Non-suicidal self-injury (NSSI) is the deliberate and self-inflicted damage to body tissue in the absence of fatal intent, and has become a serious health problem among adolescents. The aim of this study was to evaluate the efficacy of treatment for NSSI in this population through a systematic revision and meta-analysis (PROSPERO ID: 252355). Studies with therapies that reduced NSSI were included. The search was performed in the Medline, APA PsycINFO and PubPsych databases. The synthesis of measures for the main outcome (NSSI reduction) and for secondary outcomes (global functioning change and depressive symptomatology reduction) was performed using a random effects model. The search identified a total of 1881 studies. The systematic review included five studies and the meta-analysis four studies. The summary effect estimate for the standardized mean difference in NSSI was −0.53 (95% CI: −0.82, −0.25), in global functioning it was 0.62 (95% CI: 0.34, 0.91), and in depressive symptomatology it was −0.59 (95% CI: −0.82, −0.36). The certainty of the evidence using the GRADE method is low. We conclude that therapies specifically aimed at reducing NSSI are effective in reducing both NSSI and depressive symptoms while increasing global functioning.
The International Society for the Study of Self-Injury1 defines non-suicidal self-injury (NSSI) as deliberate and self-inflicted damage to body tissue for nonsocioculturally sanctioned purposes. This implies that the self-harm resulting from the action is an intentional consequence, that self-injury is separated from suicidal thoughts or behaviors, so there is no intention of causing death, and that it excludes conduct that does not result in injury, even though it is harmful or dangerous. The recent text revision of the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR)2 has incorporated ICD-10-CM codes for suicidal behavior and for NSSI. It considers suicidal behavior to characterize individuals who have engaged in potentially self-injurious behavior with at least some intent to die as a result of the act, while NSSI characterizes individuals who have engaged in intentional self-inflicted damage to their body that is likely to induce bleeding, bruising, or pain (for instance, by cutting, burning, stabbing, hitting, or excessive rubbing) in the absence of suicidal intent. It is accepted that one of the most frequent motivations for conducting NSSI is to relieve negative emotions.3 NSSI can be considered a type of self-harm, which is a broader term that includes intentional self-poisoning or self-injury regardless of degree of suicidal intent or other types of motivation. A systematic review of the relationship between NSSI and suicidal behavior concluded that both share risk factors, are statistically correlated, and seem to be behaviors on a single continuum of self-injury; however, NSSI appears to be a risk factor predictive of subsequent behavior, as if the capability to commit suicide could be developed through NSSI.4
NSSI behavior is a serious problem that often starts in adolescence. An international study estimated that the prevalence of NSSI in this age group is 18%,5 and the Working Group created to review the Clinical Practice Guideline for prevention and treatment of suicidal behavior states that the prevalence of NSSI is highest in this life stage.6 This could be explained by the fact that this is a crucial developmental stage in which important changes occur at the psychological, biological and social levels. Adolescence is also a time of increased emotional reactivity, which may play a role in the higher incidence of affective disorder onset and addiction during this developmental period.7 This could also affect the development of NSSI,8 especially when there are feelings of hopelessness.9
Regarding factors associated with its appearance in adolescents, a recent review and meta-analysis identified seven categories, namely adverse childhood experiences, low health literacy, mental disorders, bullying, problem behaviors, female gender and physical symptoms.10 The category ‘adverse childhood experiences’ combines the negative impact of family, school and society on adolescents and includes lower socioeconomic status and psychological functioning of the family. Family is one of the first environments that provides physical, psychological and social health in addition to financial and economic support and has been identified as playing a distal role that operates through poor regulation of emotions.11 Adolescents who have poor parental attachment and ineffective skills to regulate their emotions may be at higher risk of negative self-criticism and low self-esteem; when they experience distress, they self-harm as a form self-punishment. Peterson et al., 200812 suggest that NSSI may appear as an affective strategy that generates harm when being overwhelmed by negative feelings. The coexistence of other disorders, such as borderline personality disorder (BPD) or the posttraumatic stress disorder (PTSD),13 is also a key factor. In fact, more than 70% of BPD patients report a history of multiple NSSI episodes, and 60% report multiple suicide attempts,14 but NSSI is not exclusive to patients with mental health disorders.
There is not a standardized method to deal with NSSI in adolescents, and very few studies have assessed the effectiveness of interventions that are specially designed to reduce them. The lack of research on the topic may be due to several reasons. First, NSSI is often combined with other terms, such as BDP, as if NSSI would be an exclusive domain of BDP, and therefore, therapies are frequently designed for BDP patients who self-injure. Second, the terminology used to refer to NSSI in the clinical literature is confusing and inextricable, with a wide range of related terms that are not always used synonymous used, such as parasuicide, mutilation, intentional injury, nonsuicidal injury, self-harm, or deliberate self-injury. Furthermore, the line that distinguishes these terms is not always clear in clinical practice, and many works refer to the broader term self-harm, such as the recent systematic review conducted by Witt and collaborators.15 This makes it difficult both to conduct a search for information on the topic and to compare studies; thus, a standardization of the technical language was necessary to better visualize the studies linked to the area, especially in a clinical intervention.9 The study's aim is to provide specific information related to NSSI and the treatments proposed to reduce them in adolescent population with maladaptive behavior without specific mental disorders (or that have not yet developed). To do so, we conducted this review and meta-analysis that assesses the efficacy of interventions for NSSI in this population.
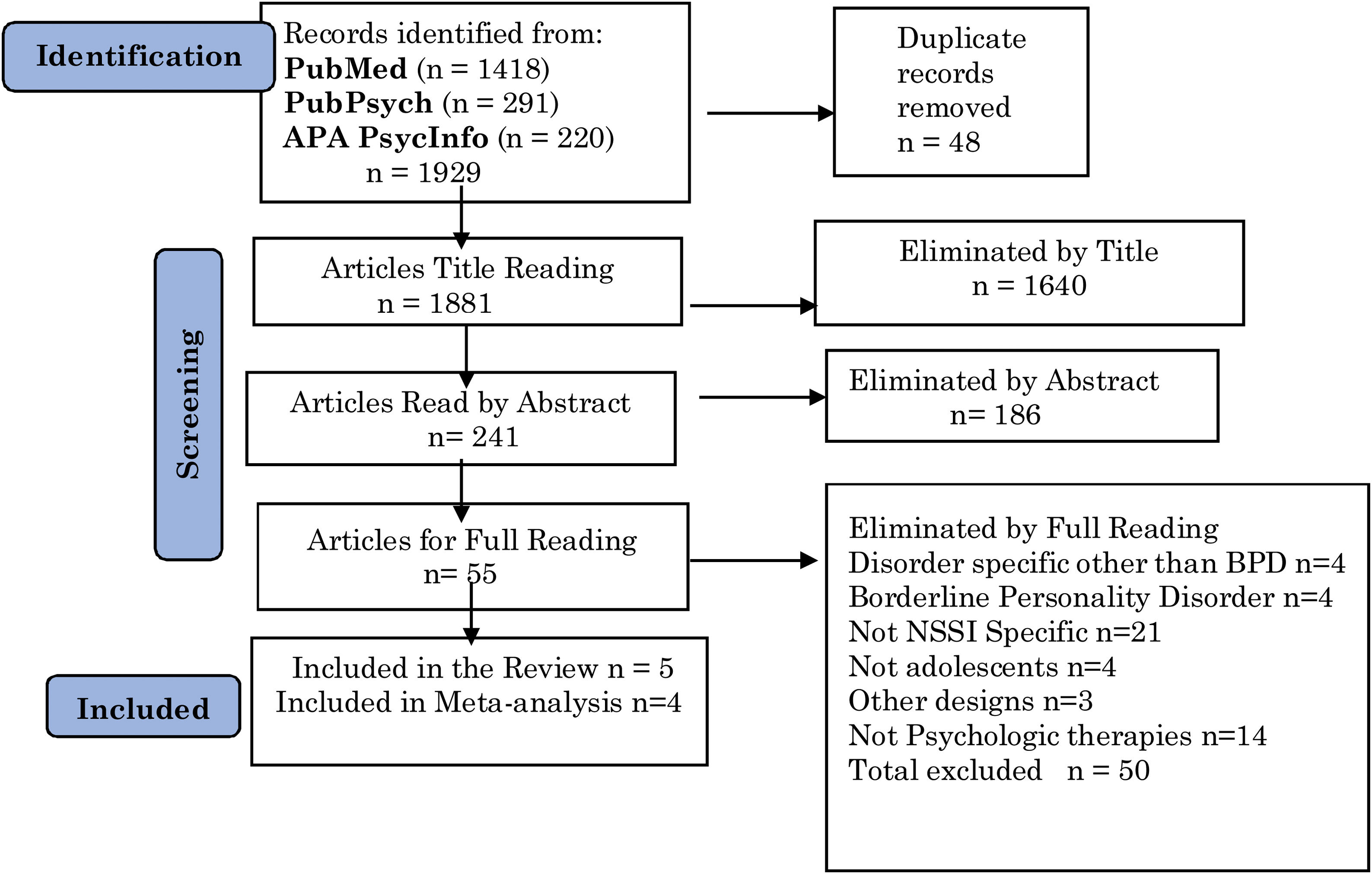
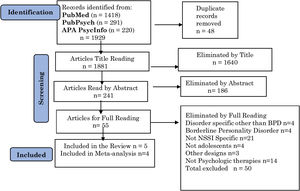
MethodsSearch strategy, information sources and eligibility criteriaThis review and meta-analyses were conducted following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines.16 The protocol of the study was registered in Prospero (ID: 252355). To identify studies eligible for inclusion in the review, a search was performed on March 22, 2021, using three databases: Medline, PsycINFO and PubPsych.
The search strategy was based on the PICOS-style approach. The terms included referring to the population analyzed were the MeSH term ‘Adolescent’ or a variant of it in free text. The terms included to refer to the outcome or objective were the MeSH term ‘self-injurious behavior’ or a variant of it in free text such as ‘nonsuicidal’, ‘self’ and ‘injury’. The filters used to refer to the study design were ‘clinical trial’ or ‘randomized controlled trial’. All three terms were joined with AND, and alternatives to the MeSH terms with ORs. No limit was applied to the search strategy regarding language or date. In addition, known reviews and lists of references of selected articles were tracked to find other records.
Studies were eligible for inclusion in the review regardless of the year of dissemination, language, or report status. Studies were not eligible if (A) they were not specific to NSSI; (B) they were conducted in a specific subpopulation with any psychological disorder other than borderline personality disorder (BPD), such as depression or bipolar disorder; (C) they were conducted in patients with BPD; (D) they were not specifically conducted in adolescents; (E) they did not assess interventions with a pre-post design or a randomized clinical trial design; or (F) they did not assess psychological therapies. Hence, interventions that assessed Deliberate Self Harm (DSH) were not included.
Data extraction, analysis, and reportingThe screening was performed in three phases: first, duplicate items were removed, and titles were analyzed; second, abstracts of the selected titles were considered; and finally, full texts of the selected abstracts were read. A unified chart of exclusion criteria was applied in the title, abstract and full-text screening steps. Each record was screened by one reviewer during the first two phases, whereas for the last stage, items were divided into two sets, and each set was reviewed independently by two reviewers; AG/VP reviewed the first set and BI/AdG reviewed the second set. Disagreements between screeners were discussed and resolved by consensus.
The information collected for the selected articles included type of design, publication year, country, number of participants, year range, a brief description of the intervention and its duration, outcomes measured and instruments of measurements for the outcomes.
Risk of bias assessmentThe tools used to assess the risk of bias in the included studies were the “Quality Assessment Tool for Before-After (Pre-Post) Studies With No Control Group” of the National Health Institute of United States (NHI)17 for studies with this design and the “Quality Assessment Tool of Controlled Intervention Studies” of the NIH for studies with Random Clinical Trial (RCT) design.17 The tool for the pre-post design studies consists of 12 questions that assess the quality of the research with three possible answers: yes/no/other (CD: cannot determine; NA: not applicable; NR: not reported). The first five questions refer to the study question and the study sample, the next four refer to the intervention process and outcomes and the last three refer to the analyses of data. Similarly, the tool for the RCT design studies consists of 14 questions with the same possible answers as the previous tool. The first five refer to the procedure of assignment, the next five refer to comparability between groups and the last four refer to the analyses conducted. Finally, the overall quality of each study was established by rating it as good, fair, or poor.
Effect measures, synthesis methods and reporting bias assessmentFor a study to be included in the synthesis, a measure of the change in NSSI after the intervention had to be included, the risk of bias assessment had to qualify it as fair or good, and a minimum of 10 participants had to be included to exclude pilot studies. The effect measure used was the standardized mean difference (SMD), that is, the post – pre-intervention mean difference divided by the estimate of the standard deviation for the pre-intervention data.18 The results of the studies included with an RCT design were summarized with the SMD for each arm. The outcomes assessed were changes in NSSI, global functioning (GF) and depressive symptomatology (DS). For those studies that did not present mean and standard deviation (SD) values but presented medians and interquartile ranges, an estimation of mean and SD values was conducted.19 Given that no study provided the intraindividual correlation between pre-post measures, r=0.5 was assumed. The method selected to conduct the meta-analysis was the random-effect meta-analysis with the DerSimonian-Laird estimator to estimate the amount of heterogeneity. To graphically represent the results, a forest plot for each of the outcome variables was displayed. Estimates of the amount of total heterogeneity were obtained using the Tau2 index and the I2 index. The possible presence of reporting bias was assessed using the funnel plot for each outcome, and their asymmetry with Egger's regression test.20 Finally, the trim and fill algorithm21 was used to estimate the effect of missing studies on the global estimate. The metafor package of the statistical program R version 3.6.322 was used to conduct the analyses.
Certainty assessmentThe overall quality of evidence for the three outcomes was appraised using the GRADE approach.23 The initial rating was ‘low’ quality due to the pre–post intervention nature of the items included. The risk of bias was assessed as described previously in the ‘risk of bias assessment’ paragraph. Indirectness of evidence was considered if the studies used a proxy measured to ascertain each outcome or deviated from the protocol. For inconsistency, we downgraded visualizing the forest plot and when I2 indicated substantial levels of heterogeneity (>50%). For imprecision, we downgraded if the 95% CI for the pooled effect included the null value. For the potential publication bias domain, we considered any evidence of funnel plot asymmetry. For the magnitude of the effect, we upgraded if SMD >0.8.
ResultsThe study selection process is described in Fig. 1. Combining the three databases (Medline, PubPsych and APA PsycINFO), a total of 1929 records were identified, and after removing 48 records that were duplicated, 1881 were screened based on their titles. After excluding 1640 in the title phase, 241 were screened during the abstract review, and after excluding 186 in this phase, 55 full texts were assessed for eligibility. Five studies were finally included in the review, and four were included in the meta-analysis.
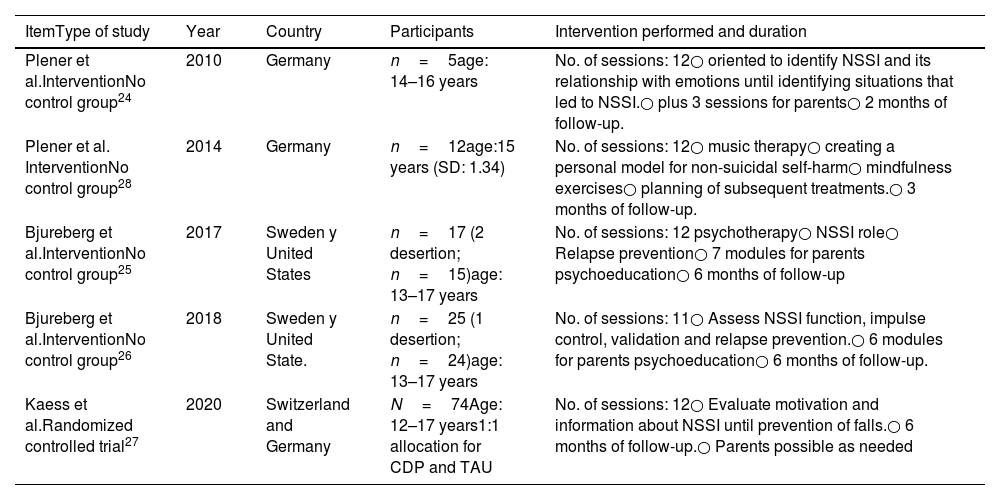
The main characteristics of the articles included in the study are presented in Table 1. Four studies were intervention studies without a control group, and the other was a randomized clinical trial. The dates range from 2009 to 2020, all were conducted in Europe, and in two cases, in cooperation with the United States. The age of the participants was between 12 and 17 years. The intervention analyzed in four of the studies consisted of 12 sessions, whereas the other study included 11 sessions. The post-intervention follow-up ranged from 2 to 6 months, the latter being the most frequent (n=3). Three of the studies incorporated sessions for parents. Different NSSI assessment instruments were used: Plener et al. (2010)24 incorporated the Self-Harm Behavior Questionnaire (SHBQ), Bjureberg et al. (2017)25 and Bjureberg et al. (2018)26 used the Deliberate Self-Harm Inventory (DSHI-9), and Kaess et al. (2020)27 used the German version of the Self-Injurious Thoughts and Behaviors Interview (SITBI-G). Additionally, Plener et al. (2014)28 used a qualitative measure through diary cards. All scales explore the activity, frequency and presence during recent months (maximum 12 months) of NSSI behavior, and all have been validated in adolescents. The DSHI-9 is specific to self-harm, whereas the SITBI-G and SHBQ explicitly incorporate suicidal behaviors. Details of the scales and their proprieties are given in Table S1 of the Supplementary Material. All studies had the pre–post intervention reduction in the NSSI values as the main outcome. Three of the studies also incorporated the Beck Depression Inventory II (BDI-II), with the pre–post intervention reduction in the BDI-II score being the associated secondary outcome, and three of them also incorporated functional assessment scales, two of them using the pre-post increase in The Children's Global Assessment Scale (CGAS) and one of them using the increase in the Kidscreen-27 score as a secondary outcome.
Characteristics of articles incorporated in systematic review and meta-analysis.
| ItemType of study | Year | Country | Participants | Intervention performed and duration |
|---|---|---|---|---|
| Plener et al.InterventionNo control group24 | 2010 | Germany | n=5age: 14–16 years | No. of sessions: 12○ oriented to identify NSSI and its relationship with emotions until identifying situations that led to NSSI.○ plus 3 sessions for parents○ 2 months of follow-up. |
| Plener et al. InterventionNo control group28 | 2014 | Germany | n=12age:15 years (SD: 1.34) | No. of sessions: 12○ music therapy○ creating a personal model for non-suicidal self-harm○ mindfulness exercises○ planning of subsequent treatments.○ 3 months of follow-up. |
| Bjureberg et al.InterventionNo control group25 | 2017 | Sweden y United States | n=17 (2 desertion; n=15)age: 13–17 years | No. of sessions: 12 psychotherapy○ NSSI role○ Relapse prevention○ 7 modules for parents psychoeducation○ 6 months of follow-up |
| Bjureberg et al.InterventionNo control group26 | 2018 | Sweden y United State. | n=25 (1 desertion; n=24)age: 13–17 years | No. of sessions: 11○ Assess NSSI function, impulse control, validation and relapse prevention.○ 6 modules for parents psychoeducation○ 6 months of follow-up. |
| Kaess et al.Randomized controlled trial27 | 2020 | Switzerland and Germany | N=74Age: 12–17 years1:1 allocation for CDP and TAU | No. of sessions: 12○ Evaluate motivation and information about NSSI until prevention of falls.○ 6 months of follow-up.○ Parents possible as needed |
| Item | Scales | Outcome |
|---|---|---|
| Plener et al., 201024 | FASMSHBQBDI-II | NSSI reduction.Reduction of depressive symptoms. |
| Plener et al., 201428 | Diary CardsBDI-II | NSSI reduction.Reduction of depressive symptoms. |
| Bjureberg et al., 201725 | DSHI-9CGAS | NSSI reduction.Global functionality increase. |
| Bjureberg et al., 201826 | DSHI-9CGAS | NSSI reduction.Global functionality increase. |
| Kaess et al., 202027 | SITBI-GBDI-IIKidscreen-27 | NSSI reduction.Reduction of depressive symptoms.Global functionality increase. |
FASM: Functional Assessment of Self-Mutilation; SHBQ: Self-Harm Behavior Questionnaire; BDI-II: Becks Depression Inventory, second edition; DSHI-9: Deliberate Self Harm Inventory; CGAS: The Children's Global Assessment Scale; SITBI-G German version of the Self-Injurious Thoughts and Behaviors Interview.
The results of the risk of bias assessment are presented in Table S2 of the Supplementary Material, and include the answers given to the different questions of each of the tools used. All studies properly described the objective of the study (P1), the selection criteria (P2), the patients who were included (P4), the intervention to be performed (P6), and the rate of dropouts in the process (P9), and all used scores measured more than once to assess the results (P11). Two studies obtained negative evaluations in the description and validity of the measurement instruments used (P7), and in relation to the representativeness of the sample (P3). One study did not present statistical tests or precision measures of the estimates (P10). All studies had smaller sample sizes than required (P5), and none of them appropriately reported the blinding procedure of assessors (P8). The work with clinical trial design obtained favorable results in the 14 questions of the tool used. In the global evaluation, Plener et al. (2010)24 was rated as poor quality, Plener et al. (2014)28 as fair quality and the rest as good quality.
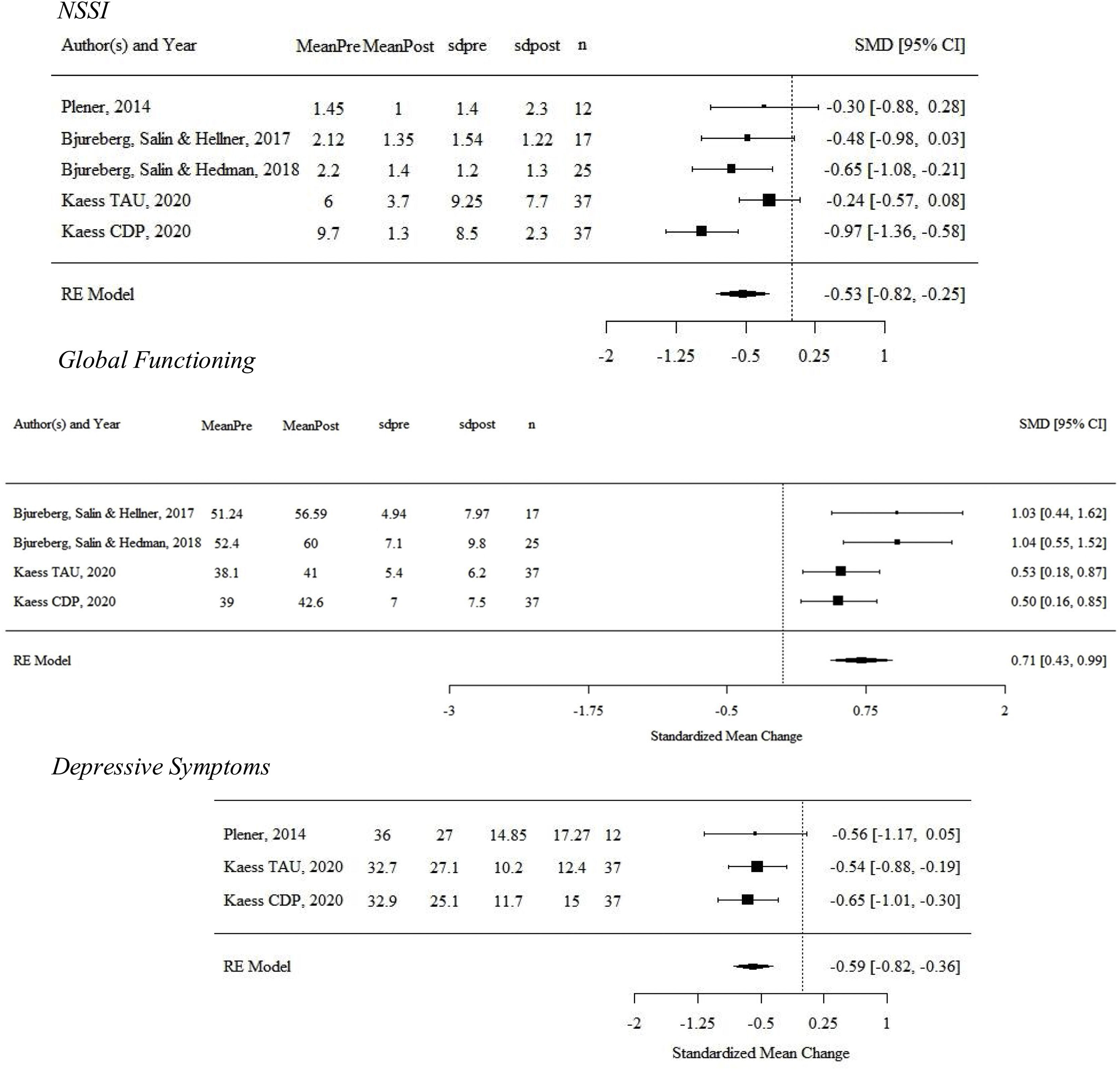
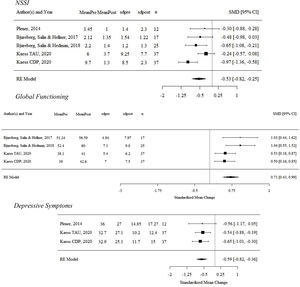
Fig. 2 shows the forest plots with the effect sizes of the intervention for each study and the summary effect for the three outcome variables studied, number of NSSI episodes, Global Functioning and Depressive Symptoms, and Table S3 in the Supplementary Material gives the numerical data and the test comparisons within the study. The study by Plener et al. (2010)24 was not included in the quantitative analysis of the results because it obtained a result of poor quality in the global evaluation. In Kaess et al. (2020)27 two interventions were differentiated, Treatment as Usual (TAU) and Cutting Down Program (CDP), so five interventions were included in the quantitative analysis for the NSSI variable, four for global functioning and three for depressive symptoms.
For the main outcome, change in NSSI, Kaess et al.27 in the CDP arm and Bjureberg et al.26 showed a reduction in SMD of −0.97 (95% CI: −1.36, −0.58) and −0.65 (95% CI: −1.08, −0.21) respectively, while the other three therapies provided lower reductions. The summary effect of the five interventions analyzed showed a reduction in the number of NSSI of SMD=−0.53 (95% CI: −0.82, −0.25). In the global functioning variable, all studies showed a significant increase, with effect sizes from 0.50 to 1.03, with the summary estimate of SMD=0.71 (95% CI: 0.42, 0.99). Finally, for depressive symptoms, Kaess TAU and Kaess CDP27 showed a reduction of −0.54 (95% CI: −0.88, −0.19) and −0.65 (95% CI: −1.01, −0.30) respectively, while in Plener et al. (2014),28 a reduction of −0.56 (95% CI: −1.17, 0.05) was observed. The summary effect of the three included studies showed a reduction of SMD=−0.59 (95% CI: −0.82, −0.36).
The degree of heterogeneity of the observed estimates was moderate for NSSI (I2=54.1%) and for global functioning (I2=42.5%) and low for depressive symptoms (I2=0%), whereas Cochran's Q test was not significant in the three cases (p value equal to 0.069, 0.156 and 0.897, respectively). Figure S2 in the Supplementary Material shows the funnel plot for each of the three variables studied that summarized the results of the publication bias assessment. No asymmetries are observed for the number of NSSI episodes or depressive symptoms, but a slight asymmetry is observed for global functioning results. In the same direction, Egger's test showed p values of 0.915, 0.051 and 0.911 for the number of NSSI, global functioning and depressive symptoms, respectively. This suggested the need to use the trim and fill method for global functioning to provide an estimate of the unbiased effect, which provided an estimated effect of 0.62 (95% CI: 0.34, 0.91).
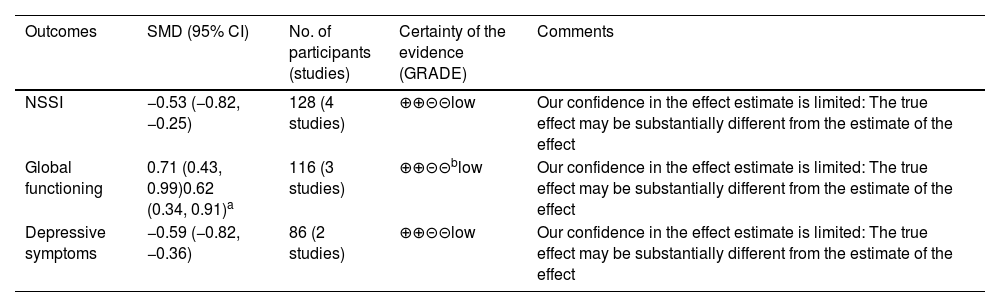
Finally, the results of the certainty assessment following the GRADE methodology are given in Table 2. The starting point for all outcomes has been a ‘low’ grade of evidence due to the nonrandomization nature of the design of the studies (although Kaess et al.27 is a randomized clinical trial, here, the pre-post results of each intervention have been used due to the aim of our study). We have not downgraded them in any of the outcomes because we have considered that (a) the risk of bias is not high for any outcome, (b) there is no indirectness in the measurements, (c) I2 is not substantial, although for NSSI it is at the limit, (d) the 95% CI for the pooled effects does not include the null value, and (e) there are no important asymmetries in the funnel plots. We have not upgraded them because (a) the magnitude of the effects is not greater than 0.8 in any case, (b) there is no evidence of a dose-response gradient, and (c) there is no result showing the effect of confounders.
Summary of findings using GRADE methodology.
| Outcomes | SMD (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments |
|---|---|---|---|---|
| NSSI | −0.53 (−0.82, −0.25) | 128 (4 studies) | ⊕⊕⊝⊝low | Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect |
| Global functioning | 0.71 (0.43, 0.99)0.62 (0.34, 0.91)a | 116 (3 studies) | ⊕⊕⊝⊝blow | Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect |
| Depressive symptoms | −0.59 (−0.82, −0.36) | 86 (2 studies) | ⊕⊕⊝⊝low | Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect |
This systematic review and meta-analysis demonstrate the scarcity of works assessing interventions focused on reducing NSSI, configuring itself as an emerging theme, and shows that interventions specifically designed for NSSI are effective in reducing both the number of NSSI episodes and depressive symptoms as well as in improving global functioning. However, the degree of certainty of the findings is low, mainly due to the nature of the design of the studies, the limited number of studies and the small sample size.
The fact that some works mix NSSI with other disorders is a cause of concern and complicates the literature search and the assessment of effectiveness of therapies. Additionally, the fact that many studies29–31 assess interventions only in participants with different underlying pathologies does not allow us to know if interventions are effective in people with NSSI, regardless of the coexistence of other disorders. We focused this review on adolescents who had engaged in NSSI with no specific associated mental disorder because we identified a lack of research on these individuals that, otherwise, receive no other treatment. We think that the recent inclusion of the specific ICD-10-CM codes for NSSI and for suicidal behavior in the DSM-5-TR will facilitate research on the topic. Furthermore, we consider that there is a need to specifically study NSSI separated from suicidal behavior since the aim of nonsuicidal self-harm is not configured with an express desire to die, and hence, the function of NSSI may differ from that of suicidal attempts. A meta-analysis of the prevalence of different functions of NSSI32 identified that intrapersonal functions (66%–81%), and especially those concerning emotion regulation (63%–78%), were the most commonly reported functions by individuals who engage in NSSI, whereas interpersonal functions (for instance, expressing distress) were less common (33%–56%). These results can guide the design of therapies, as different functions potentially entail different clinical needs in terms of therapeutic support and different training demands for services.
Our systematic review found only five studies that assessed the effectiveness of therapies designed to reduce NSSI in adolescents. The meta-analysis results suggested consistency among the therapies’ effectiveness, showing no high heterogeneity among them. The therapies that showed clear effectiveness were those presented in Kaess et al. (2020),27 Bjureberg et al. (2018)25 and Bjureberg et al. (2019),26 whereas that presented in Plener et al. (2014)28 had modest effects. The basis of this last proposed therapy is the use of music, under the assumption that it can lead to the development of an individual's ability to perceive and relate. This lower effect could be because the therapy was provided at the group level and the low number of patients. Therapies presented in Kaess et al. (2020),27 Bjureberg et al. (2018)25 and Bjureberg et al. (2019)26 have similar (though not identical) theoretical bases, but the actions to be conducted within sessions differ in certain aspects. The Cutting Down Program (CDP) used in Kaess et al. (2020)27 is based on Cognitive Behavioral Therapy (CBT) and Dialectical Behavioral Therapy (DBT), whereas the ERITA Program used in Bjureberg et al. (2018)25 and Bjureberg et al. (2019)26 (an adaptation of Bjureberg et al.25 to be delivered online) is a behavioral therapy based on acceptance and commitment. The CDP27 was designed exclusively for nonsuicidal self-injury to reduce maladaptive behaviors,33 and was based on the Manually Assisted Cognitive Behavioral Therapy (MACT),34 which was adapted for NSSI and specifically for adolescents. The CDP also has similarities with the Mental Health First Aid Training and Research Program of Australia,35 which can be considered one of the few specific manuals for self-injury that provides clinical guidance on how to help someone who has engaged in NSSI. The ERITA program, in contrast, was developed to treat self harm by targeting its underlying mechanism of emotion dysregulation, teaching skills aimed at improving emotion regulation, and was adapted from the Emotion Regulation Group Therapy manual (ERGT), which had been used in trials designed to treat adult women with self-harm and borderline personality disorder (BPD).36,37
The duration and dynamics of treatments between these therapies are also similar, but present some differences. The CDP (Kaess et al., 2020)27 can have between eight to twelve sessions, and the ERITA used in Bjureberg et al. (2018) and Bjureberg et al. (2019)25,26 had eleven to twelve sessions, after joining some of the fourteen of the ERGT program. Regarding the actions to be conducted, CDP (Kaess et al., 2020)27 focuses on the functionality of the subject by delivering skills, whereas ERITA focuses on knowing the function of self-injury through the emotional acceptance. More precisely, the CDP consists of four modules, one devoted to identifying the reasons for the behavior of NSSI, the second to identifying and understanding their feelings, the third to finding alternative solutions to self-injury, and the last to preventing relapses. The ERITA consists of different modules for adolescents, including functionality, emotional and relapse prevention, and others for parents, including psychoeducation and validation.
Both the CDP program27 and the intervention presented in Bjureberg et al.26 incorporate parents into the psychotherapy, although in the CDP program, their participation is left as a decision by each therapist. To analyze this aspect from the basic theoretical perspective proposed by DBT, we highlight the importance of accounting for the invalidating environment, which is the intolerance of the emotionality of important people in the individual's environment.36 Hence, we consider that the incorporation of parents into the therapy allows them to participate in the task of emotional regulation, favoring optimal results. In the same direction, the intervention proposed by Bjureberg et al.26 was focused on increasing the emotional approach throughout the treatment, with an emphasis on increasing emotional awareness and validation, where the incorporation of the family is important. The results of their clinical trial study support the involvement of the family because improvements in the parental punitive responses to the negative emotions of their children and on the encouragement to their children's emotional expressions were observed.
Among the strengths of this review, we highlight that this is the first conducted to assess therapies specifically designed for adolescents who have engaged in nonsuicidal self-injuries, a disorder recently included in the DSM 5th edition text revision. This study provides an exhaustive analysis of the studies included using a standardized methodology that assesses the quality of the items as well as the certainty of the evidence provided. One of the limitations of this study is that the search was conducted using the English language, so there may be some studies that use other languages that have not been included in the review. Another is that the meta-analysis includes results on three outcomes, namely NSSI reduction, depressive symptoms reduction and global functioning, but other outcomes such as comorbid disorders associated with the NSSI, assessed elsewhere,38 have not been included due to the scarcity of studies that include them. The third is that most studies included in the review had a pre-post design and not a clinical trial design, so caution is needed in interpreting the results since the assumption of comparability across moments in a person's life may not hold in this context. Another limitation is that it excluded studies with interventions specifically designed for patients with BPD or other psychiatric diagnosis, such as depression or bipolar disorder, which may limit generalizability. Finally, it should be mentioned that the scarcity of works on the topic, together with the small sample size and other methodological problems of the items included, do not allow for a clear conclusion on the effectiveness of the treatments, making it impossible to conduct subanalyses by therapy type.
This area of research is of growing interest, especially after the COVID-19 disruption in 2019, when the mental health of the general population has been seriously affected, in adolescents in particular. New studies with adequate designs to assess and compare the effectiveness of different therapy modalities need to be conducted to overcome the methodological shortcomings found in this review. The inclusion of studies of new modalities of therapy adapted to the new post-COVID19 reality, such as the online approach, is compulsory. This will be the case of the randomized clinical trial STAR (DRKS00014623), a large-scale multicenter study including adolescents who engage in NSSI, that will assess the effect on NSSI reduction of an online therapy based on that used in Kaess et al.27.
In conclusion, cognitive-behavioral and emotional regulation therapies designed specifically to reduce NSSI are effective not only in reducing its frequency but also in reducing associated depressive symptoms and in increasing global functionality. It appears that the incorporation of parents or caregivers to take part in therapy is effective, which reinforces the idea that relational elements are configured as a protective environment against NSSI.
FundingThis study did not receive specific funding from public sector agencies, the commercial sector, or non-profit bodies.
Conflict of interestsThe authors declare that they have no conflict of interest.