Abuse/dependence and acute use of ethanol and illicit drug are considered risk factors for suicide. The risk is also influenced by demographic conditions and/or psychiatric comorbidity. The aim of the study was to test the association between presence of ethanol, illicit substances and prescribed drugs in suicide decedents and controls.
Materials and methodsCase–control study of autopsies performed in the Biscay Forensic Pathology Service, Basque Country, Spain from 01/01/2010 to 30/06/2021 in subjects between 15 and 55 years old. Suicide deaths (n=481) with completed autopsy were evaluated. Concurrent natural deaths were chosen as controls (n=330). The risk for suicide according to demographic, toxicological and psychiatric variables was analyzed using logistic regression.
ResultsEthanol was present in 21% and illicit drugs, mainly cannabis, cocaine and amphetamine, in 27% of suicide deaths. Illicit drugs were more frequent among males. In 63% of suicide cases, prescribed psychotropic drugs were detected.
In a multivariate analysis, the main risk factors for suicide were psychiatric diagnosis of illicit drug abuse/dependence (OR=5.56, 95% CI 2.74–11.30) or another mental disease as mood or psychotic disorders (OR=13.05, 95% CI 8.79–19.37). Acute presence of ethanol (OR=4.22, 95% CI 2.52–7.08), recent use of cocaine (OR=2.52, 95% CI 1.05–6.07) and age <35 years (OR=2.50, 95% CI 1.62–3.87) were also associated with suicide deaths.
ConclusionsThe presence of drugs of abuse in suicide deaths of people ≤55 years old is high. Recent use of ethanol and cocaine is significantly associated with an increased suicide risk. Specific prevention strategies against exposition to substances of abuse should be promoted, especially in psychiatric patients.
Suicide is an important public health issue being one of the main causes of unnatural death worldwide. At European Union, the suicide rate stood on average at 11 deaths per 100,000 inhabitants in 2015.1 In the Basque Country, the rate was close to eight deaths per 100,000.2 Suicide possesses multiple associated risk factors, including acute and chronic use of illicit drugs and ethanol.3–6
Substance abuse has a high prevalence in Europe.7 In the Basque Country, whereas the prevalence of ethanol use is at the European average, cannabis and amphetamines use has higher prevalence rates. Conversely, cocaine use, although important, has significantly lower rates than in other countries as the United Kingdom or other regions of Spain.7–11 In this context, investigations about use of illicit drugs and completed suicide are scarce. Some studies have analyzed the association between drug abuse/dependence and suicide.3,5,12,13 However, the relationship between acute use of these substances in the hours preceding death and the suicide behaviour has received less scientific attention.15–18 Therefore, suicide population studies based on forensic autopsies with systematic toxicological analysis could be of interest to improve the current knowledge about this putative association. Moreover, as drug use and abuse are modifiable risk factors, these studies could help to promote better strategies in suicide prevention.
Taking into consideration the previous points, a forensic case–control study of suicide deaths was carried out in a well-defined population of young people and middle-aged adults. The study (i) examined the presence of substances of abuse (legal and illicit) in postmortem samples as indicative of use in the hours before suicide; (ii) determined the frequency of alcohol and drug abuse disorders in this population of suicide decedents and controls; and (iii) assessed if recent use as well as drug abuse/dependence were associated with an increased risk of death by suicide. Since self-poisoning methods could influence the results, suicide deaths were initially separated into poisoning and non-poisoning groups.
Materials and methodsData sourceThe study was performed in Biscay, an industrial province of the Basque Country (North Spain) with a total population around 1,150,000 inhabitants.
According to Spanish legislation, a forensic autopsy is required when there is suspicion of suicide death. In all autopsies, a toxicological analysis is requested except if the person was admitted to a hospital and stayed for more than 48h after the suicide attempt. Forensic autopsy reports are coded according to the underlying cause of death following the International Classification of Diseases (ICD-10).
Selection of subjectsBiscay Forensic Pathology Service is the only institution in charge of the medico-legal investigation of completed suicide in this province. Files of this Service were carefully reviewed. All suicide deaths in subjects ≤55 years old recorded from 1 January 2010 to 30 June 2021 and that incorporated a toxicological analysis were included in the study. People over 55 years of age were excluded because, based on population surveys, the consumption of illegal drugs in them is practically non-existent.8
The control group consisted of forensic cases of natural sudden deaths in subjects 15–55 years old in which toxicological analysis was carried out. Deaths due to heart disease or brain haemorrhage were excluded since illicit drug use in them is a known risk factor.19–22
Autopsy procedureA complete autopsy with histopathological study was performed. Clinical data and circumstances surrounding the death were also reviewed. This information was obtained from physicians’ and forensic doctors’ reports, official police statements and interviews with the family. The cause of death was established considering together clinical history, autopsy findings and the results of all ancillary examinations.
Femoral blood (alternatively, cardiac blood), vitreous fluid and urine samples were collected for toxicological analyses. In decomposing bodies, alternative samples were liver, kidney or bile. Analyses were performed at the Basque Institute of Legal Medicine in Bilbao, and at the National Institute of Toxicology and Forensic Sciences in Madrid, Spain. Enzyme immunoassay, high-performance liquid chromatography and gas chromatography/mass-spectrometry were used for the detection of therapeutic drugs, illicit drugs and ethanol.
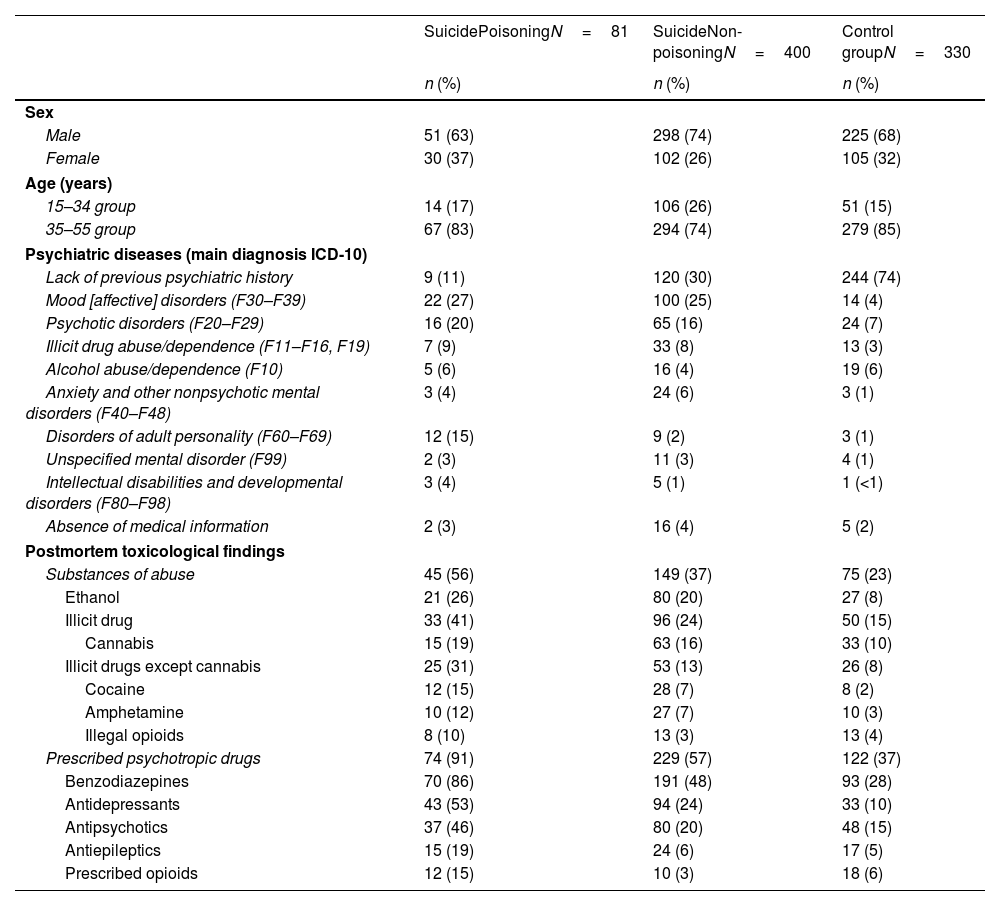
VariablesDemographic data, psychiatric diagnosis according to ICD-10 and toxicological information were evaluated in suicide and control groups. Suicide deaths were separated into poisoning and non-poisoning (violent) methods (Table 1).
Demographic characteristics, psychiatric diagnoses and postmortem toxicological data in suicide cases and control group.
| SuicidePoisoningN=81 | SuicideNon-poisoningN=400 | Control groupN=330 | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Sex | |||
| Male | 51 (63) | 298 (74) | 225 (68) |
| Female | 30 (37) | 102 (26) | 105 (32) |
| Age (years) | |||
| 15–34 group | 14 (17) | 106 (26) | 51 (15) |
| 35–55 group | 67 (83) | 294 (74) | 279 (85) |
| Psychiatric diseases (main diagnosis ICD-10) | |||
| Lack of previous psychiatric history | 9 (11) | 120 (30) | 244 (74) |
| Mood [affective] disorders (F30–F39) | 22 (27) | 100 (25) | 14 (4) |
| Psychotic disorders (F20–F29) | 16 (20) | 65 (16) | 24 (7) |
| Illicit drug abuse/dependence (F11–F16, F19) | 7 (9) | 33 (8) | 13 (3) |
| Alcohol abuse/dependence (F10) | 5 (6) | 16 (4) | 19 (6) |
| Anxiety and other nonpsychotic mental disorders (F40–F48) | 3 (4) | 24 (6) | 3 (1) |
| Disorders of adult personality (F60–F69) | 12 (15) | 9 (2) | 3 (1) |
| Unspecified mental disorder (F99) | 2 (3) | 11 (3) | 4 (1) |
| Intellectual disabilities and developmental disorders (F80–F98) | 3 (4) | 5 (1) | 1 (<1) |
| Absence of medical information | 2 (3) | 16 (4) | 5 (2) |
| Postmortem toxicological findings | |||
| Substances of abuse | 45 (56) | 149 (37) | 75 (23) |
| Ethanol | 21 (26) | 80 (20) | 27 (8) |
| Illicit drug | 33 (41) | 96 (24) | 50 (15) |
| Cannabis | 15 (19) | 63 (16) | 33 (10) |
| Illicit drugs except cannabis | 25 (31) | 53 (13) | 26 (8) |
| Cocaine | 12 (15) | 28 (7) | 8 (2) |
| Amphetamine | 10 (12) | 27 (7) | 10 (3) |
| Illegal opioids | 8 (10) | 13 (3) | 13 (4) |
| Prescribed psychotropic drugs | 74 (91) | 229 (57) | 122 (37) |
| Benzodiazepines | 70 (86) | 191 (48) | 93 (28) |
| Antidepressants | 43 (53) | 94 (24) | 33 (10) |
| Antipsychotics | 37 (46) | 80 (20) | 48 (15) |
| Antiepileptics | 15 (19) | 24 (6) | 17 (5) |
| Prescribed opioids | 12 (15) | 10 (3) | 18 (6) |
Values are frequency (percentage) for categorical variables. χ2 test was used for the comparison between groups.
Two age groups were defined: 15–34 years old, considered as young adults, and 35–55 years old, assumed as middle age adults. This separation is usually established in survey studies on drug use and abuse, due to the important consume differences between ages.7,8
Toxicological positive results, showing recent use of the substance, were coded in three groups: (i) ethanol (the legal limit for driving of 0.5g/L blood concentration was used as cut-off); (ii) illicit drugs including cannabis, cocaine, amphetamine, opioids (heroin and non-prescribed methadone) and others; and (iii) prescribed psychotropic drugs. Prescribed opioids included methadone when a medical prescription was present in the clinical report.
All the procedures were performed in compliance with Spanish policies of research and ethical boards for postmortem forensic studies. Institutional review board approval was obtained from the Basque Institute of Legal Medicine.
Data analysisThe distribution of data is presented as median and interquartile ranges [IQ25–75] or as a percentage. Differences between groups were compared using χ2 test.
A multiple logistic regression analysis was performed to identify the potential associations between presence of ethanol and illicit drug in toxicological analysis and diagnosis of ethanol, illicit drug abuse/dependence or another psychiatric disorder with death by suicide. Adjusted odds ratios and 95% confidence intervals were calculated. Here, four mental disorders categories were established: (i) alcohol abuse/dependence; (ii) illicit drug abuse/dependence; (iii) other mental disorders; and (iv) lack of previous psychiatric history. We fitted to a reduced model to explain suicide by a backward stepwise approach that sequentially removed variables that not attained a p≤0.10.
All statistical analyses were performed by using SPSS software (version 23.0). A p value <0.05 was regarded as statistically significant.
ResultsDuring the eleven and a half years covered, 1037 suicides were investigated in Biscay (mortality rate 7.93/100,000/year). A number of 504 subjects were between 15 and 55 years old. Mortality rate in them was 7.07 (10.11 for males and 4.02 for females; 4.28 for people <35 years old and 8.91 for people 35–55 years old). Toxicological information was available in 481 subjects (95%). Completed suicide due to poisoning was established in 81 cases (70 of them were poisoning by prescribed psychotropic drugs associated to ethanol and/or illegal drugs) whereas the remaining cases were violent non-poisoning suicides.
In the same period, 2378 natural deaths were investigated at the Biscay Forensic Pathology Service. The number of natural deaths in people 15–55 years old was 1038 and in 961 (93%) of them, a toxicological study was carried out. Three hundred thirty cases were sudden deaths not due to heart disease or brain haemorrhage and, therefore, included in the control group. Deaths were due to digestive diseases (n=104), lung diseases (n=49), unexplained natural deaths (n=41), pulmonary embolism (n=40), aortic pathology (n=37), endocrine and metabolic diseases (n=18), neurological diseases (n=18), systemic infections (n=9), and others (n=14). Their demographic data, psychiatric diagnosis and toxicological information are in Table 1.
Description of suicide cases with toxicological analysisDemographic data and psychiatric diagnosisIn suicide decedents, male was more frequent than female. Median age was 43 years (IQ25–75=34–49). The most frequent diagnoses were mood and psychotic disorders. Illicit and ethanol drug abuse/dependence had a frequency of 9% and 5%, respectively (Table 1).
The distribution of mental disorders in suicide cases was different between sex (p=0.001) and age (p=0.013) groups. Mood disorders stood out in women (48% vs 26% in men). In contrast, psychotic disorders and drug abuse/dependence were more frequent in men (22% vs 15% and 12% vs 5%, respectively). Lack of previous psychiatric history was more prevalent among young than in middle age suicide adults (46% vs 29%). On the contrary, mood disorders and alcohol abuse/dependence rates were higher in subjects aged 35–55 years (34% vs 22% and 6% vs 2%; respectively).
Postmortem toxicological dataToxicological analysis was positive in 377 suicide subjects (78%). Prescribed psychotropic drugs were detected in 63%, and substances of abuse (ethanol and/or illicit drugs) were present in 40% of suicide cases (Table 1): ethanol at a concentration >0.5g/L in 21% (concentration was ≥1g/L in 77% of them) and illicit drugs in 27%, being cannabis the most frequent (n=78). Illicit drugs except cannabis were detected in 78 cases. Ethanol, illicit substances and prescribed drugs were more frequent in poisoning than in non-poisoning suicide cases (Table 1).
Concurrent use of psychostimulant drugs with ethanol was detected. The presence of cocaine (16% vs 6%; p=0.004) and amphetamine (15% vs 6%; p=0.005) was higher in ethanol positive cases than in negative cases, whilst opioids and cannabis presence was similar between positive and negative ethanol cases.
The proportion of subjects who used illicit drugs (31% vs 16%; p=0.001), mainly cannabis (19% vs 9%; p=0.008) and cocaine (11% vs 2%; p=0.003), was higher among males. No significant differences were observed among age groups.
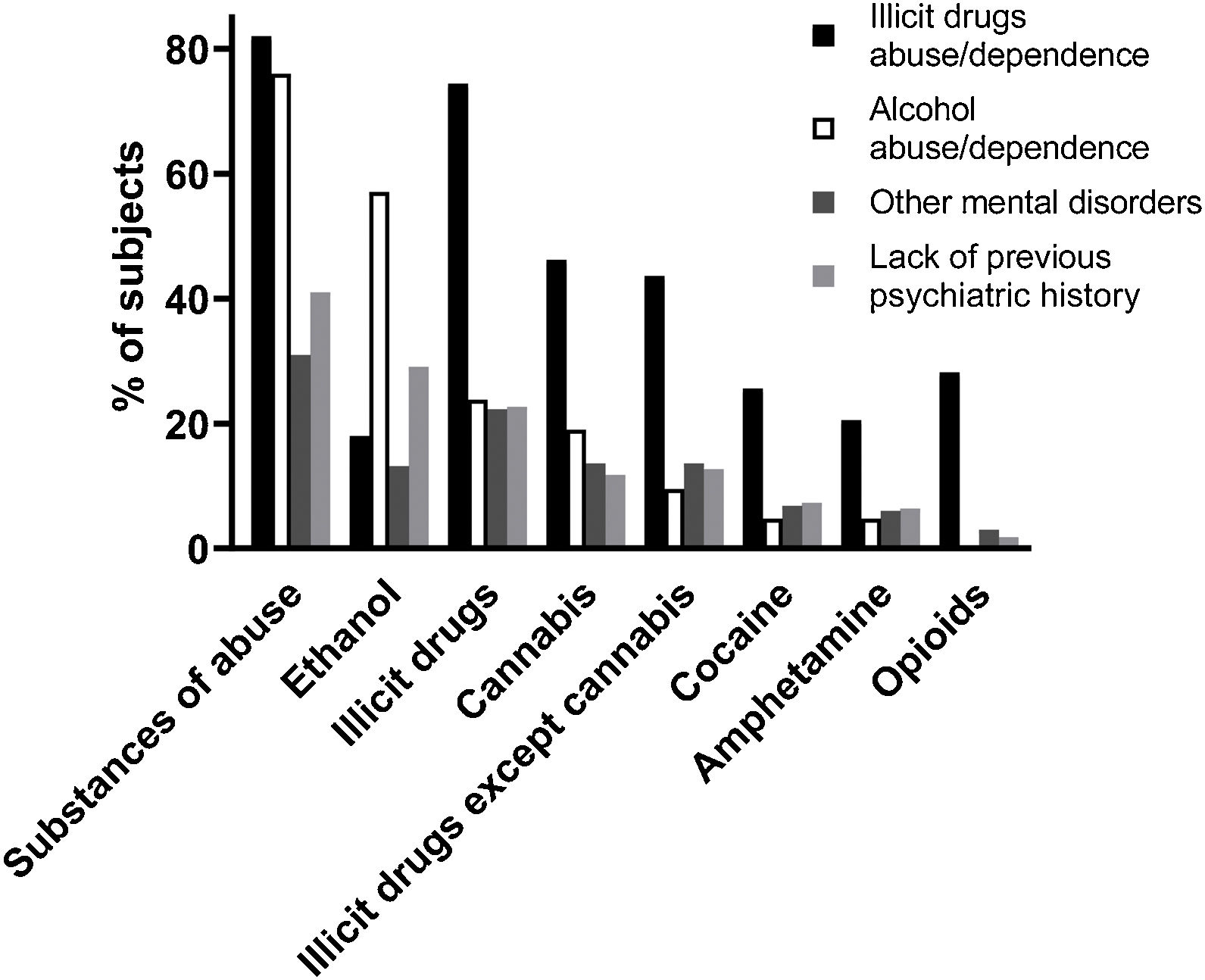
Relationship between psychiatric diagnosis and toxicological informationInformation about substances of abuse detection in suicide cases according to the psychiatric diagnosis is in Fig. 1. Important presence of ethanol was confirmed in subjects diagnosed with alcohol abuse/dependence; however, the relative high frequency in people without previous psychiatric history also stood out. Presence of illicit drugs was confirmed as higher in subjects diagnosed of illicit drug abuse/dependence (75%) than in the rest of the groups (frequencies between 18% for mood disorders and 26% for psychotic disorders).
Antidepressants were detected in 53% of suicide subjects with diagnosis of mood disorders and in 4% in the suicide group that lacked of previous psychiatric history. Antipsychotic drugs were presents in 73% of suicide cases with psychotic disorders and in 2% among subjects lacking of psychiatric records.
Comparison between suicide deaths and control groupMedian age of controls was 48 years (IQ25–75=40–52). The percentage of young people was higher in suicide than in control group. Violent suicide methods were more common in this age group. Psychiatric diagnoses were also different between suicides and controls. Thus, 74% of controls had not previous psychiatric history vs 27% in suicide cases. The frequencies of mood and psychotic disorders as well as illicit drug abuse/dependence were higher in the suicide than in the control group (Table 1). In consonance with this, postmortem toxicological results showed significantly higher figures for benzodiazepines, antidepressants and antipsychotics in suicide. With regard to the presence of substances of abuse, ethanol, cannabis and psychostimulant drugs detection was higher in suicides than in controls (Table 1).
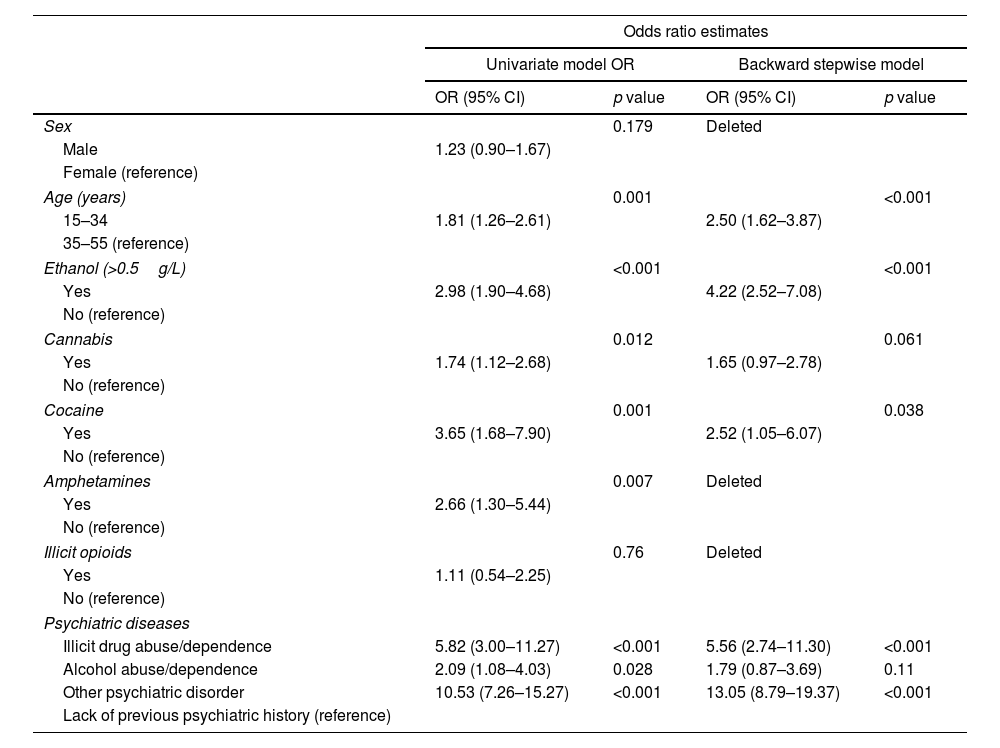
Due to the differences in sex, age, existence of psychiatric diagnoses and toxicological findings between suicide and control groups, a multiple logistic regression was performed. The analysis showed that for young adults, compared with middle age persons, the risk of suicide was 2.5 times higher (Table 2). Recent use of ethanol and cocaine were main risk factors associated with suicide after controlling for demographic characteristics and mental diagnoses. Thus, subjects that consumed ethanol in the previous hours to death presented a 4.2-fold greater risk for suicide than those who did not use ethanol. The recent use of cocaine was related to an increase of suicide risk up to 2.5-fold over the basal condition. Compared with subjects without a previous mental disorder, subjects diagnosed of illicit drug abuse/dependence showed more than 5-fold higher risk for suicide. However, to have a mental disorder different to substances abuse increased the risk of suicide up to 13 times.
Results of logistic regression models analyzing risk factors for suicide group compared with control group.
| Odds ratio estimates | ||||
|---|---|---|---|---|
| Univariate model OR | Backward stepwise model | |||
| OR (95% CI) | p value | OR (95% CI) | p value | |
| Sex | 0.179 | Deleted | ||
| Male | 1.23 (0.90–1.67) | |||
| Female (reference) | ||||
| Age (years) | 0.001 | <0.001 | ||
| 15–34 | 1.81 (1.26–2.61) | 2.50 (1.62–3.87) | ||
| 35–55 (reference) | ||||
| Ethanol (>0.5g/L) | <0.001 | <0.001 | ||
| Yes | 2.98 (1.90–4.68) | 4.22 (2.52–7.08) | ||
| No (reference) | ||||
| Cannabis | 0.012 | 0.061 | ||
| Yes | 1.74 (1.12–2.68) | 1.65 (0.97–2.78) | ||
| No (reference) | ||||
| Cocaine | 0.001 | 0.038 | ||
| Yes | 3.65 (1.68–7.90) | 2.52 (1.05–6.07) | ||
| No (reference) | ||||
| Amphetamines | 0.007 | Deleted | ||
| Yes | 2.66 (1.30–5.44) | |||
| No (reference) | ||||
| Illicit opioids | 0.76 | Deleted | ||
| Yes | 1.11 (0.54–2.25) | |||
| No (reference) | ||||
| Psychiatric diseases | ||||
| Illicit drug abuse/dependence | 5.82 (3.00–11.27) | <0.001 | 5.56 (2.74–11.30) | <0.001 |
| Alcohol abuse/dependence | 2.09 (1.08–4.03) | 0.028 | 1.79 (0.87–3.69) | 0.11 |
| Other psychiatric disorder | 10.53 (7.26–15.27) | <0.001 | 13.05 (8.79–19.37) | <0.001 |
| Lack of previous psychiatric history (reference) | ||||
OR: odds ratio; CI: confidence interval.
Ethanol and/or illicit drugs use disorders as well as acute intoxication are associated with a substantial increase in suicide risk.3,5,6,13–18,23,24 The rate of illicit drugs and ethanol presence in suicide is variable among the different autopsy studies examining the issue. Estimations are influenced by the different frequency of use in the general population and other covariates such as psychiatric comorbidity and the necessary distinction between acute (toxicological) presence and (clinical) diagnosis of substance abuse disorder. The prevalence of illicit drugs use here reported for suicide deaths (27%) is higher than in some completed suicide studies17,24–27 although similar to that observed in others.12,13 Cocaine use in suicide subjects showed similar values to those recently reported in U.K.28 and New Mexico.26 A metaanalysis evaluating the acute presence of cannabis in completed suicide established an average rate of 9.5%, smaller than the 16% here obtained.29 The frequency of ethanol presence in the present study (21%) was lower than in some series of suicide cases17,26,28,30 but greater than that obtained by others.5
The selection of an optimal control group for suicide in forensic pathology is a challenge of great difficulty because the consumption of alcohol and illegal drugs is associated with an increased risk for the majority of death types investigated by forensic pathologists.19–22 The control group chosen for the present study was the best available to match suicide group. Since it could exist concerns about how representative of the general population the control sample is, figures were compared with patterns of drug use monitored through surveys in living subjects in years 2012 and 2017 and in the same geographic area.8–11 The information collected by the Basque Government following recommendations of the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) indicated a 12%–13% prevalence of ethanol daily consumption, which is slightly higher than the 8% reported here. Surveys showed that weekly or more frequent cannabis use was present in 9% of the total population, in similar way to that observed in this forensic study (10%). The current or recent consumption of illicit drugs other than cannabis was recognized by 4%–11% of the general living population, concordant with the 8% here observed.8,9 Therefore, the comparison of the toxicological information with population surveys performed in the same area and period of evaluation suggests that control deaths are representative of the general population.
In the present study, ethanol and psychostimulant drugs were the most frequent substances of abuse. Their presence together with cannabis were significantly higher in suicides than in controls when analyzed by unadjusted models. Logistic regression showed that recent consumption of ethanol (OR=4.22), cocaine (OR=2.52), but not cannabis (OR=1.65), increases significantly the risk for suicide after controlling for demographic characteristics and mental disorders. These data agree with other studies showing that acute use of ethanol is associated in a dose-dependent relationship with six- to ten-fold increased risk for suicidal acts.16,30 Short-term cannabis use has also been described as acute triggering of suicidal behaviour and any cannabis exposure enhances 2.56 times the risk of suicide death.29 However, according to others, the recent exposition to cannabis alone and in combination with ethanol is not associated with enhanced odds of attempting suicide.15 In a similar clinical setting, acute presence of psychostimulants including cocaine did not modify the risk of suicide attempts15 whereas a recent metaanalysis of observational studies concluded that regular cocaine users show a 6.3-fold higher standardized mortality rate by suicide,31 which might not necessarily reflect a direct impact of acute drug presence.
The concurrent use of ethanol with illicit drugs is considered an additional risk for suicide beyond the simple summation of the risks for each substance separately.25,32,33 In agreement, a positive association between ethanol and psychostimulant drugs use was observed. The presence of ethanol and psychostimulant drugs would exacerbate the risk of suicide at a much higher level than each substance in its own. These facts also suggest that, at least, the effect of ethanol and cocaine could be more important than cannabis as a potential trigger for suicidal behaviour.
Risk of suicide in relation to sex and ageIt was not surprising the higher frequency of illicit drugs in suicides among males than in females because the prevalence of use in general population is also greater in males.8,9 This is consistent with a metaanalysis reporting that acute cannabis use in suicide deaths is more likely in males than in females.29 Different reports have shown also that ethanol presence in suicide deaths is more prevalent in males.6,32,33 In contrast, the present study did not find such association although the daily use of ethanol in the Basque Country is 2.5-fold higher in male subjects.8,9 In the present forensic sample, estimations after adjusting for other confounding factors seem to indicate that gender does not contribute directly to increase the suicide risk. It would be possible that the association of acute presence of substances of abuse (ethanol and illicit drugs) and other potential factors (psychiatric disorders) with suicide behaviour together with the more elevated consumption rate in males could explain the apparent higher risk of male suicide obtained in unadjusted models. In the current study, it was also found that, even after controlling for other important risk factors, the percentage of deaths by suicide was higher among people in the youth group than in the middle-age adult group. Other studies examining risk of completed suicide beyond associated factors such as acute use of substances and existence of psychiatric disorders are scarce.
Mental disorders and prescribed psychotropic drugsMental disorders have been consistently found to be major risk factors for suicide. The risk of suicide in mental illnesses has been estimated to be around eight times higher than in subjects without these disorders.34,35 As expected, in the present study, the existence of different psychiatric diagnoses were overrepresented in the suicide group. Thus, to be diagnosed of a mental disorder (mainly mood and psychotic disorders) represents a significant risk factor for suicide compared with control group (13-fold higher risk). Besides, for subjects diagnosed of illicit drug abuse/dependence, the risk was also large (5 times higher).
Although drug use is a risk factor for suicide, it is important to highlight that the (by far) most important risk factor in this study is non-addiction related mental disorders. This is in consonance with results of population studies that show a high frequency of these disorders in suicide. The prevalence of mental disorders in suicide oscillates between 50 and 90% according to psychological autopsy studies.3,36 In agreement, the present study detected a 69% frequency of subjects with psychiatric disorders and, in the toxicological analysis, a 63% of psychotropic drugs presence, mainly benzodiazepines, followed by antidepressants and antipsychotics. The use of psychotropic drugs without prescription is very infrequent in the Basque Country, representing around 1% of the psychotropic use.8,9 Therefore, the results confirm the relevant presence of mental illnesses among individuals that committed suicide, and the expected relationship between the psychiatric diagnoses and the prescribed drug obtained in the toxicological analysis.
The association between acute or regular use of substances of abuse and suicide behaviour is complex because of the existence of other risk factors that correlate with both conditions, such as mental illnesses. The use of illicit drugs and ethanol among patients with mental disorders is high. Furthermore, substance abuse may precipitate and worsen psychiatric disorders, such as psychosis, mood disorders and anxiety disorders.37–39 On the other hand, comorbidity of psychiatric and substance use disorders (dual disorders) contributes to raise suicide risk.34,40 In the present study, half of the subjects who had used ethanol and/or illicit drugs had used also prescribed psychotropic drugs, i.e., probably they had a previous psychiatric diagnosis. Taken into consideration the prevalence of mental disorders and the rate of psychotropic drugs use (approximately 10%) in the general population,8,9 the finding of this study suggests an enhanced presence of individuals with comorbid disorders among suicide victims.
Strengths and limitationsThe methodology of the present study provides several strong points: (i) an unselected population of a whole geographic area was studied for a long period of time; (ii) cases and controls were investigated according to the available information obtained from a complete forensic protocol that includes toxicological analysis, which overcomes self-reports or psychological autopsy limitations; (iii) the rate of achieved toxicological analyses in completed suicides was higher (95%) than in other forensic studies27,28; and (iv) findings in a forensic sample bring additional evidence to clinical studies of suicide attempts where fatal events are not usually included.
Postmortem alcohol concentration may be altered by different causes. So, it can be difficult to perform a correct interpretation of the results. In order to minimize this problem, toxicological routine protocol included femoral blood, vitreous fluid and urine samples. On the other hand, a cut-off of 0.5g/L was considered to avoid false positives due to postmortem alcohol production.
The toxicological analysis of the present study only evaluated the role of the acute drug presence, which could have contributed as a trigger for suicide. Hair analysis could have been interesting to better characterize a long-term use of illicit drugs. The observational nature of the study does not allow us to establish a causation relationship between acute presence of substances of abuse and suicide behaviour. Thus, the results might be subject to confounding health and/social factors that were not measured in the present study.
ConclusionsIdentification of acute modifiable factors that might trigger suicide represents an important need, because it would provide approaches to develop useful prevention strategies. According to these results, the proportion of suicides in young and middle-age adults showing exposition to substances of abuse (legal or illicit) is very high. Acute consumption of ethanol and recent use of cocaine seem to be significant precipitating risk factors for suicide. Moreover, the risk increases markedly when both substances are present. The use of illicit substances should be bear in mind when suicide attempts in young people occur. In addition, patients diagnosed of illicit drug abuse/dependence are in greater risk of suicide than people without a previous psychiatric history. Specific strategies should be developed in dual disorder patients in order to prevent suicidal behaviours. The presented data emphasize considering substance use as key factor to promote strategies aimed to reduce mortality from suicide.
Authors’ contributionsStudy conception and design: all authors; acquisition of data: BM; analysis and interpretation of data: all authors; drafting of the manuscript: BM and JJM; critical revision and approval of the definitive version: all authors.
FundingThis work was supported by the Spanish MINECO (PID2019-106404RB-100), the Department of Education (IT1211/19 and IT1512/22) and Department of Health (2018111083) of the Basque Government, and The European Foundation for Alcohol Research (ERAB, EA 1819).
Conflicts of interestThe authors have no conflicts of interest to declare in relation to the present study.
The authors would like to thank the staff members of the Basque Institute of Legal Medicine for their cooperation in the study.