Recent advances in flexible ureteroscopy, as well as the development of various accessories and the implementation of Holmium laser as a fragmentation mechanism, consisting of flexible retrograde laser nephrolithotomy (FRLN), is an attractive alternative for the management of large lithiasic masses. The analysis of the evidence available to date is essential to establish the benefits and limitations compared to other therapies, such as percutaneous nephrolithotomy.
Materials and methodsA systematic search was performed in MEDLINE and SCIENCEDIRECT data bases. The search was limited by language to articles published in English and Spanish, and limited in time to articles published in the last 10 years. A total of 30 articles of interest to the topic and a case report on a large lithiasic mass handled with FRLN are included.
DiscussionPercutaneous nephrolithotomy is considered the gold standard for the management of renal stones larger than 2cm, with stone free rates of 76–95% with 1.9 procedures. However, complication rates have been reported between 8 and 45%, and decreased GFR between 9 and 34% was recorded in the post-operative period. On the other hand FRLN provides an stone free rates of 86–95% in about 1.6 procedures, and complication rates ranging from 10 to 20%.
ConclusionsThe FRLN has become an effective alternative for the management of large lithiasic masses, with stone free rates similar to those obtained with percutaneous nephrolithotomy, but with fewer complications. Its usefulness is most evident in special cases, such as large stones associated with significant comorbidity, obesity, failure renal, spinal malformations, or a single kidney.
Los recientes avances en la ureteroscopia flexible, como el desarrollo de diversos accesorios y la aparición del láser holmio como mecanismo de fragmentación, hacen de la nefrolitotomía retrógrada flexible láser (NRFL) una alternativa atractiva para el manejo de grandes masas litiásicas. El análisis de la evidencia disponible hasta el momento resulta fundamental para establecer sus beneficios y limitaciones frente a terapias establecidas como la nefrolitotomía percutánea.
Materiales y métodosSe realizó una búsqueda sistemática en bases de datos MEDLINE y SCIENCEDIRECT. La búsqueda fue limitada por idioma para artículos publicados en inglés y español, y limitada en tiempo para artículos publicados en los últimos 10 años. Se incluyen 30 artículos de interés para el tema y el reporte de caso de gran masa litiásica manejada con NRFL.
DiscusiónLa nefrolitotomía percutánea es considerada el patrón de oro para el manejo de cálculos renales mayores de 2cm con tasas libres de cálculo del 76–95% con 1,9 procedimientos, sin embargo, las tasas de complicación se han descrito entre el 8–45%, y la disminución de la TFG en el periodo postoperatorio se ha registrado entre 9–34%. Por otro lado la NRFL ofrece tasas libres de cálculo del 86–95% con 1,6 procedimientos, y tasas de complicación que oscilan entre el 10–20%.
ConclusionesLa NRFL se convierte en una alternativa eficaz para el manejo de grandes masas litiásicas con tasas libres de cálculo similares a las obtenidas con nefrolitotomía percutánea aunque con menor índice de complicaciones; su utilidad es más evidente en casos especiales tales como cálculos grandes asociados a comorbilidad importante, obesidad, falla renal, malformaciones óseas, espinales o riñón único.
The latest advances in retrograde flexible laser nephrolithotomy (RFLNL) have led to its increasing use. The different benefits of the technique, as well as the decrease in the diameters of the instruments, its flexibility and the development of accessories, such as ureteral access sheaths, nitinol baskets, water pumps, and holmium laser fibres for stone fragmentation, has made this procedure an alternative for the management of calculi greater than 2cm. Without prejudice to the role of percutaneous nephrolithotomy (PCNL), it is important to highlight the benefits and limitations of RFLNL for the management of large volume stone masses.
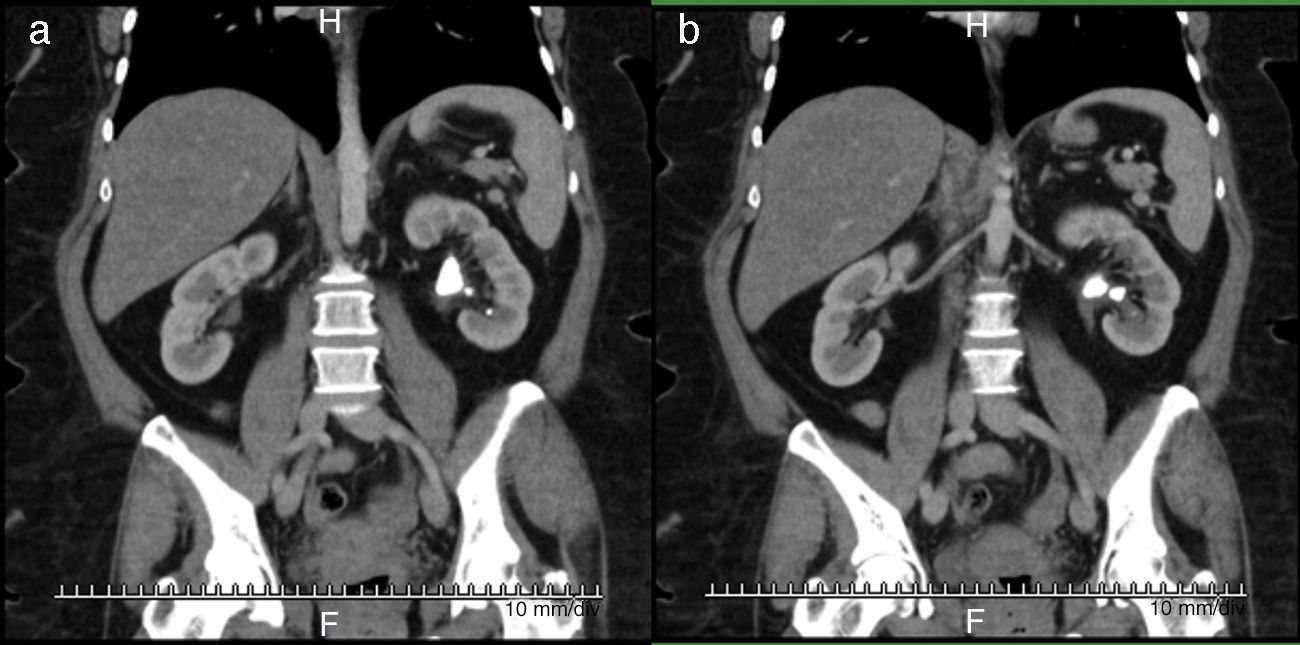
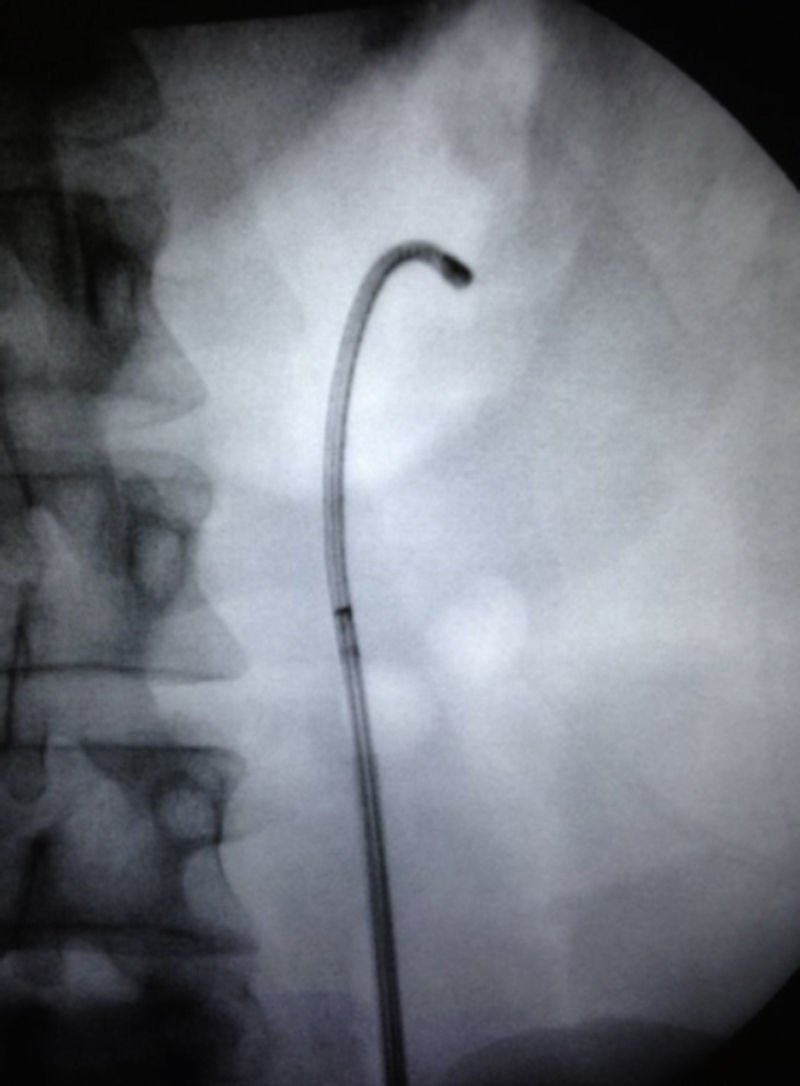
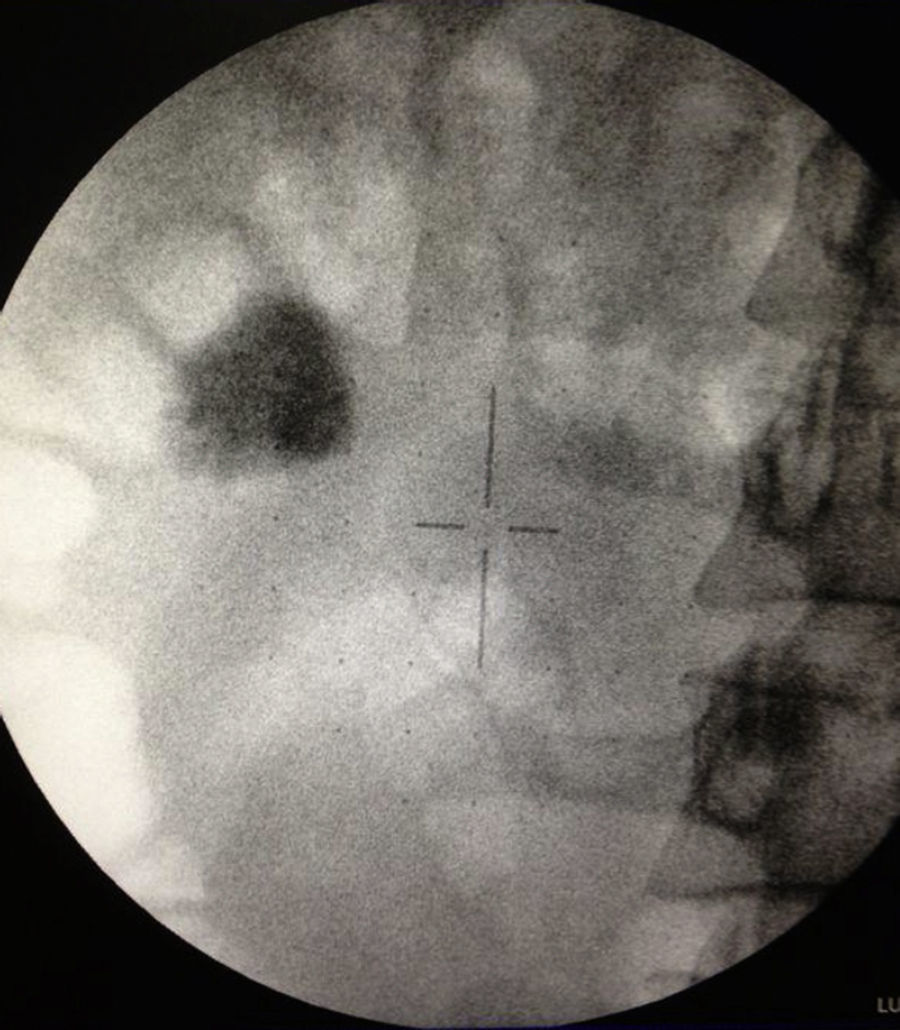
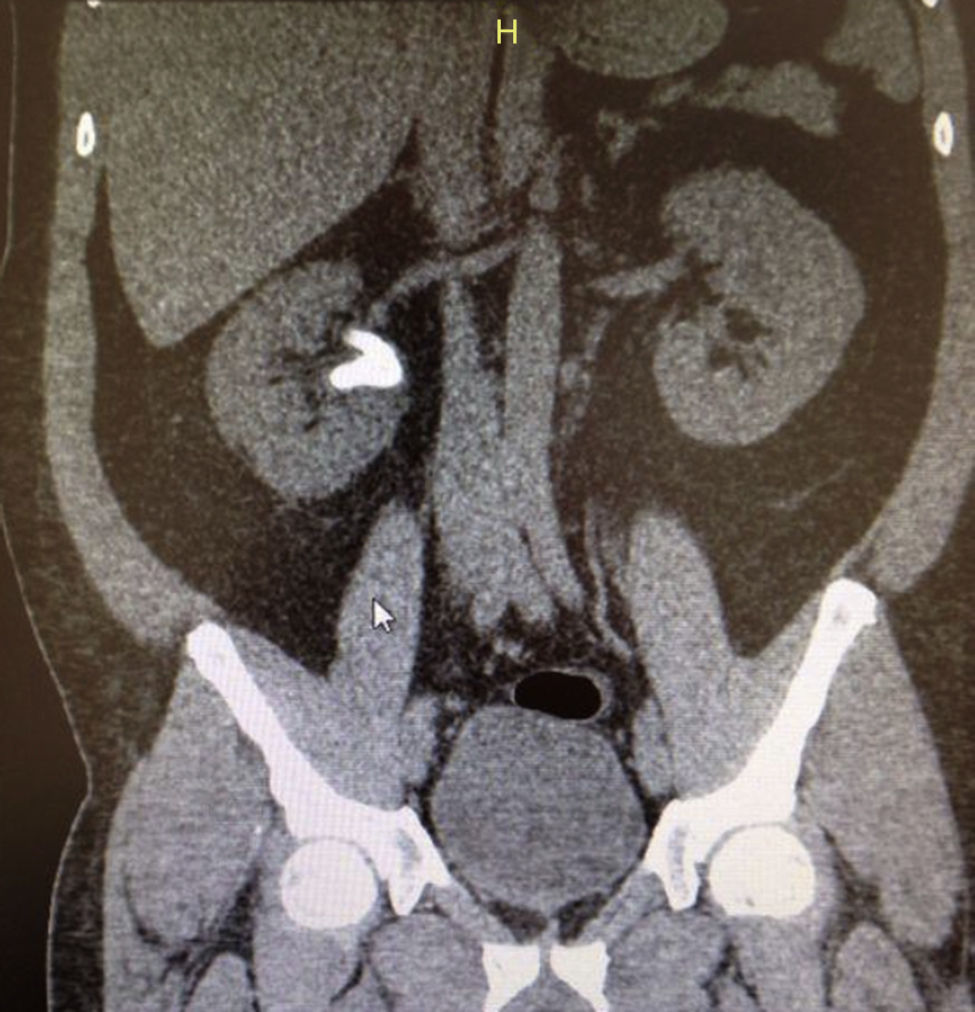
Clinical case 1A 52 year-old female patient with a body mass index of >35 and incomplete staghorn calculi that occupied the upper, middle and pelvic calyx in the left kidney, (Figs. 1a and b, and 2a and b), was managed with RFLNL (Fig. 3a and b) obtaining complete clearance of the calculus with fragments less than 2mm in a single procedure (Fig. 4), and with no complications observed.
A 58 year-old male patient with a history of degenerative discopathy and lumbar spine instrumentation, hypothyroidism, and a previous history of lithiasis and who required a uretero-lithotomy. The images showed evidence of an incomplete staghorn calculi that occupied the upper and pelvic calyx of the right kidney (Figs. 5 and 6), that was managed with RFLNL, obtaining complete clearance of the calculus in a single surgical procedure (Fig. 7).
A 32 year-old female patient with a history of a right percutaneous nephrolithotomy due a complete calciform calculus. In the follow-up imaging tests, residual lithiasis was observed in the renal pelvis and lower calyx, with a total calculus mass of approximately 2cm (Fig. 8). An RFLNL was performed, achieving completing clearing of the calculus in only one surgical procedure (Fig. 9).
A systematic search was performed the MEDLINE and SCIENCEDIRECT data bases, using the medical subject headings (MeSh) terms: “2cm”, “holmium laser”, “retrograde intrarenal surgery”, “stones”, “flexible, retrograde nephrolithotomy”, and “percutaneous nephrolithotomy”. The search was limited to articles published in English and Spanish, and limited in time to articles published in the last 10 years.
A total of 30 articles on the topic of interest were included, finding only a meta-analysis and uncontrolled retrospective studies that made reference to RFLNL in the management of large stone masses. No randomised prospective studies of interest to the case were identified.
DiscussionIn the management of stone-forming disease, open surgery for renal calculi was documented in ancient Greek and Roman civilisations in the years 1500–1600. It was popularised by Ingalls in the USA from 1872, and its use was seen to fall from 1980 with the introduction of the introduction of extracorporeal lithotripsy (ECL), is becoming a lost art in the era of minimally invasive surgery.1 Its use is now limited to second or third line treatments due to its negative impact on kidney function in 13.7% of cases, major complications, and longer hospital stays of between 6 and 7 days, with stone free rates (SFR) of 76.2%.2,3
Percutaneous nephrolithotomy (PCNL) is considered the reference standard for the management of kidney stone disease with a size greater than 2cm, and it has almost completely replaced open surgery for the treatment of large-sized or complex stones. The European Guidelines of 2014 recommend PCNL for the treatment of all stones greater than or equal to 2cm and calculi of the lower pole greater than or equal to 1.5cm, in which ECL has limited use.4
The first description of PCNL was published by Fernstrom and Johansson in 1970, and for staghorn calculi, the first report was by Clayman in 1983. It was initially described in the prone decubitus position, and its aim was to ensure complete removal of calculi with minimal morbidity.5 The controversies as regards the surgical technique of PCNL are presented in 5 special situations: the position, percutaneous access, dilation of the tract, post-operative drainage, and the alteration in kidney function.
There have been significant advances in the positions of PCNL since the first description. The different positions described include the Valdivia position, the modified Valdivia, flank position, and the fully supine position. The incidence of complications decreases with obvious advantages in a supine position, and is more suitable for obese patients and those respiratory or cardiac compromise.5
Percutaneous access is more commonly performed using fluoroscopic guidance. Inherent to this method is the exposure to ionising radiation for the surgeon and the rest of the surgical team. For this reason, several studies have been conducted with ultrasound-guided access, arriving at the conclusion that it has satisfactory results with few complication, and less exposure to radiation.6 Kumari quantified the radiation received by the surgeon, and found that in a surgery with a mean fluoroscope time of 6min radiation exposure in the finger of the surgeon reached a level of 0.28mSv, and a level of 0.56mSv in the trunk. The Radiation Protection Agency recommends a maximum dose of exposure in one years of 50,000mSv. The annual doses, according to this study, are admissible but very variable depending on the complexity and duration of each procedure. For this reason, several studies with ultrasound-guided access have been conducted, and all reached the conclusion that it has satisfactory results with few complications for the patient and less radiation exposure for the surgeon.6
For the tract dilation, a variety of methods with dilators have historically been used, such as Alken (metallic), Amplatz (plastic), and dilation with a balloon. Although there is no general consensus in the literature as regards the superior safety and efficacy with balloon dilation over dilation with metal or plastic devices, the CROES (Clinical Research Office of the Endourological Society) study compared 5537 dilations (2277 with balloon and 3260 Telescopic/serial dilations), and demonstrated higher rates of bleeding and transfusion needs in the group with balloon dilation.6 More recently, the Miniperc technique has emerged as a percutaneous procedure with a tract size of <18Fr, compared to 26Fr for the standard PCNL. The indications for a Miniperc and ECL overlap it and is commonly used for the treatment of low volume calculi.5 The prospective trials that compare operation times, SFR, and complications, report slightly lower post-operative pain rates for Miniperc and a significantly shorter hospital stay (3.8 vs. 6.9 days) when compared to the group with PCNL.6
The shunt at the end of the procedure traditionally forms part of the PCNL surgical technique. Even so, Desai Bellman described the “tubeless” technique, and determined that there were few complications, improving the recovery time, post-operative pain, and hospital stay. The shunt was reserved for cases with more than two accesses, significant intra-operative bleeding, or the need for a second exploration. Yuan et al. report the same conclusions in a meta-analysis of 14 randomised controlled studies that compared the use of small calibre catheters and the technique without post-operative nephrostomy. On the other hand, in the United Kingdom register, the procedures without post-operative nephrostomy or shunt did not have higher rates of complications, but they did have a shorter hospital stay (3 days vs. 1.5 days; p<.0001.4 The 2014 European guides recommend that in non-complicated cases PCNL, without nephrostomy and without a ureteral catheter, it provides an alternative insurance.4
Many studies have been conducted to evaluate the impact of PCNL on renal function. Teichman et al. reported worsening of renal function in 28% of 177 patients with a follow-up at 7 years. Nahas et al. report no compromise in renal function in 91.5% of patients. The series by Akman et al. reported a stable kidney function in 66.8% of the patients in their series, and even an improvement in 12.8%. This is defined by changes in the glomerular filtration rate (GFR) in the immediate post-operative period (the most important period associated with kidney function in the long-term).7
It has been demonstrated in the literature that the SFR in PCNL for the treatment of staghorn calculi is 78% vs. 71% for open surgery, 66% for PCNL combined with ECL, and 54% with ECL only.6 The number of procedures that were required to achieve suitable success rates with PCNL was 1.9, 3.6 in combination with ECL, and 1.4 procedures in open surgery.6 El-Nahas et al., in 1466 cases of patients subjected to PCNL for staghorn calculi, reported SFR of 56.9%.8
Complications during or after PCNL can be present up to an overall rate of 83%, including urinary extravasion in 7.2%, transfusion in 11.2–17.5%, and fever in 21–32.1%. Among the major complications are, septicaemia (0.3–4.7%), bowel injury (0.2–0.8%), or pleural injuries (0.0–3.1%). A recent review of complications after PCNL using the Clavien system showed a normal course, without complications, in 76.7% of patients.4 The complication rates in PCNL reported by the American Urology Association (AUA) for staghorn calculi are from 7% to 27%, with transfusion rates up to 18%.8 The CROES retrospective study reported that obesity is associated with longer surgical time, a lower SFR, and a higher re-intervention rate.9
On the other hand, the first laparoscopic treatment for lithiasis was performed by Wickham in 1979 using retroperitoneal access, with its use increasing up to 1993 as a less invasive option for selected cases.4,10 SFR up to 100% were are reported, and it could replace open surgery in the majority of situations, with benefits, such as less post-operative pain, shorter hospital stay, and improved cosmetic results.1,4 The indications in the 2014 European guides for laparoscopy of renal calculi include a complex calculi load, treatment failure with ECL and/or endourological procedures, anatomical abnormalities, such as concomitant narrowing of the pyeloureteral junction, and morbid obesity.
Desai et al., in a study of 35 patients reported surgical times of 75 and 102min with transperitoneal and retroperitoneal access, respectively. There were no conversions or need for transfusion. The most common complication was urine leak (0–20%), followed by narrowing (1.4–5.2%).10 Training, technology, and costs limit the use of this technique that will continue to be an alternative option for the modern surgical approach to urolithiasis.11
The advances in the instruments for endoscopic procedures in the last twenty years or so, have led to an increase in their use in patients with large-sized calculi. The flexibility and the smaller diameters of the instruments, as well as the development of new accessories and holmium laser technology, have meant that flexible ureteroscopy and laser lithotripsy have become a valid alternative for these patients.12 The development of ureteral sheaths makes it easier for the instrument to pass through the ureteral lumen, as well as the removal of stone fragments. These have additional benefits due to the protection of the ureteral mucosa during the procedure after the repeated insertion and removal of the instrument, and decrease in intra-renal pressures during prolonged procedures and maintaining continuous drainage.12
For the first time, in 1983, Huffman et al. described the use of flexible ureteroscopy for the management of pyelic stones. Grasso et al. described the use of flexible ureteroscopy in large stone masses in patients who, due to their comorbidity, were not candidates for PCNL, achieving success rates of between 93% and 100% in ureteral calculi.13–15
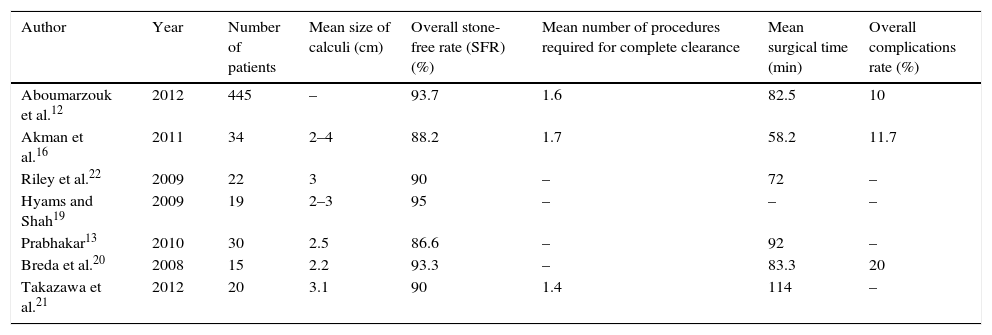
There have been very few prospective, randomised and controlled studies in this field. Up to 2012, the meta-analyses performed only included retrospective studies to evaluate RFLNL compared to PCNL (Table 1).
RFLNL data for calculi greater than 2cm, stone-free rate, number of procedures required, surgical time, and complications recorded for each series.
| Author | Year | Number of patients | Mean size of calculi (cm) | Overall stone-free rate (SFR) (%) | Mean number of procedures required for complete clearance | Mean surgical time (min) | Overall complications rate (%) |
|---|---|---|---|---|---|---|---|
| Aboumarzouk et al.12 | 2012 | 445 | – | 93.7 | 1.6 | 82.5 | 10 |
| Akman et al.16 | 2011 | 34 | 2–4 | 88.2 | 1.7 | 58.2 | 11.7 |
| Riley et al.22 | 2009 | 22 | 3 | 90 | – | 72 | – |
| Hyams and Shah19 | 2009 | 19 | 2–3 | 95 | – | – | – |
| Prabhakar13 | 2010 | 30 | 2.5 | 86.6 | – | 92 | – |
| Breda et al.20 | 2008 | 15 | 2.2 | 93.3 | – | 83.3 | 20 |
| Takazawa et al.21 | 2012 | 20 | 3.1 | 90 | 1.4 | 114 | – |
Akman et al.16 carried out a comparative retrospective study on 68 patients with calculi between 2cm and 4cm, 34 of them treated with RFLNL, and 34 with PCNL, finding operation times of 58.2min (30–85min) and 38.7min (14–60) min (p<.001) for RFLNL and PCNL, respectively. The overall SFR was 88.2% in RFLNL and 91% in PCNL, with no significant difference. As regards complications, they were higher for PCNL (5 patients), but not statistically significant compared with RFLNL (4 patients). However, the length of hospital stay was statistically significant, being 61h (24–192) for PCNL and 30h (18–192) for RFLNL (p<.001).16
There is wide variation as regards how SFR is defined, and there are large differences in the type of images that are used for its definition.17 Thomas et al. considered residual fragments of <4mm in order to constitute a “stone free” result. The most rigorous definition generally includes absence of fragments or that they are <2mm.18 Hyams and Shah19 reported an SFR (defined as fragments of <4mm) of 95%, with no significant differences compared to PCNL, for the previously mentioned 100% success rate. Similarly, Prabhakar13 found an SFR of 86.6% for RFLNL with the first procedure and 100% with the second procedure (13.3% required a second procedure).13 Breda et al. reported an SFR of 93.3%, in which 26.6% required a second procedure in order to achieve complete clearance.20 Likewise, Takazawa et al.,21 reported an SFR of 90% in a group of 20 patients.
As regards calculus size, Riley et al.16,22 demonstrated a 90% success rate for calculi with a mean size of 3cm, with a mean surgical time of 72min. Specifically, an SFR of 91% for calculi between 3cm and 3.5cm with 1.9 procedures; 80% for calculi between 3.5cm and 4cm with 1.8 procedures, and 50% with 2 procedures for calculi >4cm.16 Takazawa et al.21 mention an SFR of 100% for calculi <4cm, and 67% for those >4cm. As regards the location of the calculi, the SFR has been calculated as 91%, 96.5%, 79%, and 84% in the upper pole, middle pole, lower pole, and renal pelvis, respectively.23
Aboumarzouk et al.12 included 445 patients in a meta-analysis that were in retrospective cohorts without randomisation, finding among the results, clearance rates of 93.7% (77–97.5%) for calculi of 2.5cm, with a mean of 1.6 procedures per patient, and a surgical time of 82.5min (28–215min). In the analysis by sub-groups, the clearance rate for calculi between 2cm and 3cm was better than for calculi >3cm (95.7% vs. 84.6%; p=.001; OR: 4.03; 95% CI: 1.38–11.72). In the 2–3cm group, the number of procedures was lower (1.46±0.2 vs. 1.85±0.02; p<.0001; 95% CI: −0.42 to 0.36).
The overall complications rate was 10% in this same study, with minor and major complications being recorded in 4.8% (19 patients) and 5.3% (21 patients), respectively. Among the minor complications was self-limited haematuria in 6 patients, pain in 3 patients, urinary infection treated with oral antibiotics as an outpatient in 5 patients, and minor intra-operative bleeding and urine retention in one patient. Among the major complications were, subcapsular haematoma in 4 patients, obstructive pyelonephritis in 4 patients, one of whom required management in an intensive care unit.12
Furthermore, for the year 2011, the cost of PCNL was estimated as $1903 (€1600), while the cost for RFLNL was estimated as $1025 (€1400), being significantly higher for PCNL, mainly due to a more prolonged hospital stay and management of the complications.24
Akman et al.16 also found higher costs with PCNL compared to RFLNL ($19,845 vs. $6675, p<.0001), with more second procedures being required in patients subjected to PCNL than those managed with RFLNL, with 1.6 vs. 1.1 procedures required for each case.
RFLNL is proposed as an alternative treatment for calculi masses >2cm, however, different points of controversy arise, among which include the lack of higher level evidence since the results are mainly based on retrospective studies, the variation in the concept of SFR, since some studies interpret it as fragments <1mm, others a fragments <2mm, and even others that include fragments <4mm. However, residual stones of >4mm could lead to more symptomatic episodes that could require intervention in the future, while fragments of 2mm could be observed as being safe. The time and types of imaging for their follow-up is not well-defined either.
ConclusionAlthough PCNL continues to be the reference standard for the management of kidney stones >2cm, RFLNL is becoming a valid alternative for these patients, showing success rates similar to PCNL, but lower morbidity, since complications with PCNL have been described in 8–45% of cases.16 In special cases, such as large calculi associated with significant comorbidity, obesity, kidney failure, bone and spine malformations, or a single kidney, RFLNL is an important therapeutic tool, with advantages as regards conservation of patient kidney function, and lower radiation exposure rates for the surgeon in comparison with PCNL.23,25
Conflict of interestsThe authors declare that they have no conflicts of interests.