Altered intestinal permeability and low-grade chronic inflammation disrupt the integrity of the blood–brain barrier (microbiota–gut–brain axis), probably playing a role in the pathophysiology of schizophrenia-spectrum disorders. However, studies assessing the microbiota–gut–brain axis are inconsistent. This article describes the rationale, objectives, protocol, and presents descriptive results for a new project.
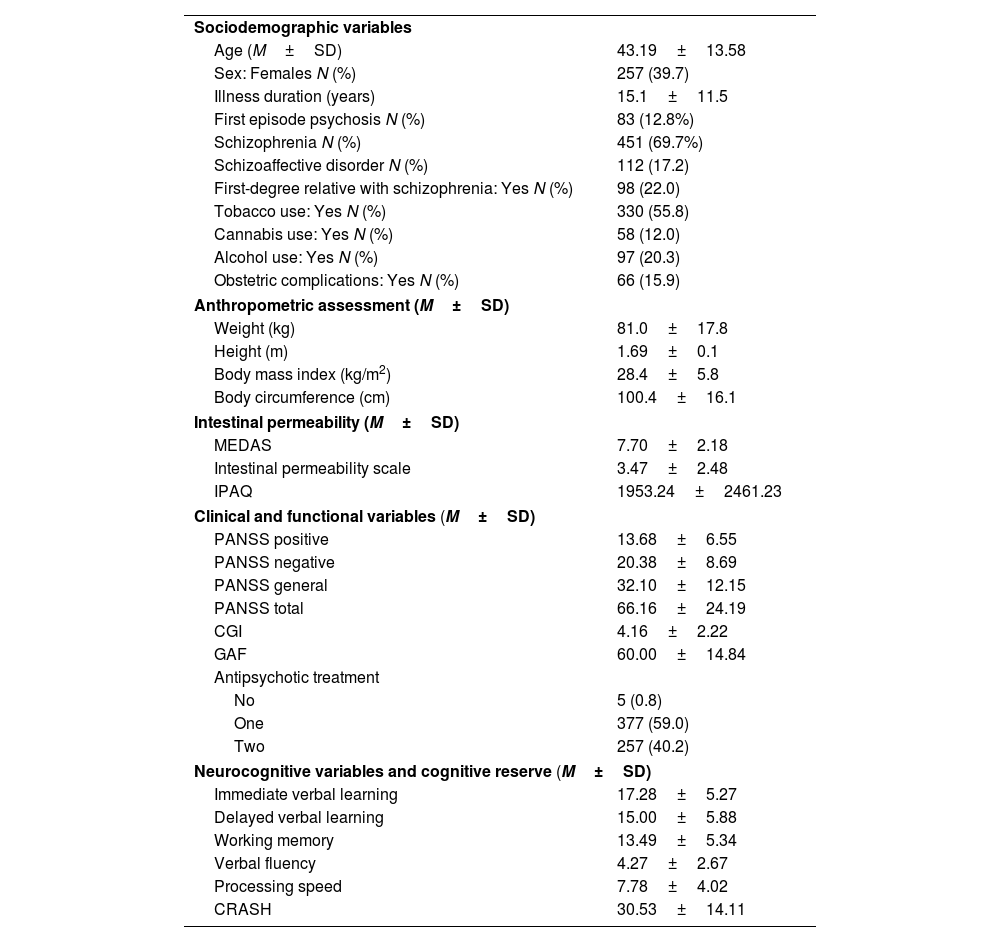
MethodsThe sample of this study came from an observational, cross-sectional and multisite study including four centers in Spain (PI17/00246) recruiting adult patients with DSM-5 schizophrenia-spectrum disorders at any stage of the disease. The aims of the project are to assess the interrelation between intestinal permeability and low-grade chronic inflammation in schizophrenia-spectrum disorders and the role of peripheral biomarkers, diet, exercise, metabolic syndrome, disease severity and functioning as well as cognition. Assessments included the following variables: (1) anthropometric, (2) intestinal permeability, diet, and physical exercise, (3) clinical and functional, (4) neuropsychological and cognitive reserve, and (5) peripheral biomarkers from blood.
ResultsA total of 646 patients were enrolled (257, 39.7% female). Mean age was 43.2±13.6 years, illness duration 15.1±11.5 years. 55.8% consumed tobacco. Positive PANSS score was 13.68±6.55, and 20.38±8.69 in the negative symptoms. CGI was 4.16±2.22 and GAF was 60.00±14.84.
ConclusionThe results obtained by this project are expected to contribute toward the understanding of the physiopathology of schizophrenia-spectrum disorders. This will likely aid to personalize treatments in real-world clinical practice, potentially including variables related to intestinal permeability and inflammation.
Artículo
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora