19 for causes assimilated to IA, as this compensation is exclusively for IA and OD.
Nevertheless, there is the right to PD from the first day of work for non-invaliding sequelae, if it is recognised to be an IA or OD. These circumstances are important as it is not known how many individuals infected by COVID-19 will eventually have sequelae or a PD.
Classification as an OD will have greater advantages for the worker than would be the case for an IA, due to the right to change jobs. A worker who is unable to perform his professional activity in a company due to an OD will have the right to be assigned to another job by the company owner, with the same salary (on condition that such a compatible job exists). This is not the case for IA, where the worker may commence to receive compensation for PD amounting to 55% or the maximum of 75%.
Countries such as Germany and Italy recognise workers infected by COVID-19 while doing their job as a case of OD. On 28 April the general journal “Redacción Médica” published a new item on the World Health Organisation (WHO)22 and the International Labour Organisation (ILO) warning that health workers infected by COVID-19 after exposure in their place of work should have the right to benefits due to occupational injuries caused by OD, including compensation, rehabilitation and curative services.23
In Italy, the National Institute of Industrial Accident Insurance (Istituto Nazionale per l'Assicurazione contro gli Infortuni sul Lavoro - INAIL) has confirmed that infection by coronavirus of doctors, nurses and other National Health Service (Servizio Sanitario Nazionale - SSN) employees, as well as those of other public and private hospitals is considered to be an OD. For this group of employees, the causal link between their work and infection is assumed automatically, with the aim of offering coverage to cases where it is problematic to determine the specific causes and how working methods connect with the infection. Additionally, the INAIL also applies this principle to COVID-19 cases in which infection by the SARS-CoV-2 virus occurred while travelling to or from work.24
In Spain it has always been very difficult to gain recognition of an OD, in administrative as well as in judicial terms. The OD which are reported are a minimum percentage of those which actually arise.25 However, there is no obstacle due to current regulations against a judge being able to recognise infection by COVID-19 as an OD. What the judge cannot do is to add to the OD which are listed in Royal Decree 1299/2006, as modification of the table of OD corresponds to the Ministry of Work and Social Matters and would require the previous report of the Ministry of Health and Consumption and the National Commission of Health and Safety at Work. However, as COVID-19 is a group 3 infection, it is expressly recognised as an OD in Appendix 1 of Decree 1299/2006.
The possibility of claims or lawsuits due to suffering infection by COVID-19 because of the lack of safety measures or hygieneIf workers who have suffered a COVID-19 (SARS-CoV-2) infection and have TD due to a situation accepted as an IA consider this to have been caused by a lack of Safety measures or Hygiene, or due to a lack of preventive measures (PPE), they do not have the option of claiming compensation from the administration because of field because of the said lack of safety measures and hygiene, as this TD has been granted “exclusively for the economic compensation of disability”; in these cases they would have to claim beforehand for what is considered to be an industrial contingency (whether it be an IA or an OD), unless it had been classified always “as an IA when the contagion of the disease is proven to have been contracted exclusively when working”.
Only in the case that one of the causes of TD is due to and IA or an OD and if this is the consequence of a lack of safety or protective measures by the business owner, all of the economic compensations that may derive from the IA or OD (whether it be a TD or a PD) will increase depending on the severity of the infraction by 30 per cent to 50 per cent.26 The responsibility for payment lies directly with the company which committed the infraction and it may not be covered by any insurance. This responsibility for payment of this addition to Social Security services is independent and compatible with responsibilities of another type, penal or civil, that may derive from the infraction.
The Provincial Board of the National Social Security Institute is competent to administratively declare and determine the responsibility for surcharging for the services of the SS and the scope of the additional services, after a report by Work Inspection. If the company owner or the worker does not agree, they may have recourse to judicial means before the court of Social matters.
We consider the number of claims of this type due to lack of safety measures and hygiene at work to be extremely high, as well as possible lawsuits in the Social and Civil fields or reports in the Penal field, especially in cases of death, where the standard set by Law 35/201527 would often be used to calculate compensation.
Conclusions1. We consider the Modification of Royal Decree-Law 6/2020 to be correct and relevant where it introduces the possibility of contracting the disease to be classified as an IA when it is proved that this took place exclusively while working. Nevertheless, we consider it to be insufficient, as the term “exclusive cause” restricts the possibility of recognition and it would often be impossible if strictly applied by insurance companies, as this is designed for other causes (such as trauma) and not for an infection.
2. The correct classification for those workers who may have been infected in their workplace or who may have been exposed to infected persons would be the case for an OD, as is established by a Supreme Court Sentence, which states that it may expand to cover more jobs that those shown in the risk groups of Table 1.
3. The condition of being an OD has some advantages for the affected workers, as they are superior to those of an IA, as in cases of PD it permits a change of job within the same company at the same salary, and this is obligatory for the company owner.
4. This concept of OD for those who have been infected by SARS-CoV-2 is the one that is used by the majority of countries for workers who have been infected with the disease (COVID-19) in their workplace. The ILO and the WHO have warned that health workers infected by COVID-19 after exposure in the workplace should be considered to be affected by an OD.22,23
5. We appreciate the fact that there is a clear option for requested additional services due to the lack of safety measures and hygiene in those jobs where there has been a lack of personal protective equipment (PPE) or an insufficiency in the same.
6. The possibility exists of an extremely high number of claims which could lead to the request for additional services that may terminate in Social jurisdiction, especially in cases of PD or death due to COVID-19. This is also the case for lawsuits in Civil and Penal Courts that we believe may surpass the possibilities of the Courts if no change in the law is made.
7. The WHO has warned that health workers infected by COVID-19 after exposure in the workplace should have the right to benefits for industrial injuries caused by OD, including compensation, rehabilitation and medical services. To evaluate whether COVID-19 is an OD it is fundamental to have exact and transparent criteria to determine whether the SARS-CoV-2 biological agent is able to cause COVID-19 in medical workers, and the final decision lies in recognising the cause of the disease and the workplace.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Martí-Amengual G, Sanz-Gallen P, Arimany-Manso J, Valoración medicolegal de la infección por COVID-19 en el ámbito laboral. Rev Esp Med Legal. 2020;46:146–152.