Suicide attempts are an important predictor of completed suicide and may differ in terms of severity of medical consequences or medical lethality. There is little evidence on serious suicide attempt (SSA) and very few studies have compared SSA with non-SSA.
ObjectiveThe aim of this multisite, coordinated, cohort study was to analyze the role of clinical variables and the sociodemographic and psychological risk factors of SSA.
MethodIn this multisite, coordinated, cohort study, 684 participants (222 for the mild suicide attempt group, 371 for the moderate suicide attempt group and 91 for the SSA group) were included in the study. Ordinal regression models were performed to analyze the predictor variables of SSA.
ResultsEarly physical abuse (OR=1.231) and impulsivity (OR=1.036) were predictors of SSA, while depressive symptoms were associated with a lower risk of SSA.
ConclusionEnvironmental and psychological factors as physical abuse and impulsivity are related with severe suicide severity. These findings will help to develop strategies to prevent suicide and may be considered for the treatment and management of suicide.
Suicide attempts are an important predictor of completed suicide,1 and are themselves a serious public health problem. It is estimated that there are 20 attempts for each completed suicide.2 Suicide attempt may differ in terms of method used, type of attempt (that includes attitudes and expectancies of fatality, premeditation for the suicidal act, the method's lethality and/or communication with others) and severity of medical consequences or medical lethality.3 Within the broad spectrum of suicide attempts, a serious suicide attempt (SSA) has been conceptualized in terms of medical lethality from two dimensions, the suicidal attempt's physiological consequences and post-attempt medical procedures.4,5 SSA is defined as a suicide attempt that causes a serious physical injury requiring intensive medical treatment. Individuals who made SSA have greater risk of death by suicide compared to non-serious suicide attempters6–11 and are twice as likely as other suicide attempters to subsequently complete suicide.12 Moreover, SSA and suicide attempts that result in completed suicide share similar clinical and behavioural characteristics and have similar risk factors13–15 so represent a crucial subgroup to understand and study suicide behaviour.
SSA is considered a multifactorial phenomenon.16 The studies that have examined the risk factors associated with a SSA have shown that psychosocial factors may play a critical role. Among men, psychological problems and conduct disorders were frequently associated with SSA,17 while depressive symptoms are not related to suicide outcome. Some studies have found that psychosocial stressors like school/work problems and psychopathological factors, like agitation, were related to more SSA.18 In a systematic review about psychological risk factors,4 conclude that in a devastating state of mental pain, higher levels of impulsivity and aggression may become decisive SSA facilitators, especially in those patients with difficulties in communication and with scarce social connectedness. In addition, childhood trauma has been related to general suicide risk.19 Specifically, childhood and family adversities, such as sexual/physical abuse or negligence parenting, are significantly higher among serious suicide attempters.13,20 This association has been related with unhealthy attachment.21 Other studies have found other risk factors for the SSA, such as some sociodemographic variables like being older,4,22 family history of suicide and/or history of medical illnesses.16
Since SSA may share similar clinical characteristics to attempts leading to completed suicide, studying the variables that predict SSA may allow understanding suicide and identifying pathophysiological mechanisms involved in suicide risk. To date, few studies have investigated the SSA. Moreover, studies that have approached SSA have obtained unconclusive results and very few studies have compared SSA with non-SSA with large sample sizes.4
Due to the scarcity of research on this key public health hazard and considering that there is not clear evidence about the risk factors associated with SSA, the objective of this multisite, coordinated, cohort study was to analyze the role of clinical variables and the sociodemographic and psychological risk factors SSA presence and features.
MethodsDesignIt is a multisite, coordinated, cohort study. Participants were recruited as part of the “Suicide Prevention and Intervention Study (SURVIVE)” study from ten recruitment sites distributed across Spain (Hospital Clínic; Corporació Sanitària Parc Taulí; Parc de Salut Mar, Hospital Clínico San Carlos; Hospital Universitario La Paz, Hospital Universitario Araba-Santiago, Hospital Universitario Virgen del Rocio and Hospital Universitario Central de Asturias). The study was approved by the clinical research ethics committees of all participating centres in the SURVIVE study. The study protocol is described in the article conducted by Pérez et al.23 This project is composed by research groups of 11 university hospitals distributed in Spain, and patients were recruited from their emergency departments. Inclusion criteria were (a) at least 18 years-old and (b) attempted suicide with a recognized dead intention. Exclusion criteria were (a) not being mental or emotionally able to carry out the initial interview and (b) not report a clear suicidal intention.
SubjectsPatients were required to be 18 years or older and to give written informed consent to participate in the study. Moreover, they must have been admitted at hospital emergency department due to suicidal attempt. Suicide attempt was defined as a “self-initiated sequence of behaviours by an individual who, at the time of the initiation, expected that the set of actions would lead to his or her own death”.24 Assessments have been conducted within 10 days from the suicide attempt and data collection was performed between 17th December 2020 and 8th September 2022. Data was collected by researchers of every site.
The exclusion criteria to participate were having incapacity to give informed consent, having lack of fluency in Spanish and/or taking part in another clinical study which, in the opinion of the investigator, is likely to interfere with the objectives of the SURVIVE study.
Patients were divided into three groups according to the suicide attempt severity defined by the level of real lethality/medical injuries measured by the Columbia Suicide Rating Scale.25 The scale measures the severity of the lethality/medical injuries with a scale from 0 (no injury or very minor physical injuries) to 5 (death). The groups were defined according to the following scores ranges: mild suicide attempt group (score of 0–1); moderate suicide attempt group (score equal to 2); and SSA group (scores of 3–4).
MeasuresSocio-demographic (sex, age, level of education, marital and employment status), clinical and the characteristics of the suicidal behaviour data were collected using a clinical interview. Patient assessment was conducted within 15 days of the suicide attempt.
Patients were diagnosed using the International Neuropsychiatric Interview (MINI).26 It is a short diagnostic structured interview structured by diagnostic modules according to Diagnostic and Statistical Manual of Mental Disorders (DSM V) criteria.
Depressive and anxiety symptoms were assessed by the Patient Health Questionnaire (PHQ-9)27 and the General Anxiety Disorder-7 (GAD-7),28 respectively.
Impulsivity was evaluated with the Barrat Impulsivity Scale (BIS-11),29 a 30-item questionnaire that measures the motor impulsiveness, the attentional impulsiveness, and the non-planned impulsiveness.
Adherence to the pharmacological treatment was assessed using the Morisky Medication Adherence Scale (MMAS).30
The variables related to suicide attempt were assessed with the Columbia Suicide Rating Scale (C-SSRS)25 and the Acquired Capability for Suicide Scale-Fearlessness about Death (ACSS-FAD).31 The C-SSRS is a clinician-administered suicidal ideation and behaviour rating scale that assesses severity and intensity of suicidal ideation, types of suicidal behaviour, and lethality of suicide attempts. The ACSS-FAD is a seven-item self-report that measures the levels of the acquired capability for suicide.
Health-related quality of life was assessed with the EuroQoL-5D32 which measures the health problems into five dimensions and a Visual Analogue Scale corresponding to the current state of the subject's health.
Childhood traumatic experiences were collected with the Childhood Trauma Questionnaire (CTQ-SF),33 which retrospectively assess childhood trauma across five subscales: sexual abuse, physical abuse, emotional abuse, physical neglect and emotional neglect.
Lastly, the 8-item version of the Reflective Functioning Questionnaire (RFQ)34 was used to measure the levels of both certainty and uncertainty about one's own mental processes.
Statistical analysesSPSS Statistics for Windows (version 23.0) was used for the statistical analysis, with the significance level set at p≤0.05.
Differences in sociodemographic, clinical and suicide attempt characteristics between three groups of suicide attempt severity were analyzed using the X2 test for categorical variables and ANOVA followed by Tukey post hoc testing for continuous variables.
Ordinal regression models with backward stepwise were performed to analyze the predictor variables of suicide attempt severity. Initially, all variables were considered as potential risk factors of severity and were included in the model as independent variables taking as dependent the severity group variable. Those variables which remained significant were maintained in the final model.
These models were also used to study the relation between the suicide attempt method and the lethality that produces. Those significant risk factors previously found were included as covariate variables and the method as predictor variable. As the suicide attempt method variable had several categories, the firearms were selected as the reference category.
Data is presented as β coefficients, p value, 95% confidence interval and odds ratio (OR).
ResultsSociodemographic, clinical and suicide attempt characteristics of the sampleA total of 684 patients (222 for the mild suicide attempt group, 371 for the moderate suicide attempt group and 91 for the SSA group) who met inclusion criteria and consented to participate were included in the study.
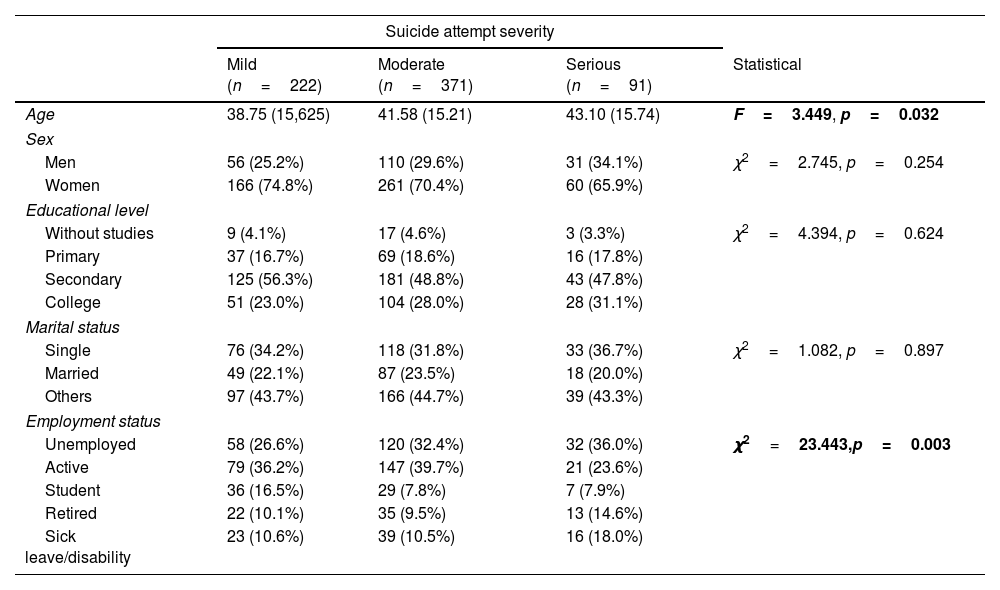
The majority of the sample (71.2%) were women. The mean age of the sample was 40.86 (±15.48) and 33.2% were single. Half of participants (51.1%) had secondary education and 36.5% were active workers. There were no statistically significant differences between the three groups on sociodemographic characteristics except on age and employment status. The SSA group had a mean age higher than mild suicide attempt group (F=3.449, p=0.032) and a higher percentage of unemployed (36%) compared to the moderate (32.4%) and mild (26.6%) suicide attempt groups, respectively (χ2=23.443, p=0.003) (Table 1).
Sociodemographic characteristics of the sample.
| Suicide attempt severity | ||||
|---|---|---|---|---|
| Mild (n=222) | Moderate (n=371) | Serious (n=91) | Statistical | |
| Age | 38.75 (15,625) | 41.58 (15.21) | 43.10 (15.74) | F=3.449, p=0.032 |
| Sex | ||||
| Men | 56 (25.2%) | 110 (29.6%) | 31 (34.1%) | χ2=2.745, p=0.254 |
| Women | 166 (74.8%) | 261 (70.4%) | 60 (65.9%) | |
| Educational level | ||||
| Without studies | 9 (4.1%) | 17 (4.6%) | 3 (3.3%) | χ2=4.394, p=0.624 |
| Primary | 37 (16.7%) | 69 (18.6%) | 16 (17.8%) | |
| Secondary | 125 (56.3%) | 181 (48.8%) | 43 (47.8%) | |
| College | 51 (23.0%) | 104 (28.0%) | 28 (31.1%) | |
| Marital status | ||||
| Single | 76 (34.2%) | 118 (31.8%) | 33 (36.7%) | χ2=1.082, p=0.897 |
| Married | 49 (22.1%) | 87 (23.5%) | 18 (20.0%) | |
| Others | 97 (43.7%) | 166 (44.7%) | 39 (43.3%) | |
| Employment status | ||||
| Unemployed | 58 (26.6%) | 120 (32.4%) | 32 (36.0%) | χ2=23.443,p=0.003 |
| Active | 79 (36.2%) | 147 (39.7%) | 21 (23.6%) | |
| Student | 36 (16.5%) | 29 (7.8%) | 7 (7.9%) | |
| Retired | 22 (10.1%) | 35 (9.5%) | 13 (14.6%) | |
| Sick leave/disability | 23 (10.6%) | 39 (10.5%) | 16 (18.0%) | |
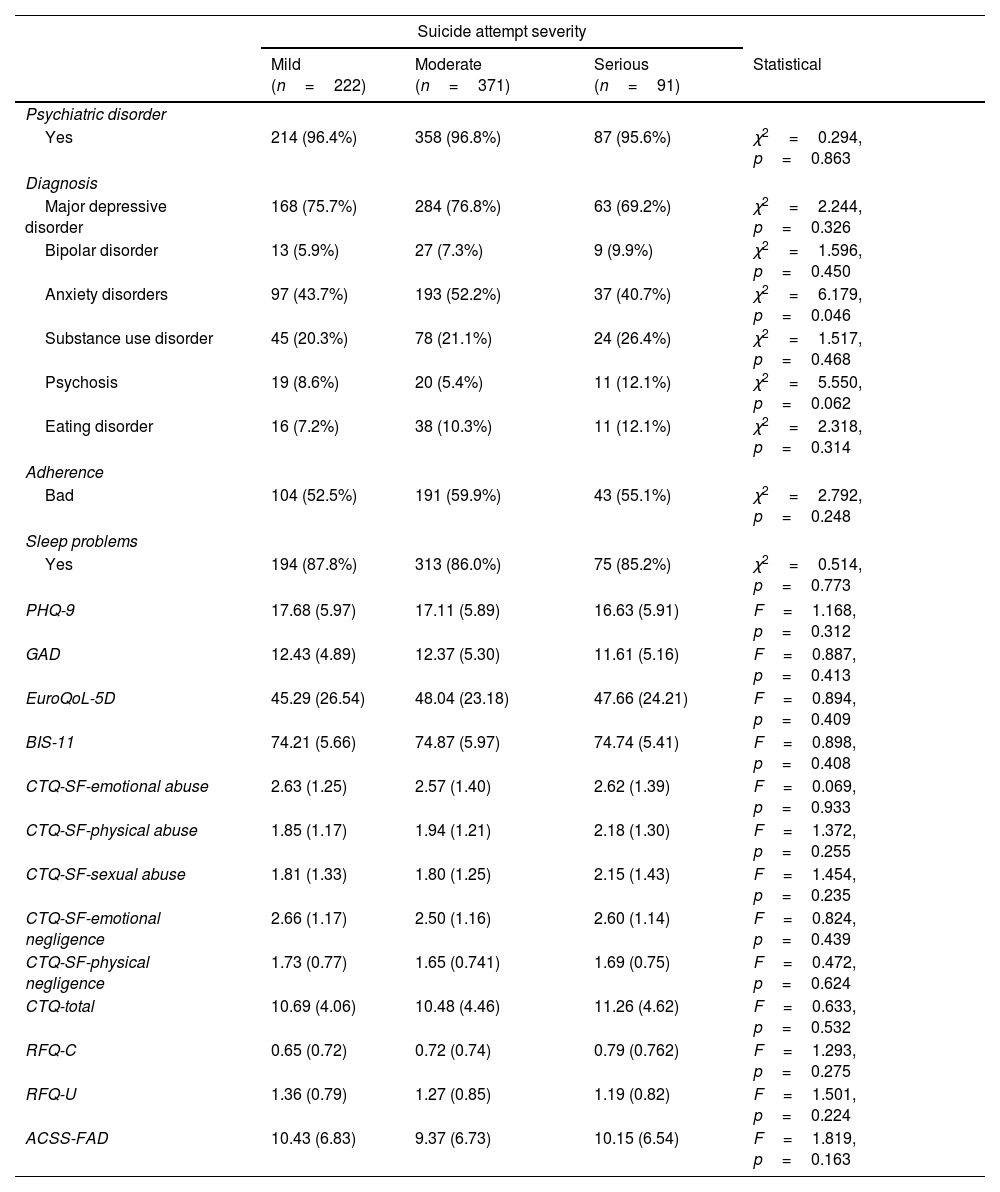
Regarding the clinical characteristics, the majority of patients had a psychiatric diagnosis (96.5%). Major depressive disorder was the most frequent, with no significant differences between groups. Anxiety disorders were the second most common disorder, especially in the moderate suicide attempt (52.2%) compared to mild (43.7%) and serious (40.7%) groups (χ2=6.179, p=0.046). Despite not reaching significant level, it was observed a tendency to a higher percentage of patients with schizophrenia or psychotic disorder that commit a SSA (χ2=5.550, p=0.062). There were no significant differences in the other clinical variables (Table 2).
Clinical characteristics of the sample.
| Suicide attempt severity | ||||
|---|---|---|---|---|
| Mild (n=222) | Moderate (n=371) | Serious (n=91) | Statistical | |
| Psychiatric disorder | ||||
| Yes | 214 (96.4%) | 358 (96.8%) | 87 (95.6%) | χ2=0.294, p=0.863 |
| Diagnosis | ||||
| Major depressive disorder | 168 (75.7%) | 284 (76.8%) | 63 (69.2%) | χ2=2.244, p=0.326 |
| Bipolar disorder | 13 (5.9%) | 27 (7.3%) | 9 (9.9%) | χ2=1.596, p=0.450 |
| Anxiety disorders | 97 (43.7%) | 193 (52.2%) | 37 (40.7%) | χ2=6.179, p=0.046 |
| Substance use disorder | 45 (20.3%) | 78 (21.1%) | 24 (26.4%) | χ2=1.517, p=0.468 |
| Psychosis | 19 (8.6%) | 20 (5.4%) | 11 (12.1%) | χ2=5.550, p=0.062 |
| Eating disorder | 16 (7.2%) | 38 (10.3%) | 11 (12.1%) | χ2=2.318, p=0.314 |
| Adherence | ||||
| Bad | 104 (52.5%) | 191 (59.9%) | 43 (55.1%) | χ2=2.792, p=0.248 |
| Sleep problems | ||||
| Yes | 194 (87.8%) | 313 (86.0%) | 75 (85.2%) | χ2=0.514, p=0.773 |
| PHQ-9 | 17.68 (5.97) | 17.11 (5.89) | 16.63 (5.91) | F=1.168, p=0.312 |
| GAD | 12.43 (4.89) | 12.37 (5.30) | 11.61 (5.16) | F=0.887, p=0.413 |
| EuroQoL-5D | 45.29 (26.54) | 48.04 (23.18) | 47.66 (24.21) | F=0.894, p=0.409 |
| BIS-11 | 74.21 (5.66) | 74.87 (5.97) | 74.74 (5.41) | F=0.898, p=0.408 |
| CTQ-SF-emotional abuse | 2.63 (1.25) | 2.57 (1.40) | 2.62 (1.39) | F=0.069, p=0.933 |
| CTQ-SF-physical abuse | 1.85 (1.17) | 1.94 (1.21) | 2.18 (1.30) | F=1.372, p=0.255 |
| CTQ-SF-sexual abuse | 1.81 (1.33) | 1.80 (1.25) | 2.15 (1.43) | F=1.454, p=0.235 |
| CTQ-SF-emotional negligence | 2.66 (1.17) | 2.50 (1.16) | 2.60 (1.14) | F=0.824, p=0.439 |
| CTQ-SF-physical negligence | 1.73 (0.77) | 1.65 (0.741) | 1.69 (0.75) | F=0.472, p=0.624 |
| CTQ-total | 10.69 (4.06) | 10.48 (4.46) | 11.26 (4.62) | F=0.633, p=0.532 |
| RFQ-C | 0.65 (0.72) | 0.72 (0.74) | 0.79 (0.762) | F=1.293, p=0.275 |
| RFQ-U | 1.36 (0.79) | 1.27 (0.85) | 1.19 (0.82) | F=1.501, p=0.224 |
| ACSS-FAD | 10.43 (6.83) | 9.37 (6.73) | 10.15 (6.54) | F=1.819, p=0.163 |
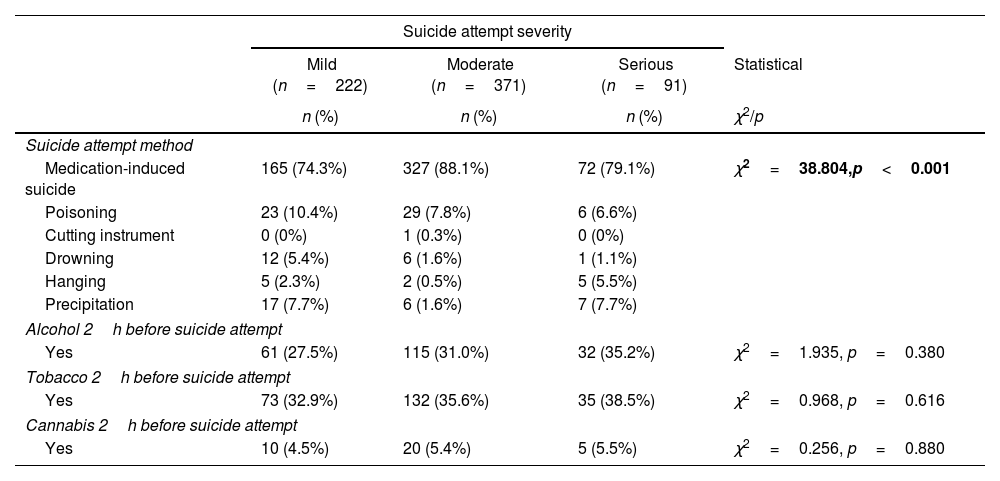
With respect to characteristics of suicide attempt, 28% of the sample had a family history of suicide. The medication-induced suicide was the most used method across patient groups (82.5%) (χ2=38.804, p<0.001). Besides, this method produced more frequently moderate suicide attempts than mild or serious attempts (88.1% vs 74.3% and 79.1%, respectively). The suicide attempt characteristics of the participants of the three groups are presented in Table 3.
Suicide attempt characteristics of the sample.
| Suicide attempt severity | ||||
|---|---|---|---|---|
| Mild (n=222) | Moderate (n=371) | Serious (n=91) | Statistical | |
| n (%) | n (%) | n (%) | χ2/p | |
| Suicide attempt method | ||||
| Medication-induced suicide | 165 (74.3%) | 327 (88.1%) | 72 (79.1%) | χ2=38.804,p<0.001 |
| Poisoning | 23 (10.4%) | 29 (7.8%) | 6 (6.6%) | |
| Cutting instrument | 0 (0%) | 1 (0.3%) | 0 (0%) | |
| Drowning | 12 (5.4%) | 6 (1.6%) | 1 (1.1%) | |
| Hanging | 5 (2.3%) | 2 (0.5%) | 5 (5.5%) | |
| Precipitation | 17 (7.7%) | 6 (1.6%) | 7 (7.7%) | |
| Alcohol 2h before suicide attempt | ||||
| Yes | 61 (27.5%) | 115 (31.0%) | 32 (35.2%) | χ2=1.935, p=0.380 |
| Tobacco 2h before suicide attempt | ||||
| Yes | 73 (32.9%) | 132 (35.6%) | 35 (38.5%) | χ2=0.968, p=0.616 |
| Cannabis 2h before suicide attempt | ||||
| Yes | 10 (4.5%) | 20 (5.4%) | 5 (5.5%) | χ2=0.256, p=0.880 |
n (%), number and percentage of individuals per group.
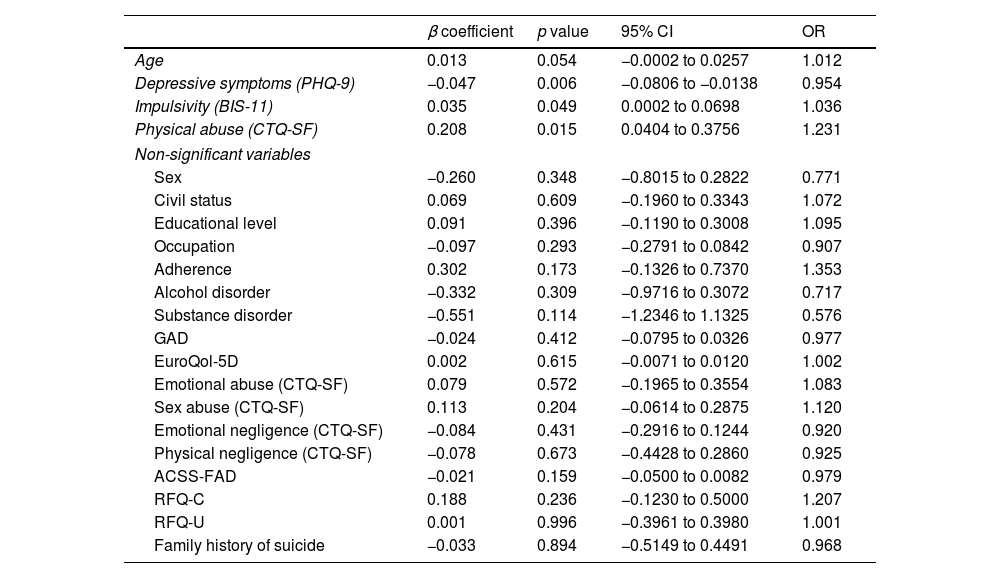
Ordinal regression models were performed including all variables as independent predictor variables and the suicide attempt severity groups as dependent variable. After the backward procedure, the final model included age, depressive symptoms, impulsivity and physical abuse.
Except for depressive symptoms, all variables were directly related to SSA: age (non-significant association), impulsivity and physical abuse, so that a higher value in these variables increased the probability of having had a more severe suicide attempt. In fact, physical abuse was proven to have a higher impact on suicide attempt severity (OR=1.231). Regarding depressive symptoms, the model revealed that they could be a protective factor as they were inversely related with suicide attempt severity. In fact, those patients with higher values in PHQ-9 scale had more probably milder suicide attempts than those with lower values (Table 4).
Predictors of suicide attempt severity.
| β coefficient | p value | 95% CI | OR | |
|---|---|---|---|---|
| Age | 0.013 | 0.054 | −0.0002 to 0.0257 | 1.012 |
| Depressive symptoms (PHQ-9) | −0.047 | 0.006 | −0.0806 to −0.0138 | 0.954 |
| Impulsivity (BIS-11) | 0.035 | 0.049 | 0.0002 to 0.0698 | 1.036 |
| Physical abuse (CTQ-SF) | 0.208 | 0.015 | 0.0404 to 0.3756 | 1.231 |
| Non-significant variables | ||||
| Sex | −0.260 | 0.348 | −0.8015 to 0.2822 | 0.771 |
| Civil status | 0.069 | 0.609 | −0.1960 to 0.3343 | 1.072 |
| Educational level | 0.091 | 0.396 | −0.1190 to 0.3008 | 1.095 |
| Occupation | −0.097 | 0.293 | −0.2791 to 0.0842 | 0.907 |
| Adherence | 0.302 | 0.173 | −0.1326 to 0.7370 | 1.353 |
| Alcohol disorder | −0.332 | 0.309 | −0.9716 to 0.3072 | 0.717 |
| Substance disorder | −0.551 | 0.114 | −1.2346 to 1.1325 | 0.576 |
| GAD | −0.024 | 0.412 | −0.0795 to 0.0326 | 0.977 |
| EuroQol-5D | 0.002 | 0.615 | −0.0071 to 0.0120 | 1.002 |
| Emotional abuse (CTQ-SF) | 0.079 | 0.572 | −0.1965 to 0.3554 | 1.083 |
| Sex abuse (CTQ-SF) | 0.113 | 0.204 | −0.0614 to 0.2875 | 1.120 |
| Emotional negligence (CTQ-SF) | −0.084 | 0.431 | −0.2916 to 0.1244 | 0.920 |
| Physical negligence (CTQ-SF) | −0.078 | 0.673 | −0.4428 to 0.2860 | 0.925 |
| ACSS-FAD | −0.021 | 0.159 | −0.0500 to 0.0082 | 0.979 |
| RFQ-C | 0.188 | 0.236 | −0.1230 to 0.5000 | 1.207 |
| RFQ-U | 0.001 | 0.996 | −0.3961 to 0.3980 | 1.001 |
| Family history of suicide | −0.033 | 0.894 | −0.5149 to 0.4491 | 0.968 |
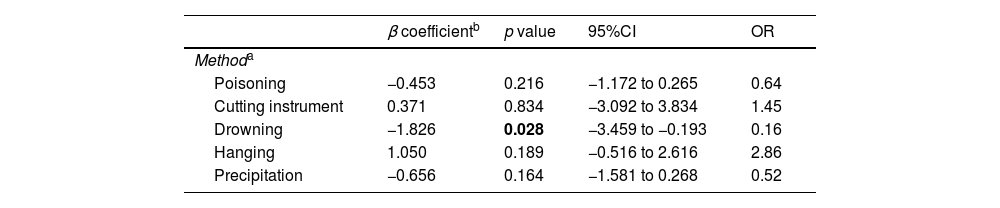
These four variables previously found related to SSA were included as covariates in the ordinal regression model to analyze the relation between the suicide attempt method (predictor) and its lethality. As a result, drowning was found to show significantly a lower risk of a SSA than firearms (OR=0.16). Hanging seemed to have the higher risk of producing SSA (OR=2.86), although there were no statistical differences (Table 5).
Relationship between method and suicide attempt severity.
The aim of this multisite, coordinated, cohort study was to determine the predictors of SSA in a large sample of patients who were admitted a hospital emergency department due to a suicide attempt. The study shows that physical abuse and impulsivity were associated with greater severity of suicide attempt, while depressive symptoms were associated with less severity of suicide attempt.
Our findings show that early traumatic life experiences represent the factor more strongly associated with an SSA. There is a previous study that has found a direct association between early trauma and SSA in cocaine abusers,20 but there is a lack of studies on the relation between early trauma and SSA. Few studies have found that childhood and family adversities are significant SSA risk factors.13,20 Early traumatic experiences can leave permanent epigenetic marks on the brain, and it has been shown that can increase the risk of suicide later in life.35,36 Adverse childhood experiences may have an influence on the stress regulation pathways, leading to alterations in coping style, emotional regulation, stress response and personality characteristics, such as trait impulsivity, with long lasting effects on adulthood.37,38 According to the stress sensitization theory, early stress in life dysregulates stress response systems and lowers the threshold for reactivity and adaptive responses to stress thought life.39 In turn, these poor emotional regulation strategies coupled with early-life adversity and some clinical and personality factors can increase the risk of suicidal behaviour.40–42 Traumatic events are frequent in severe mental disorders, including personality disorders, eating disorders psychosis and major depressive disorders.
Another risk factor associated with suicide attempt severity in our sample was the impulsivity. It is known that impulsivity may play an important role in suicidal behaviour4; however, there are few studies regarding the association between impulsivity and SSA. The degree of preparation and planning of suicidal behaviour is a significant factor in determining the severity of the attempt and it is generally used as an indicator of the impulsiveness-state. In fact, many people die by suicide or engage in highly lethal behaviours due to their state impulsivity, in each circumstance, with no or poor planning. Although impulsiveness does not necessarily explain the severity of the suicide attempt, it does facilitate the ability to attempt a more lethal suicide in the future, especially among those patients who originally made an SSA.4 The inability to control the impulses, coupled with characteristics of aggression and feelings of anger are associated with the suicide attempt severity.4,43–46 According to the model of the acquired capability Component of Joiner's47 Interpersonal-Psychological Theory of Suicide, impulsivity is a risk factor for the capability for suicide that moderates the experience of painful life events. Suicide attempters, particularly severe suicide attempters, experience reduced serotonergic activity that has been associated with impulsivity traits.47 These individuals are less likely to heed warning signs of fear and pain, leading them to fearlessness and pain insensitivity to the actions and ideas involved in severe suicide attempts.48
Our study reveals that in the univariate analyses, the severity of a suicide attempt is associated with older age, consistent with other studies.16,18 Age was part of the final model, but did not reach significance in the regression analyses. Although the mean age of the sample was around the middle age, when we compared the three-suicide attempt severity groups in fact, the patients in the SSA group were older than those in the mild attempt group. Other studies suggests that forms of presentation of suicidal behaviour, specifically, behavioural lethality, vary greatly depending on age. In general, suicide occurs primarily in middle ages of life, however two peaks are observed: adolescence/youth (25% of all completed suicides) and old age. As age advances, the ratio between suicide attempts and completed suicide is lower, which implies that adults make fewer suicide attempts than young, but use more effective methods when trying, which leads to greater lethality and a large part of suicide attempts ends up being consummated. Adults can experience a feeling of personal, work and family failure or a social reproach, which leads despair feelings. If this situation is compounded by the presence of loneliness, a poor social support, chronic disabling diseases or poor prognosis disorders, these people can plan the act, carry it out alone and use fast and effective methods, such as precipitation, hanging, or firearms.49
Another main finding of the study was that depressive symptoms were inversely related with SSA. That is, patients with higher levels of depressive symptoms were more likely to have a milder suicide attempt, suggesting that depression may be a slight protective factor for SSA, although a depressive episode is a frequent diagnose in the three groups. More than 2/3 of the SSA were diagnosed of a Major Depressive Episode, and only 4,6% of patients with a SSA had no psychiatric diagnosis.
Many studies have found that depression and hopelessness may substantially contribute to an increased risk of suicidal ideation, suicide attempts and even death.36,50 In fact, around 10–15% of patients with a major depressive disorder may engage in suicide, and between 60 and 70% of subjects who attempt suicide, suffered a depressive episode.51 Nevertheless, it has been seen that depression can act as a protective factor for suicide attempt,52 possibly due to motor inhibition or treatment. It is also possible that patients that are improving from a depressive episode do not reach the Major Depressive Disorder diagnosis by the MINI but are at high risk of suicide attempt. In a 10-year follow-up study of patients with bipolar disorder, we also found that when patients who improved from depression or had mixed symptoms, showed at increased risk of suicide.53
Other studies comparing SSA with non-SSA, also found that depression was not associated with SSA. In the study conducted by Swahn and Potter,54 the percentage of individuals who experienced severe depression in SSA and non-SSA groups was high, but depressive symptoms were significantly associated with lower lethal suicide attempters. Similarly, in other studies found that depression, mental pain and hopelessness did not predict medical severity of the suicide attempt when SSA and non-attempters were compared.50,55,56 These findings suggest that psychological pain, hopelessness, emotional distress and depression which are linked to suicidal thoughts and suicide attempts are related to a lower medical lethality of the attempt.55 This could be explained because despite the desire to die, inhibition and apathy, typical of depression, act as a protective factor, preventing lethal suicidal behaviour.49 The absence of association between other mental disorders and suicide severity could be related to the small sample size of these groups, as previously large samples have shown higher risk of dying by suicide in these groups.57 With the exception of anxiety disorder group, all other diagnoses (psychosis, eating disorders, bipolar disorder and substance abuse) were numerically more prevalent in the SSA group.
Gender was not associated with severity of suicide attempts. Women usually do more suicide attempts and die less by suicide.58 As severe suicide attempts are related to death by suicide, we could expect a higher number of men in the group of SSA. We found a small and non-significant higher proportion of men in this group. In fact there is a non-significant gradient of presence of men related to SSA, with higher proportion of men in SSA (34.1%), intermediate in moderate suicide attempts (29.6%), and lower frequency in mild suicide attempts (25.2%). Despite these results, the sample includes more women with SSA (65.9%) than men with SSA. In addition, we did not find any differences between severe and non-severe mental disorders in relation to the scale of reflective function.
In conclusion, the results of this study indicate that early physical abuse and impulsivity are predictors of SSA whereas depressive symptoms were associated to lower suicide attempt severity risk. Our findings have important implications to clinical practice. Most studies consider suicide as a complex, multifactorial phenomenon, but a unified approach is often employed, without considering differences between suicide severity levels. Our results suggest that suicidal behaviour is heterogeneous. There are different factors associated to SSA compared to those with mild suicide attempter patients. Therefore, it is important consider these risk factors (impulsivity, early trauma and depression) to assess the risk of a future severe suicide attempt. Moreover, the results are generalizable, because they were obtained in a multicentre study that included a large sample of patients with suicide attempt recruited at ten sites distributed across Spain. Our findings support the importance of developing a more accurate diagnosis and risk assessment to identify individuals at risk for SSA. Knowing the differences between the risk factors associated with suicide severity levels can open avenues for the treatment and management of suicide attempters. Likewise, identify the risk factors of suicide attempt severity will allow us to develop strategies to prevent suicide. The seriousness of this phenomenon urges the need of promote a national suicide prevention plan that includes guidance criteria for management of vulnerable and affected people.
This study has some limitations. Although the classification of levels of SSA is based on concrete criteria and measures (Columbia Suicide Rating Scale and DSM-V criteria), different definitions of severity may result in different findings. Further studies should clarify and refine the wide variety of definitions found in the literature. Likewise, this is a cross-sectional study; future studies could conduct longitudinal studies to analyze suicidal behaviour in long-term follow-up. We did not include any dimensional scale of depressive symptoms. Besides, the study lacks other confounding variables that may have been considered: lifestyle habits, inflammation parameters, BMI index or other psychological variables such as sexual orientation, coping styles, cognitive function and attachment.
Ethics approvalThe study was approved by the Clinical Research Ethics Committees of all the participating centres.
Patient consentInformed consent was obtained from all subjects involved in the study.
Clinical trial registrationThis study was registered in ClinicalTrials.gov (Identifier NCT04343703).
FundingThis study was funded by the Spanish Ministry of Economy and Competitiveness through the Carlos III Health Institute (ISCIII) and the European Regional Development Fund (ERDF): Complutense University of Madrid (PI20/00259), Mar Institute of Medical Research (IMIM), Parc de Salut Mar (PI19/00236), University of Oviedo (PI19/01027), Hospital Clínico San Carlos (PI19/01256), Araba University Hospital (PI19/00569), La Paz Institute for Health Research (IdiPAZ) (PI19/00941), Hospital Universitari Parc Taulí (PI19/01484), Hospital Clínic of Barcelona (PI19/000954), Hospital Virgen del Rocío (PI19/00685).
Dr. Bobes has received partial support from the Government of the Principality of AsturiasPCTI-2021-2023 IDI/2021/111, the Fundación para la Investigación e Innovación Biosanitaria del Principado de Asturias (FINBA), and Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM), Instituto de Salud Carlos III, and Ministerio de Ciencia e Innovación. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Dr. González-Pinto thanks the support of the Spanish Ministry of Economy and Competitiveness through the Carlos III Health Institute (ISCIII) and the European Regional Development Fund (ERDF) (PI18/01055, PI21/00713); the Foundation for Health Innovation and Research (BIOEF); the Networking Centre for Biomedical Research in Mental Health (CIBERSAM), the Basque Government [grant number 2017111104] and the University of the Basque Country [grant number 321218ELCY]. The psychiatric research department in Araba University Hospital is supported by the Stanley Research Foundation [grant number 03-RC-003].
Dr. Grande thanks the support of the Spanish Ministry of Science and Innovation (MCIN) (PI19/00954) integrated into the Plan Nacional de I+D+I and cofinanced by the ISCIII-Subdirección General de Evaluación y Fondos Europeos de la Unión Europea (FEDER, FSE, Next Generation EU/Plan de Recuperación Transformación y Resiliencia_PRTR); the Instituto de Salud Carlos III; the Networking Centre for Biomedical Research in Mental Health (CIBERSAM); and the Secretaria d’Universitats i Recerca del Departament d’Economia i Coneixement (2017 SGR 1365), CERCA Programme/Generalitat de Catalunya as well as the Fundació Clínic per la Recerca Biomèdica (Pons Bartran 2022-FRCB_PB1_2022).
Conflict of interestDr. Bobes has received research grants and served as a consultant, advisor, or speaker within the last 5 years for AB-Biotics, Acadia Pharmaceuticals, Alkermes, Allergan, Ambrosetti-Angelini, Biogen, Casen Recordati, D&A Pharma, Exeltis, Gilead, Indivior, GW Pharmaceuticals, Janssen-Cilag, Jazz Pharmaceuticals, Lundbeck, Mundipharma, Newron, Otsuka, Pfizer, Roche, Sage Therapeutics, Servier, Schwabe Farma Ibérica, Shire, and Takeda and has received research funding from the Spanish Ministry of Economy and Competiveness – Centro de Investigación Biomedica en Red area de Salud Mental (CIBERSAM) and Instituto de Salud Carlos III– and the Spanish Ministry of Health.
Dr. Gonzalez-Pinto has received grants and served as consultant, advisor or CME speaker for the following entities: Almirall, AstraZeneca, Bristol-Myers Squibb, Cephalon, Eli Lilly, Glaxo-Smith-Kline, Janssen-Cilag, Ferrer, Johnson & Johnson, Lundbeck, Merck, Otsuka, Pfizer, Sanofi-Aventis, Servier, Shering-Plough, Solvay, the Spanish Ministry of Science and Innovation (CIBERSAM), the Ministry of Science (Carlos III Institute), the Basque Government, the Stanley Medical Research Institute (03-RC-003), and Wyeth.
Dr. Grande has received grants and served as consultant, advisor or CME speaker for the following identities: ADAMED, Angelini, Casen Recordati, Ferrer, Janssen Cilag, and Lundbeck, Lundbeck-Otsuka, Luye, SEI Healthcare outside the submitted work.
Dr. Seijo-Zazo has received honoraria/grants and served as consultant, advisor or speaker within de last 5 years for: Adamed, Angelini, Alter, Esteve, Janssen-Cilag, Lundbeck, Otsuka, Pfizer, Rubió, Servier, Shire, Exeltis.
The rest of the authors of this manuscript have no conflict of interest to declare.
We would like to thank the following institutions: the Basque Foundation for Health Innovation and Research (BIOEF), the Centre for Biomedical Research in the Mental Health Network (CIBERSAM), the University of the Basque Country, and Bioaraba Research Institute.
Natalia Angaritaaa,ak, Wala Ayad-Ahmedac,ad, Jose Luis Ayuso-Mateosaa,ad, Mª Teresa Bobes-Bascaránaa,af, Lorenzo Braccoao,ap, Manuel Canal-Riveroaa,ai, Irene Canosa-Garcíaaa,ak, Myriam Caveroal, Laura Comendadorak,ap, Javier Curto-Ramosag, Jennifer Fernández-Fernándezaf, Melisa V Fernandez-Iturriaj, Daniel Garcíaag, Ainoa García-Fernándezaf, Elena Garcia-Ligeroaj, Adriana Garcia-Ramosad, Joaquín Gilal, Luis Jimenez-Treviñoaa,af, Guillermo Juarezag, Itziar Leal-Leturiaad, Saioa López-Zurbanoab,ae, Lorea Mar-Barrutiaab, Maria T Muñozah, Marta Navasac, Beatriz Orgazag, Diego J Palaoaa,ah,ap, Ivan Pérez-Diezad, Joaquim Puntiah, Pablo Reguera-Pozueloaj, Julia Rideraj, Pilar A Sáizaa,af, Lola Saizac, Alba Tollaa,ak, Nuria Turac, Mireia Vazquezal, M Velascoag, Eduard Vietaaa,al,am,an, Iñaki Zorrillaaa,ab,ae
aa Centre for Biomedical Research in the Mental Health Network (CIBERSAM), Madrid, Spain
ab Department of Psychiatry, Araba University Hospital, Bioaraba Research Institute, Vitoria, Spain
ac Hospital Clínico San Carlos, Madrid, Spain
ad Complutense University of Madrid, Madrid, Spain
ae Department of Neurosciences, University of the Basque Country, Leioa, Spain
af Department of Psychiatry, University of Oviedo, Oviedo, Spain
ag Department of Psychiatry, Clinical Psychology and Mental Health, La Paz University Hospital, Madrid, Spain
ah Mental Health Service. Hospital Universitari Parc Taulí. Unitat Mixta de Neurociència Traslacional I3PT-INc-UAB, Barcelona, Spain
ai Department of Clinical and Health Psychology, Faculty of Psychology, Universitat Autònoma of Barcelona, Cerdanyola del Vallès, Spain
aj Hospital Virgen del Rocío, Instituto de Biomedicina de Sevilla (IBIS), Sevilla, Spain
ak Mar Institute of Medical Research (IMIM), Parc de Salut Mar, Barcelona, Spain
al Bipolar and Depressive Disorders Unit, Hospital Clinic of Barcelona, Institut d’Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Barcelona, Spain
am Institute of Neurosciences (UBNeuro) P. de la Vall d’Hebron, Barcelona, Spain
an Departament de Medicina, Facultat de Medicina i Ciències de la Salut, Universitat de Barcelona (UB), Barcelona, Spain
ao Department of Neurosciences and Mental Health, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, 20122 Milan, Italy
ap Department of Psychiatry and Forensic Medicine, Faculty of Medicine, Universitat Autònoma de Barcelona. 08193 Cerdanyola del Vallès, Spain