Modifiable lifestyle behaviors are important factors for improving mental health, yet there has been a lack of research studying lifestyle as a multidimensional construct in bipolar disorder (BD). The aim of this cross-sectional study was to compare the lifestyle patterns of individuals with BD in a current mood episode with healthy controls (HCs) using the Short Multidimensional Inventory Lifestyle Evaluation (SMILE).
Materials and methodsThe sample consisted of 46 individuals with BD currently experiencing a depressive or manic episode and 50 HC, assessed using the MINI International Neuropsychiatric Interview, Montgomery-Åsberg Depression Rating Scale (MADRS), and the Young Mania Rating Scale (YMRS). The SMILE scale assesses lifestyle across seven domains: diet and nutrition, substance abuse, physical activity, stress management, restorative sleep, social support, and environmental exposures. Between-groups comparisons were performed based on the presence of a psychiatric diagnosis and the type of BD episode.
ResultsWe found significant differences in the total SMILE score (r=0.75, p<0.001) and in scores from each domain of the scale between BD and HC (p<0.05), where individuals with BD in a depressive or manic episode with or without mixed features reported worse lifestyle across all domains. Differences between individuals with BD in different mood episodes across domains on the SMILE scale were non-significant.
ConclusionFindings from this study highlight the presence of unhealthy lifestyle patterns in people with BD regardless of the polarity of their mood episode. Implementation of multidimensional lifestyle assessments is an essential step toward detecting the clustering of unhealthy lifestyle patterns in BD.
Bipolar disorder (BD) is a severe psychiatric disorder, with an estimated annual prevalence rate of 2% worldwide.1 BD is associated with severe functional impairments in work, family and social settings, as well as with a lower quality of life across all mood states.2,3 The accumulating evidence on challenges in everyday functioning of people with BD,4 along with the high comorbidity rates with other physical and mental health disorders,5 has raised awareness to the burden of BD and the immediate need for effective strategies to reduce it.6
There is growing interest in the field of Lifestyle Medicine (LM), an area of medicine that focuses on improving everyday lifestyle behaviors using evidence-based strategies in order to prevent and intervene on the progression of chronic physical and mental health challenges.7 Unhealthy behaviors in different areas of everyday life can aggregate and have a detrimental cumulative effect on short and long-term health outcomes, such as cardiovascular complications, respiratory diseases, and the risk of mortality.8–10 Lifestyle Psychiatry (LP) is a subspecialty of LM focused on the application of preventive and treatment strategies for mental illnesses following the LM guidelines.11 Recognizing the importance of lifestyle factors for mental health has lagged behind other subspecialties of medicine, although recent reports have shed light on the significance of these factors for reducing the burden of mental disease.12 For many years, different lifestyle areas have been regarded as independent risk factors for mental disorders. However, the fast-growing area of LP suggests a multidimensional focus on lifestyle behaviors for achieving a significant improvement of mental health outcomes.11 According to the American College of Lifestyle Medicine (ACLM), there are six main areas to be targeted: diet, physical activity, avoiding substance use, restorative sleep, stress management, and social support.13
There is evidence showing the close association of symptoms and clinical outcomes of BD with unhealthy behaviors.12 Unhealthy behaviors related to dietary patterns,14 physical activity levels,15 substance abuse,16 sleep quality,17 chronic stress management,18 and social support19 are each linked to poorer clinical outcomes in BD, such as metabolic and cardiovascular diseases, and increased risk of mortality. To date, majority of lifestyle assessments and interventions for BD have been directed to a single lifestyle domain at a time. However, following recent suggestions from the ACLM and findings related to lifestyle and mental health,20,21 supported by evidence from the field of LP, a multidimensional approach can help better understand the various lifestyle areas affected in people with BD, and the clustering of unhealthy behaviors. Moreover, people suffering from BD may need help in different lifestyle areas depending on the current mood state they are experiencing. Hence, an approach that takes into account the multidimensional nature of lifestyle and its likely changes across clinical mood states can pave the way for more personalized, tailored lifestyle interventions to improve the clinical and functional outcomes of individuals suffering from severe mental health conditions, such as BD.
Therefore, the aim of this study was to compare the lifestyle patterns between people with BD in a current mood episode and healthy controls using a multidimensional lifestyle assessment. We also aim to compare the seven lifestyle domains (diet and nutrition, substance abuse, physical activity, stress management, restorative sleep, social support, and environmental exposures) across people with BD in different mood states.
Materials and methodsStudy design and settingThis is a cross-sectional study conducted between October 2021 and July 2022 as part of a larger, cross-sectional study validating a new questionnaire evaluating emotional states in people with BD in a current mood episode. Study interviews were administered at the Mood Disorders Clinic in St. Joseph's Healthcare Hamilton (SJHH) in Hamilton, Canada, or using online video platforms, such as Zoom. Depending on the current COVID-19 restrictions at SJHH and the preference of interested participants, the screening process and data collection were conducted either in-person or remotely. The study was approved by the Hamilton Integrated Research Ethics Board (HiREB) under protocol #8193.
ParticipantsPotential participants that were 18 and older were invited for an interview to determine their eligibility for the study according to the inclusion and exclusion criteria, which differed for the BD and HC groups. Participants from the BD and HC groups were matched by age and sex at the time of recruitment. For the current study, the inclusion criteria for BD were (1) a diagnosis of BD according to DSM-5 criteria using the Mini International Neuropsychiatric Interview (MINI)22 and (2) currently experiencing a depressive, (hypo)manic, or (hypo)manic episode with mixed features episode according to the MINI. Exclusion criteria for the BD group were (1) severe psychotic symptoms, determined according to the presence of current psychotic symptoms on the MINI and the severity of these symptoms based on clinical judgment, (2) severe suicide risk, indicated by a score of ≥17 on the suicidality module of the MINI, and (3) severe cognitive disability that could impact on their understanding of the assessments based on clinical judgment. In contrast, inclusion criteria for healthy controls were (1) absence of any psychiatric diagnosis according to the MINI for DSM-5 and (2) did not demonstrate any severe cognitive disability that could impact their understanding of the assessments based on clinical judgment. The study was advertised using paper flyers in the community, as well as online advertisements posted on advertising websites and social media outlets (Facebook, Instagram, Reddit, and Kijiji). After receiving verbal and written information about the study, all participants provided informed consent prior to the screening interview. Assessments consisted of a diagnostic interview, clinical assessments of current mood state, and lifestyle assessments.
MeasurementsDemographic information was collected for all participants, which included questions regarding the individual's age, sex, years of education, highest educational degree attained, and current occupational status (working/studying). In this study, we only included sociodemographic variables that were assessed in the larger study based on previous validation studies.
Clinical assessmentsAll clinical assessments were conducted by a trained PhD candidate with extensive data collection experience using these instruments.
The MINI was used to evaluate for the presence of psychiatric diagnosis according to the DSM-5.22 For the purpose of the current study, participants in the BD group had to satisfy the criteria for BD, as well as the criteria for a current depressive and/or (hypo)manic episode according to the MINI. In contrast, participants in the HC group were eligible if they did not have a positive screening on any module on the MINI. Presence of psychotic symptoms and suicide risk was also assessed using the MINI.
The Montgomery-Åsberg Depression Rating Scale (MADRS) was used to evaluate the severity of current depressive symptoms.23 The MADRS consists of 10 items that are rated from 0 to 6, evaluating features related to a depressive state within the past week (e.g., sadness, lassitude, pessimism, etc.). The 10 items combine for a total score between 0 and 60. The cut-off score of ≥7 for a current depressive episode was an inclusion criterion in the larger study.24
The Young Mania Rating Scale (YMRS) was used to evaluate the severity of current (hypo)manic symptoms.25 The YMRS is an 11-item scale used to assess the severity of (hypo)manic symptoms within the past week. There are 4 items graded on a 0–8 scale, and 7 items graded on a 0–4 scale, each one assessing a different feature associated with a manic mood state (e.g., irritability, motor activity, decreased need for regular sleep, etc.). The 11 items combine for a total score between 0 and 60. The cut-off score of ≥7 for a current (hypo)manic episode was an inclusion criterion in the larger study.26,27
Participants were considered to be in a current depressive episode if they satisfied the current depressive episode, but not the current (hypo)manic episode criteria on the MINI. Likewise, participants were regarded as currently experiencing a (hypo)manic episode if they satisfied those criteria, but not the criteria for a depressive episode on the MINI. Participants that satisfied the criteria for both depressive and (hypo)manic episode were considered to be experiencing a (hypo)manic episode with mixed features. We grouped manic and manic episodes with mixed features together as there were only 9 participants exclusively in a manic state without mixed features.
Lifestyle assessmentsLifestyle in the previous 30-days was assessed using the Short Multidimensional Inventory Lifestyle Evaluation (SMILE).20 The SMILE is comprised of 43 items evaluating 7 different lifestyle domains: diet and nutrition, substance abuse, physical activity, stress management, restorative sleep, social support, and environmental exposures. Response options are measured on a 4-point Likert scale (always, often, seldom, never), resulting in a maximum possible score of 172 (noting that some questions are reverse-scored). In addition, we considered scores on each domain individually for subanalysis of differences between the groups. Higher scores on the total SMILE scores, as well as on the diet and nutrition (7–28), substance abuse (4–16), physical activity (4–16), stress management (9–36), restorative sleep (5–20), social support (10–40), and environmental exposures (4–16) domains indicated healthier lifestyle.
Statistical analysisThe data were collected directly on REDCap, a secure web platform for collection and storage of data.28 After, the data were transferred to SPSS v.28.0 where the statistical analyses were performed.29 We tested the normality of continuous variables using the Shapiro–Wilk test for normality.30 To describe the sample characteristics between the two groups, HC vs BD, we performed chi-square and Mann–Whitney U tests, for categorical variables and nonparametric continuous data, respectively. We also performed a Mann–Whitney U test to analyze these two groups on the total SMILE scores. We used a non-parametric test for the bivariate analysis because the distribution of the outcome (SMILE scores) was asymmetric. We used Student's t-test for the comparisons of the domains with normal distributions of the scores, and Mann–Whitney U test for the comparisons with asymmetric distribution of the scores. We created two box plot graphs using the Prism GraphPad v.9 to demonstrate the findings of the comparison between HC and BD, and the comparison between HC, BD in a depressive episode, and BD in a manic (with and without mixed features) episode across the different SMILE domains (Figs. 1 and 2). We also calculated effect size of the differences between the groups using r values for nonparametric comparisons and Cohen's d for parametric comparisons. We calculated the post hoc statistical power of the main comparison using Epi Info™. Multivariate linear regression was performed to evaluate the effect of independent factors (predictors) on the SMILE score. The analyses included variables that presented an association of p<0.20 with the outcome (SMILE scores). We did not include the ‘highest degree of education’ variable in this analysis, as it measures the same construct as the years of education variable. The final model was reached using a manual stepwise removal of each non-statistically significant variable. Furthermore, we compared total scores on the SMILE scale, as well as scores for each domain of the SMILE across HCs, BD in a current depressive episode, and BD in a current manic (with and without mixed features) episode. Significance for all comparisons was set at p<0.05.
Comparison of total SMILE scores between healthy controls (HCs) and individuals with bipolar disorder (BD) in a current mood episode. Healthy individuals reported significantly higher median scores on the SMILE scale (median: 133.5 [IQR: 125.75–141.25]) than individuals with BD in a current mood episode (median: 104.0 [IQR: 95.0–115.0], p<0.001), suggesting unhealthier behaviors in individuals with BD.
BD: bipolar disorder; HC: healthy control; SMILE: Short Multidimensional Inventory Lifestyle Evaluation.
Comparison of SMILE scores across different lifestyle domains between healthy individuals, individuals with bipolar disorder in a depressive episode, and individuals with bipolar disorder in a manic or manic with mixed features episode.
BD – D: bipolar disorder in a depressive episode; BD – M/M: bipolar disorder in a manic or manic with mixed features episode; HC: healthy control; SMILE: Short Multidimensional Inventory Lifestyle Evaluation; *p<0.05; **p<0.001.
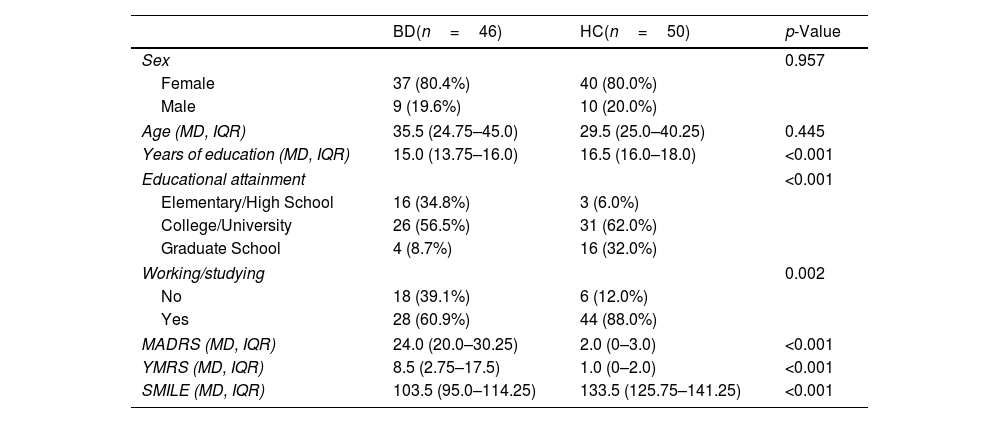
The total sample of this study consisted of 96 participants (46 BD and 50 HC). The sociodemographic characteristics of the sample are described in Table 1. There were no significant differences between groups regarding sex (p=0.957) or age (p=0.445). Consistent with the well-known educational and occupational burden of BD, the HC group had completed significantly more years of education (p<0.001), attained a higher educational degree (p<0.001), and were more likely to be working/studying (88.0%) at the time of assessment than the BD group (60.9%, p=0.002). The groups also differed in scores on the clinical assessments, as expected. The HC group had significantly lower median scores on the MADRS (2.0, IQR: 0–3.0) and on the YMRS (1.0, IQR: 0–2.0) than the BD group (MADRS: 24.0, IQR: 20.0–30.5, p<0.001; YMRS: 8.5, IQR: 2.75–17.5, p<0.001).
Characteristics of the sample according to the diagnostic groups.
| BD(n=46) | HC(n=50) | p-Value | |
|---|---|---|---|
| Sex | 0.957 | ||
| Female | 37 (80.4%) | 40 (80.0%) | |
| Male | 9 (19.6%) | 10 (20.0%) | |
| Age (MD, IQR) | 35.5 (24.75–45.0) | 29.5 (25.0–40.25) | 0.445 |
| Years of education (MD, IQR) | 15.0 (13.75–16.0) | 16.5 (16.0–18.0) | <0.001 |
| Educational attainment | <0.001 | ||
| Elementary/High School | 16 (34.8%) | 3 (6.0%) | |
| College/University | 26 (56.5%) | 31 (62.0%) | |
| Graduate School | 4 (8.7%) | 16 (32.0%) | |
| Working/studying | 0.002 | ||
| No | 18 (39.1%) | 6 (12.0%) | |
| Yes | 28 (60.9%) | 44 (88.0%) | |
| MADRS (MD, IQR) | 24.0 (20.0–30.25) | 2.0 (0–3.0) | <0.001 |
| YMRS (MD, IQR) | 8.5 (2.75–17.5) | 1.0 (0–2.0) | <0.001 |
| SMILE (MD, IQR) | 103.5 (95.0–114.25) | 133.5 (125.75–141.25) | <0.001 |
IQR: interquartile range; MADRS: Montgomery-Åsberg Depression Rating Scale; MD: median; SMILE: Short Multidimensional Inventory Lifestyle Evaluation; YMRS: Young Mania Rating Scale.
Our analysis revealed significant differences with a large effect size on the total SMILE score between the HC (median: 133.5 [IQR: 125.75–141.25]) and BD (median: 103.5 [IQR: 95.0–114.25], r=0.75, p<0.001) groups (Fig. 1). The post hoc statistical power for the comparison between BD and HC was 100%. These differences indicate a significantly worse lifestyle among individuals with BD than healthy controls. Furthermore, our analysis revealed significantly lower scores in BD in comparison to HC with a large effect size across all domains on the SMILE scale (Table 2).
Comparison of SMILE scores across healthy controls and individuals with BD in different mood states.
| HC(n=50) | BD(n=46) | p-Value | Effect size | |
|---|---|---|---|---|
| SMILE Totala | 133.5 (125.75–141.25) | 103.5 (95.0–114.25) | <0.001 | 0.75 |
| SMILE – Dieta | 22.0 (19.0–23.0) | 17.5 (14.75–20.0) | <0.001 | 0.53 |
| SMILE – Physical Activitya | 11.0 (9.0–12.0) | 8.0 (7.0–9.0) | <0.001 | 0.53 |
| SMILE – Substance Usea | 16.0 (15.0–16.0) | 13.0 (12.0–16.0) | <0.001 | 0.45 |
| SMILE – Restorative Sleepa | 15.0 (14.0–17.0) | 12.0 (10.0–13.0) | <0.001 | 0.63 |
| SMILE – Stress Managementb | 26.58 (±4.01) | 19.3 (±4.07) | 0.001 | 1.87 |
| SMILE – Social Supporta | 34.0 (30.0–37.0) | 26.5 (22.0–29.0) | 0.001 | 0.66 |
| SMILE – Environment Exposureb | 10.28 (±2.23) | 8.48 (±2.23) | 0.001 | 0.85 |
BD: bipolar disorder; HC: healthy control; SMILE: Short Multidimensional Inventory Lifestyle Evaluation.
In the final adjusted linear regression model, we included years of education, current working/studying status, and diagnosis (HC or BD) as predictors of SMILE scores. After the removal of the least significant factor in the model (currently working/studying), we performed another linear regression with years of education and SMILE scores. Years of education was also non-significant in the model, and after the removal of this factor, diagnosis (HC/BD) remained as the only significant predictor of total SMILE scores, where a diagnosis of BD was predictive of worse scores on the SMILE. The multivariate linear regression models are presented in Supplementary Material 1.
Lifestyle across mood statesFor the analysis of scores on the SMILE scale across different mood states, we included 26 participants in a depressive state, 20 participants in a manic state (manic without mixed features=9, manic with mixed features=11), and 50 healthy controls. In addition to the total SMILE scores, we analyzed the scores of the 7 subdomains of the SMILE scale across the 3 groups (Table 3 and Fig. 2). Once again, participants in both BD groups had significantly lower median scores on the total SMILE scale, as well as all 7 subdomains of the scale than HC (p<0.05). In contrast, BD in a depressive episode and BD in a manic (with and without mixed features) episode did not show any differences in total SMILE scores or in any of the subdomains of the scale.
Comparison of SMILE scores across healthy controls and individuals with BD in different mood states.
| HC (n=50) | BD – Depressive (n=26) | BD – Manic/Mixed (n=20) | Between groups comparisons | Effect size | |
|---|---|---|---|---|---|
| SMILE Totala | 133.5 (125.75–141.25) | 100.5 (94.75–111.5) | 106.0 (97.25–118.0) | HC>D**HC>M/M**D=M/M | 0.750.640.18 |
| SMILE – Dieta | 22.0 (19.0–23.0) | 17.0 (14.75–19.25) | 18.0 (14.25–21.75) | HC>D**HC>M/M*D=M/M | 0.590.370.12 |
| SMILE – Physical Activitya | 11.0 (9.0–12.0) | 7.5 (7.0–9.0) | 9.0 (7.25–9.75) | HC>D**HC>M/M**D=M/M | 0.550.430.2 |
| SMILE – Substance Usea | 16.0 (15.0–16.0) | 14.5 (12.0–16.0) | 13.0 (12.0–16.0) | HC>D**HC>M/M**D=M/M | 0.380.490.09 |
| SMILE – Restorative Sleepa | 15.0 (14.0–17.0) | 12.0 (11.0–13.0) | 11.5 (10.0–12.75) | HC>D**HC>M/M**D=M/M | 0.570.590.13 |
| SMILE – Stress Managementb | 26.58 (±4.01) | 18.54 (±3.82) | 20.3 (±4.27) | HC>D**HC>M/M**D=M/M | 2.051.520.43 |
| SMILE – Social Supporta | 34.0 (30.0–37.0) | 25.0 (22.0–29.0) | 27.0 (21.75–29.75) | HC>D**HC>M/M**D=M/M | 0.670.530.11 |
| SMILE – Environment Exposureb | 10.28 (±2.23) | 8.08 (±2.28) | 9.0 (±1.59) | HC>D**HC>M/M**D=M/M | 0.920.660.47 |
D: depressive; HC: healthy control; M/M: Manic/Mixed; SMILE: Short Multidimensional Inventory Lifestyle Evaluation.
To our knowledge, this is the first cross-sectional study evaluating differences in lifestyle between healthy individuals and people with BD in a current mood episode, using a multidimensional lifestyle approach based on contemporary notions of lifestyle. Our findings revealed significantly healthier lifestyle across all domains in healthy controls in comparison to BD in a current depressive, manic, or manic with mixed features state. Regardless of the type of mood episode they were experiencing, people with BD reported unhealthier lifestyle than age and sex-matched healthy individuals. Intriguingly, individuals with BD reported worse lifestyle across all domains on the scale, suggesting that all areas of their everyday life are affected during mood episodes.
Our findings are in line with previous reports suggesting differences between BD and healthy individuals on these lifestyle domains. In comparison to healthy controls, individuals with BD have showed unhealthier dietary patterns and increased intake of obesogenic nutrients,31–33 significantly lower physical activity and higher rates of sedentary behavior,34 and higher rates of sleep–wake and circadian rhythm disruptions.35,36 Recent reports have suggested specific diets may be effective for preventing the recurrence of depressive episodes, such as a Mediterranean diet with extra virgin olive oil.37 Novel, innovative studies are also exploring the effects of individualized exercise programs for improving functional status of people with BD.38 Moreover, previous findings have also suggested the reduced use of adaptive coping strategies (such as stress management techniques and social relationships) and increased use of maladaptive coping strategies (such as substance abuse) in individuals with BD in comparison to healthy controls.39 There is evidence that unhealthy lifestyles such as low physical activity and poor sleep quality may further compound the neurocognitive dysfunction associated with BD and may cumulatively aggravate the social and occupational disability of these patients.40
Furthermore, the clustering of unhealthy lifestyle behaviors across different areas, such as unhealthy eating, physical activity, and substance use patterns, has been associated with an increased risk of depressive symptoms, higher levels of psychological distress, lower vitality, and lower quality of life.41–45 The patterns in different areas of everyday life are intertwined and dependent on each other, and the formation of unhealthy habits can lead to detrimental effects on the individual's physical and mental well-being. Importantly, our analysis highlights the clustering of unhealthy lifestyle domains across individuals with BD in depressive, manic, and manic with mixed features episodes. Importantly, previous findings have also suggested the presence of unhealthy behaviors in euthymic individuals with BD, such as unhealthy dietary patterns, physical inactivity, hindered personal relationships, and sleep disturbances.46–49
The implementation of a multidimensional lifestyle assessment is very important for both detecting the clustering of unhealthy behaviors in everyday life routines of individuals with BD in any mood state and developing more informed and personalized lifestyle-based interventions. Of note, all lifestyle behaviors are modifiable, and growing evidence supports that multimodal strategies targeting exercise, nutrition and wellness are feasible and effective to improve mental and somatic health in individuals with BD.50,51 The clustering of unhealthy behaviors from different domains may lead to more severe clinical trajectories and increase the rates of physical and mental health comorbidities with BD. The main lifestyle areas, as recognized by LP, are deemed to be “modifiable” domains, with assessments and subsequent interventions in these domains showing promising results for improving mental health outcomes and reducing the burden of these disorders.11 A multidimensional approach to evaluating lifestyle behaviors in BD should be implemented in the clinical setting, as it allows for a more detailed assessment of the person's everyday behaviors and the complex interactions between these behaviors and symptoms of BD, which would be an essential step toward developing more personalized, tailored interventions for improving clinical outcomes and quality of life in individuals with BD.
LimitationsFindings from our study should be interpreted considering some limitations. Considering that this cross-sectional study was part of a larger study designed to validate an emotional reactivity scale in people with BD in a current mood episode, we did not include any data of euthymic individuals with BD, which would be helpful for understanding whether unhealthy lifestyles are associated to the disorder even when individuals are asymptomatic. Also, the SMILE scale has not been validated for use in a BD population yet, however, the validation study is currently ongoing. Furthermore, 37 out of the 46 individuals in the BD group had a positive screening for a depressive episode, which prevented us from including a manic only group in our analysis and led to the grouping of individuals in manic and manic with mixed features states. Also, our sample predominantly consisted of females, although this could be explained by the higher prevalence of females than males with BD.6 Lastly, we did not collect information regarding the socio-economic status, current medications use of participants, comorbid medical conditions and other psychiatric disorders which may be related to the observed behaviors on some of the SMILE domains. Despite these limitations, this is the first cross-sectional study to compare lifestyle across healthy individuals and people with BD in different mood episodes using a multidimensional approach based on contemporary notions of lifestyle.
ConclusionFindings from this study confirm the association between multidimensional unhealthy lifestyle behaviors and symptomatic people with BD. We found that symptomatic individuals with BD reported significantly unhealthier lifestyle behaviors than healthy controls. This association was present across multiple areas of lifestyle, an important consideration for the onset and progression of physical and psychiatric comorbidities in BD. However, there were no differences among individuals with BD across different mood episodes, indicating unhealthy lifestyle patterns in BD regardless of the polarity of the mood episode. There is a strong need for future research on implementing a multidimensional approach to lifestyle assessments in BD across all mood states of the disorder, including euthymia, and evaluating the clustering of unhealthy lifestyle behaviors across different areas of everyday life that could potentially lead to worse clinical and functional outcomes for the affected individuals.
Authors’ contributionsConceptualization – MS, TAC, FK; data collection – MS; formal analysis – MS, TAC; writing original draft and visualization – MS; writing – review & editing – RDB, VBM, BNF, LM, FK, TAC; supervision – TAC, FK.
FundingThis research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interestMS, TAC, BNF, LM, RDB, and FK have nothing to disclose.
VB-M has been a consultant, advisor or Continuing Medical Education (CME) speaker over the last 3 years for the following companies: Angelini, Lundbeck, and Nutrición Médica, all of them unrelated to the present work. FK has been a consultant for Janssen – Johnson & Johnson, unrelated to the present work.
The authors thank all the participants involved in this study. Dr. de Azevedo Cardoso acknowledges her postdoctoral fellowship from the Canadian Institutes of Health Research (CIHR).











![Comparison of total SMILE scores between healthy controls (HCs) and individuals with bipolar disorder (BD) in a current mood episode. Healthy individuals reported significantly higher median scores on the SMILE scale (median: 133.5 [IQR: 125.75–141.25]) than individuals with BD in a current mood episode (median: 104.0 [IQR: 95.0–115.0], p<0.001), suggesting unhealthier behaviors in individuals with BD. BD: bipolar disorder; HC: healthy control; SMILE: Short Multidimensional Inventory Lifestyle Evaluation. Comparison of total SMILE scores between healthy controls (HCs) and individuals with bipolar disorder (BD) in a current mood episode. Healthy individuals reported significantly higher median scores on the SMILE scale (median: 133.5 [IQR: 125.75–141.25]) than individuals with BD in a current mood episode (median: 104.0 [IQR: 95.0–115.0], p<0.001), suggesting unhealthier behaviors in individuals with BD. BD: bipolar disorder; HC: healthy control; SMILE: Short Multidimensional Inventory Lifestyle Evaluation.](https://static.elsevier.es/multimedia/29502853/0000001600000004/v2_202312091027/S1888989123000113/v2_202312091027/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)

