Losing a patient by suicide may lead to psychological distress and mid/long-term personal and professional consequences for psychiatrists, becoming second victims.
Material and methodsThe validated Spanish version of the Second Victim Experience and Support Tool (SVEST-E) questionnaire and a 30-item questionnaire created ad-hoc was administered online to psychiatrists from all over Spain to evaluate how patient suicide affects mental health professionals.
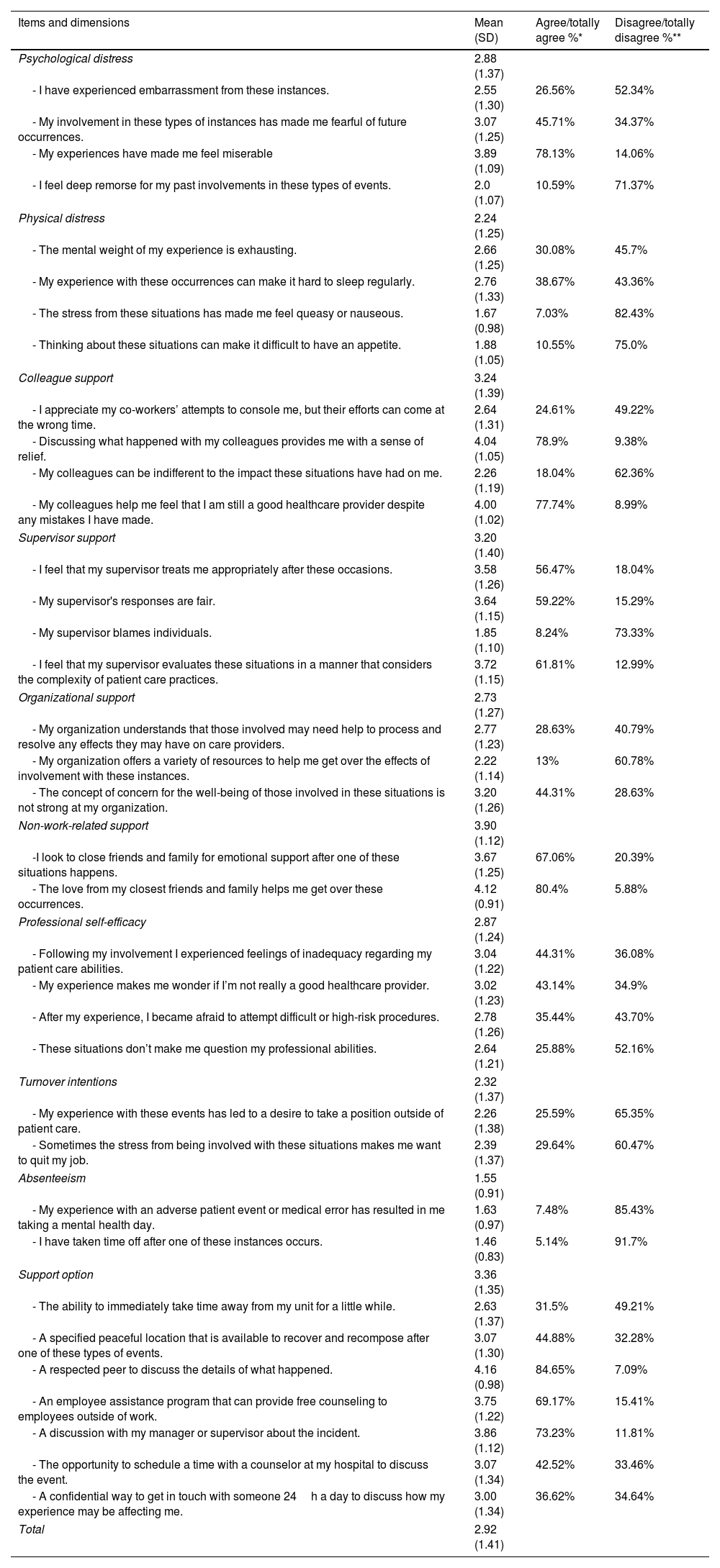
ResultsTwo hundred ninety-nine psychiatrists participated in the survey, and 256 completed the SVEST-E questionnaire. The results of the SVEST-E questionnaire revealed a negative impact of suicide on emotional and physical domains, although this seemed not to lead to work absenteeism. Most respondents desired peer support from a respected colleague and considered institutional support, although desirable, lacking. Almost 70% of surveyed stated that an employee assistance program providing free counseling to employees outside of work would be desirable. The ad-hoc questionnaire showed that up to 88% of respondents considered some suicides unavoidable, and 76% considered the suicide unexpected. Almost 60% of respondents reported no changes in the approach of patients with suicidal ideation/behavior, after losing a patient. However, up to 76% reported performing more detailed clinical evaluations and notes in the medical record. Up to 13% of respondents considered leaving or changing their job or advancing retirement after losing a patient by suicide.
ConclusionsAfter a patient's suicide, psychiatrists often suffer the feelings of second victim, impacting personal and professional areas. The study results indicate the need for postvention strategies to mitigate the negative impact of patient suicide.
Artículo
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora