Vacunas COVID-19: desarrollo y práctica - COVID-19 vaccines: development and practice
Más datosHesitancy towards COVID-19 vaccination and its rejection remains a major public health concern worldwide, especially in the Middle East and North African countries. The current study aimed to assess the intentions to get COVID-19 vaccines and its determinants among the general public in Algeria.
MethodsA self-administered online survey was distributed during August-September 2021 using a convenience-based sampling approach. Data were collected anonymously and analyzed using IBM SPSS v22.0 software.
ResultsThe study sample comprised a total of 656 participants, with 51.1% being in favor of COVID-19 vaccines while 18.5% and 30.5% were against or hesitant respectively. Only 38.6% among the study participants got vaccinated. Factors associated with higher odds of acceptance were: male sex, healthcare profession, the belief in natural origin of the pandemic and previous COVID-19 infection in family. The most common cited reasons for COVID-19 vaccine acceptance were the belief that vaccination is the only way to fight COVID-19 and the fear of getting infected by the virus; while the most common reasons of rejection were lack of trust in proper vaccine testing and fear of side effects.
ConclusionThe overall level of COVID-19 vaccine acceptance in this study was below the levels required to achieve population immunity. Besides certain socio-demographic characteristics, the determinants of COVID-19 vaccine rejection included the embrace of conspiratorial ideas regarding the virus and its vaccination. This should be considered in implementation of interventional measures aiming to promote COVID-19 vaccination in the country.
Las dudas sobre la vacuna contra la COVID-19 y el rechazo a la misma siguen siendo un gran problema de salud pública a nivel mundial, especialmente en Oriente Medio y los países del norte de África. El objetivo del estudio actual es evaluar la intención de recibir las vacunas contra la COVID-19 y sus determinantes entre el público general de Argelia.
MétodosSe distribuyó una encuesta autoadministrada durante agosto-septiembre de 2021, utilizando un enfoque de muestreo basado en conveniencia. Los datos fueron recopilados de manera anónima utilizando el software IBM SPSS v22.0.
ResultadosLa muestra del estudio incluyó un total de 656 participantes, de los cuales el 51,1% estuvo a favor de las vacunas contra la COVID-19, y el 18,5% y el 30,5% estuvo en contra o tuvo dudas, respectivamente. Solo el 38,6% de los participantes del estudio acudió a vacunarse. Los factores asociados a las mayores probabilidades de aceptación fueron: sexo masculino, profesión sanitaria, creencia en el origen natural de la pandemia e infección por COVID-19 previa en la familia. Los motivos más comúnmente citados para la aceptación de la vacuna contra la COVID-19 fueron la creencia en que la vacuna es el único modo de luchar contra la enfermedad, y el miedo a infectarse por el virus, mientras que los motivos más comunes de rechazo fueron la falta de confianza en las pruebas de la propia vacuna y el miedo a los efectos secundarios.
ConclusiónEl nivel general de aceptación de la vacuna contra la COVID-19 en este estudio estuvo por debajo de los niveles requeridos para lograr la inmunidad de la población. Además de ciertas características socio-demográficas, los determinantes del rechazo a la vacuna contra la COVID-19 incluyeron la adhesión a ideas conspiratorias en cuanto al virus y su vacuna. Esto deberá considerarse a la hora de implementar medidas intervencionistas encaminadas a promover la vacuna contra la COVID-19 en el país.
Two years have passed since the first reports on coronavirus disease 2019 (COVID-19), with the negative consequences of the pandemic being far from proper control.1 In the initial phase of the pandemic, the absence of vaccines and effective therapies against the causative agent: severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), forced the preventive efforts to rely mostly on non-pharmaceutical interventions (NPIs).2 These measures included restricting mass gatherings, stay at home orders, and enforcing face masks to limit the forward transmission of the virus.3 This approach helped to control the virus spread; however, the protracted implementation of NPIs can be linked to devastating psychologic, social and economic consequences.4
Attaining population immunity through vaccination appears as the safest central public health measure to control virus spread and to lessen the health, social and economic burden of the disease.5 As of November 2021, a total of 24 COVID-19 vaccines were approved by at least one country, and eight vaccines were approved by the WHO.6 However, vaccine uptake has been suboptimal in many countries worldwide, with barriers involving unequal vaccine distribution, and widespread misinformation and conspiracy beliefs surrounding COVID-19 vaccines.7–9 Safety concerns, and lack of confidence in vaccine efficacy were central among different studies as the predictors of COVID-19 vaccine hesitancy.10
Algeria launched the COVID-19 vaccination campaign by the end of January 2021. In the country, COVID-19 vaccination is mainly based on Sputnik V vaccine (Gam-COVID-Vac), Oxford–AstraZeneca vaccine and the Sinopharm/Sinovac vaccines.11 The number of fully-vaccinated people in Algeria at the time of manuscript writing was 6.11 million, representing a merely of 13.9% of the total Algerian population.12 Such a low level of COVID-19 vaccine uptake can be attributed to low rates of vaccine engagement in the country as evidenced by recent publications which reported generally high levels of COVID-19 vaccine hesitancy in different study groups.13–16 Subsequently, several waves of COVID-19epidemics were observed in the country, with drastic consequences which in turn can result in lower levels of complacency towards the disease and a higher chance of vaccine acceptance.17,18
In the present study, we aimed to investigate the overall rate of COVID-19 vaccine acceptance among the general public in Algeria. Additionally, the study objectives included the investigation of the predictors of COVID-19 vaccine acceptance in the country, besides the assessment of vaccine type preference among the Algerian population.
Material and methodsStudy designThe current study was based on an online questionnaire that was distributed using Google Forms. The survey was distributed based on two non-probabilistic sampling processes; convenience and snowball sampling among Algerian citizens using the following social media and instant messaging platforms: Facebook, Twitter, and WhatsApp.The study was approved by the Scientific Research Committee at the Faculty of Natural and Life Sciences of the University of Djelfa (reference: 170/20-08-2021). Participation in the study was voluntary with no incentives, and all participants provided an informed e-consent prior to their enrollment. Collected data were treated and analyzed confidentially. The survey was distributed in Arabic and French at the same time. The period of survey distribution spanned August 20, 2021 to September 28, 2021.
To estimate the minimum sample size, we used two online tools: “CheckMarket: Sample size calculator”, and “Epitools - Epidemiological Calculators”, with the following parameters: Algerian population of 44,994,071, estimated proportion of 0.5, desired precision of estimate (margin of error) of 4% and 95% confidence level. Based on the previous calculations, we found that 601 participants would represent the minimum sample size in this study.19,20
Overview of the survey itemsThe survey instrument was based on previous literature that investigated COVID-19 vaccine acceptance/hesitancy and with minor modifications.8,15,21–23
After an introductory section containing the objectives of the study and the e-consent to participate, the questionnaire was divided into two main sections comprising mainly closed-ended questions.
The first section assessed the general socio-demographic information including: age, sex, educational level, marital status, occupation (including healthcare-related work [HCW] vs. non-HCW), residence (Algerian provinces and rural vs. urban residence), monthly household income in Algerian dinar (DZD) and history of chronic disease.
The second section included the following items: 1) Assessment of previous influenza vaccine uptake; 2) History of COVID-19; 3) History of hospital admission due to COVID-19; 4) History of COVID-19 among relatives; 5) History of COVID-19-related mortality among relatives; 6) Belief regarding the origin of SARS-CoV-2 (natural vs. man-made); and 7) The item that was considered as the primary outcome measure assessing attitude towards COVID-19 vaccination was phrased as follows “Are you in favor of or against COVID-19 vaccination?” (in favor of vaccination vs. against vaccination vs. no opinion).The participants who opposed vaccination were asked to identify the reason for vaccine rejection with multiple selections allowed from the following list: a) COVID-19 vaccines are ineffective; b) COVID-19 vaccines can cause infertility; c) COVID-19 vaccines contain microchips to control people; d) Fear of long-term side effects; e) I have been previously infected by SARS-CoV-2; f) Pharmaceutical companies are only interested in making financial profits; g) The vaccines were developed without sufficient testing; h) Vaccinated individuals still die due to COVID-19; and i) Vaccinated individuals still get infected by SARS-CoV-2. An additional item was used to assess COVID-19 vaccine uptake “Have you received COVID-19 vaccination?”. Those who received the vaccine were asked to identify the reason for vaccine acceptance, with multiple selections allowed from the following list: a) Vaccination in the only way to fight COVID-19; b) Because I fear of getting infected by the virus; c) My doctor advised me to get COVID-19 vaccination; d) Because a family member got infected by the virus; e) Because a family member died due to COVID-19; f) Because a family member/friend got vaccinated; g) Because it is obligated by the government. The rest of survey items assessed COVID-19 vaccine type preference, reason for such a preference and type of vaccine received among those who were vaccinated.
Statistical analysisStatistical analysis was performed using IBM SPSS v22.0 software for Windows with a significance level determined at p<0.05. Chi-squared (χ2) test was used to analyze associations between categorical variables and univariate analysis was used to assess the possible association between beliefs about SARS-CoV-2 origin and vaccine acceptance with different covariates that include: age, sex, educational level, residence, relationship status and monthly income. Multinomial regression analysis was used to eliminate possible confounding factors in the assessment of COVID-19 vaccine acceptance, COVID-19 vaccine uptake and their predictors.
ResultsCharacteristics of the study respondentsThe total number of participants was 669, with 13 that were excluded for lack of e-consent, or suspected careless responses. The majority of respondents were between 21 and 40 years (71.49%), and were females (56.10%). The vast majority of respondents had a university-level education (91.01%), living in urban areas (81.86%), with a monthly income of 50,000 Algerian dinar (DZD) or less (70.43%) and were either single (50%) or married (47.10%).
The number of respondents with healthcare profession was 190 (28.96%), and about one-fifth of the respondents (19.51%) reported a history of chronic disease.
On the other hand, more than a half of the study respondents reported a previous history of COVID-19 diagnosis (51.98%), with 38.71% being diagnosed in the past three months. Additionally, a majority (86.59%) reported a previous COVID-19 diagnosis in family (Table 1).
Summary of the characteristics of the study respondents (N=656).
| Variable | Category | Number | Percentage (%) |
|---|---|---|---|
| Age | ≤ 20 years | 21 | 3.20 |
| 21–30 years | 275 | 41.92 | |
| 31–40 years | 194 | 29.57 | |
| 41–50 years | 119 | 18.14 | |
| 51–60 years | 44 | 6.71 | |
| > 60 years | 3 | 0.46 | |
| Sex | Male | 288 | 43.90 |
| Female | 368 | 56.10 | |
| Educational level | School | 59 | 8.99 |
| University | 597 | 91.01 | |
| Healthcare work | Yes | 190 | 28.96 |
| No | 466 | 71.04 | |
| Relationship status1 | Alone | 344 | 52.44 |
| In a relation | 312 | 47.56 | |
| Monthly income | ≤ 50,000 DZD2 | 462 | 70.43 |
| > 50,000 DZD | 194 | 29.57 | |
| Living area | Rural | 119 | 18.14 |
| Urban | 537 | 81.86 | |
| History of chronic disease3 | Yes | 128 | 19.51 |
| No | 528 | 80.49 | |
| History of receiving flu vaccine | YesNo | 114542 | 17.3882.62 |
About a half of the study respondents (51.07%) were in favor of COVID-19 vaccination, while 18.45% were against COVID-19 vaccination and 30.49% had no opinion. Only 253 (38.57%) participants stated that they got vaccinated against COVID-19 (Table 3).
Regarding the view of the participants towards COVID-19 vaccine effectiveness, the majority stated that vaccination is either effective (21.80%), or effective depending on vaccine type (29.73%). A total of 84 (12.80%) respondents stated that COVID-19 vaccination is ineffective and 234 (35.67%) had no opinion.
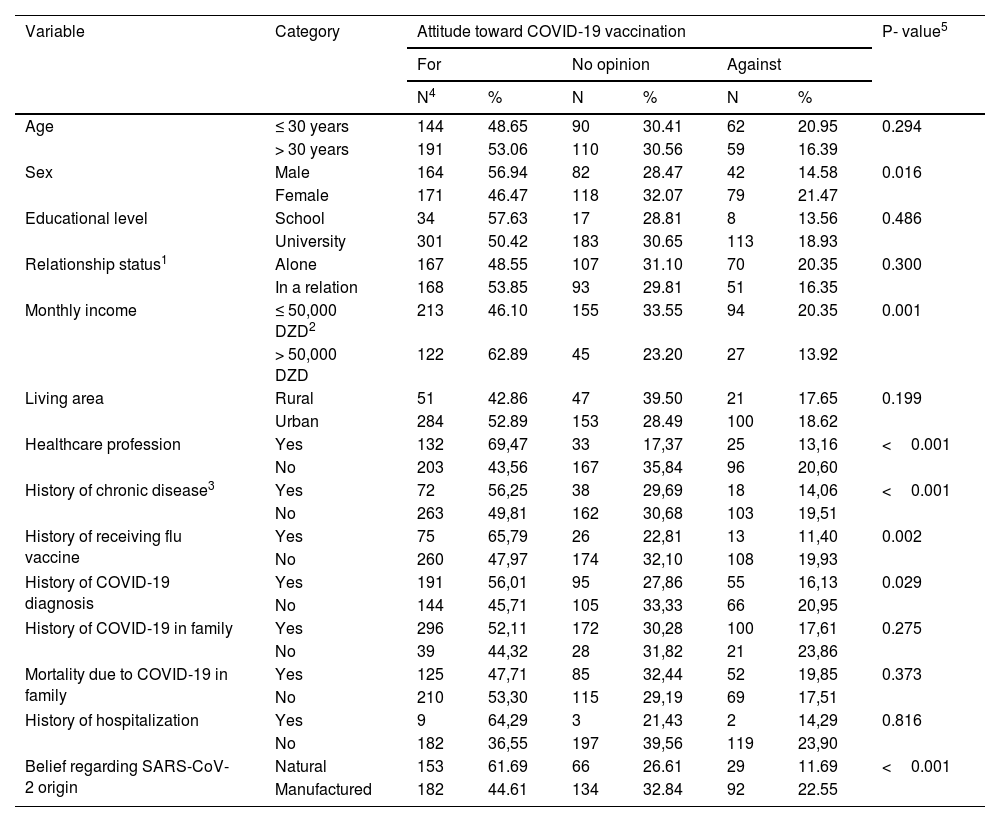
Factors that were associated with being in favour of COVID-19 vaccination included male sex, being a healthcare worker, having a higher monthly income, the belief in natural origin of SARS-CoV-2, history of chronic diseases, previous influenza vaccine uptake and previous diagnosis of COVID-19 (Table 2).
Associated factors with attitude towardCOVID-19 vaccine in Algeria.
| Variable | Category | Attitude toward COVID-19 vaccination | P- value5 | |||||
|---|---|---|---|---|---|---|---|---|
| For | No opinion | Against | ||||||
| N4 | % | N | % | N | % | |||
| Age | ≤ 30 years | 144 | 48.65 | 90 | 30.41 | 62 | 20.95 | 0.294 |
| > 30 years | 191 | 53.06 | 110 | 30.56 | 59 | 16.39 | ||
| Sex | Male | 164 | 56.94 | 82 | 28.47 | 42 | 14.58 | 0.016 |
| Female | 171 | 46.47 | 118 | 32.07 | 79 | 21.47 | ||
| Educational level | School | 34 | 57.63 | 17 | 28.81 | 8 | 13.56 | 0.486 |
| University | 301 | 50.42 | 183 | 30.65 | 113 | 18.93 | ||
| Relationship status1 | Alone | 167 | 48.55 | 107 | 31.10 | 70 | 20.35 | 0.300 |
| In a relation | 168 | 53.85 | 93 | 29.81 | 51 | 16.35 | ||
| Monthly income | ≤ 50,000 DZD2 | 213 | 46.10 | 155 | 33.55 | 94 | 20.35 | 0.001 |
| > 50,000 DZD | 122 | 62.89 | 45 | 23.20 | 27 | 13.92 | ||
| Living area | Rural | 51 | 42.86 | 47 | 39.50 | 21 | 17.65 | 0.199 |
| Urban | 284 | 52.89 | 153 | 28.49 | 100 | 18.62 | ||
| Healthcare profession | Yes | 132 | 69,47 | 33 | 17,37 | 25 | 13,16 | <0.001 |
| No | 203 | 43,56 | 167 | 35,84 | 96 | 20,60 | ||
| History of chronic disease3 | Yes | 72 | 56,25 | 38 | 29,69 | 18 | 14,06 | <0.001 |
| No | 263 | 49,81 | 162 | 30,68 | 103 | 19,51 | ||
| History of receiving flu vaccine | Yes | 75 | 65,79 | 26 | 22,81 | 13 | 11,40 | 0.002 |
| No | 260 | 47,97 | 174 | 32,10 | 108 | 19,93 | ||
| History of COVID-19 diagnosis | Yes | 191 | 56,01 | 95 | 27,86 | 55 | 16,13 | 0.029 |
| No | 144 | 45,71 | 105 | 33,33 | 66 | 20,95 | ||
| History of COVID-19 in family | Yes | 296 | 52,11 | 172 | 30,28 | 100 | 17,61 | 0.275 |
| No | 39 | 44,32 | 28 | 31,82 | 21 | 23,86 | ||
| Mortality due to COVID-19 in family | Yes | 125 | 47,71 | 85 | 32,44 | 52 | 19,85 | 0.373 |
| No | 210 | 53,30 | 115 | 29,19 | 69 | 17,51 | ||
| History of hospitalization | Yes | 9 | 64,29 | 3 | 21,43 | 2 | 14,29 | 0.816 |
| No | 182 | 36,55 | 197 | 39,56 | 119 | 23,90 | ||
| Belief regarding SARS-CoV-2 origin | Natural | 153 | 61.69 | 66 | 26.61 | 29 | 11.69 | <0.001 |
| Manufactured | 182 | 44.61 | 134 | 32.84 | 92 | 22.55 | ||
Relationship status: Alone includes single, divorced, separated or widow/widower, while a relation includes married or engaged.
However, persons who had a family member infected or dead from COVID-19 infection and those with a history of hospitalization after COVID-19 infection were not associated with a statistically significant difference in the attitude toward COVID-19 vaccination (Table 2).
Causes of being in favor or against COVID-19 vaccinationAmong the study respondents who were in favor of COVID-19 vaccination, the most common cited reason for acceptance of vaccination was “vaccination in the only way to fight COVID-19” followed by “fear of getting infected by the virus” (Table 3).
The cited reasons for acceptance or rejection of COVID-19 vaccination among the study participants.
| Causes | Frequency (%) |
|---|---|
| Cause of being in favor of COVD-19 vaccines | |
| Vaccination is the only way to fight COID-19 | 85.78 |
| I fear of getting infected by the virus | 34.22 |
| My doctor advised me to get COVID-19 vaccination | 16.89 |
| Because a family member got infected by the virus | 15.11 |
| Because a family member is died due to COVD19 | 14.22 |
| Because a family member/fried got vaccinated | 10.67 |
| Because it is obligated by the government | 04.89 |
| Causes for COVID-19 vaccines opposition | |
| Vaccines were developed without sufficient testing | 81.82 |
| Fear o long term side effects | 62.81 |
| Pharmaceutical companies are only interested in making financial profits | 40.50 |
| Vaccinated individuals still die due to COVID-19 | 38.02 |
| Vaccinated individuals still get infected by SARS-CoV-2 | 34.71 |
| COVID-19 vaccines are ineffective | 26.45 |
| COVID-19 vaccines can cause infertility | 21.49 |
| I have been previously infected by SARS-CoV-2 | 19.83 |
| COVID-19 vaccines contain microchips to control people | 09.09 |
For those who were against vaccination, the most common cited reasons were the belief that COVID-19 vaccines have not been tested properly and the fear of long-term side effects (Table 3).
Attitude toward SARS-CoV-2 originThe majority of study participants believed that SARS-CoV-2 is man-made (62.20%). The acceptance of COVID-19 vaccination was higher among those who believed in natural origin of the virus compared to those who believed it was manufactured (61.69% vs. 44.61%, p<0.001). Univariate analysis showed the independent correlation between the belief in natural SARS-CoV-2 origin and higher COVID-19 vaccine acceptance (p<0.001), with the following covariates: age, sex, educational level, residence, relationship status and monthly income.
We conducted multinomial logistic regression analysis to assess the association between attitude towards COVID-19 vaccination (for vs. against with removal of “no opinion category”) with the following factors: previous influenza vaccine uptake, COVID-19 diagnosis, hospitalization due to COVID-19, COVID-19 diagnosis in family, mortality due to COVID-19 in a family member, attitude towards SARS-CoV-2 origin, and the following as covariates: age (≤ 30 years vs. > 30 years), sex, educational level (school vs. university), occupation (HCW vs. non-HCW), relationship status (alone vs. in a relation), monthly income (≤ 50,000 DZD vs. > 50,000 DZD), residence (rural vs. urban), and history of chronic disease.
Analysis showed that the belief in natural origin of SARS-CoV-2 was significantly correlated with COVID-19 vaccine acceptance (OR: 2.3, 95% CI: 1.3 – 3.9). Also, healthcare workers (OR: 2.15, 95% CI: 1.20 – 3.86), males (OR: 1.92, 95% CI: 1.11 – 3.33) and individuals who had at least one family member previously affected by COVID-19 (OR: 2.13, 95%CI: 1.01 – 4.48) have been associated with a high odds of vaccine acceptance (Table 4).
Multinomial regression analysis of COVID-19 vaccine acceptance with variable factors.
| Variable | Odds ratio (95% CI)1 | p-value |
|---|---|---|
| Previous influenza vaccine uptake (Yes vs No) | 1.94 (0.95– 3.96) | 0.068 |
| COVID-19 diagnosis | 1.24 (0.72–2.13) | 0.436 |
| Hospitalization due to COVID-19 | 0.75 (0.13 –4.35) | 0.744 |
| COVID-19 diagnosis in family | 2.13 (1.01 – 4.48) | 0.047 |
| Mortality due to COVID-19 in a family member | 0.70 (0.41–1.20) | 0.194 |
| Belief in natural origin of SARS-CoV-2 | 2.29 (1.33–3.93) | 0.003 |
| Covariates | ||
| Age (≤ 30 years vs. > 30 years) | 0.87 (0.44 – 1.69) | 0.672 |
| Sex (male vs. female) | 1.92 (1.11 – 3.33) | 0.020 |
| Educational level (school vs. university) | 1.21 (0.49 – 2.99) | 0.678 |
| Occupation (HCW vs. non-HCW) | 2.15 (1.20 – 3.86) | 0.010 |
| Relationship status (alone vs. in a relation) | 1.12 (0.58 – 2.14) | 0.735 |
| Monthly income (≤ 50,000 DZD vs. > 50,000 DZD) | 0.52 (0.27 – 1.00) | 0.051 |
| Residence (rural vs. urban) | 1.12 (0.56 – 2.25) | 0.749 |
| History of chronic disease (Yes vs. No) | 1.61 (0.81 – 3.19) | 0.177 |
Among the 253 participants who reported the uptake of COVID-19 vaccination, the vast majority got Sinovac/Sinopharm vaccine (80.80%), followed by Sputnik V vaccine (9.10%) and the AstraZeneca vaccine (8.70).
Regarding COVID-19 vaccine preference, results showed that while about one-fifth had no preference to any vaccine type, the Sinovac/Sinopharm and Pfizer BioNTech vaccines had the first place in as the preferred type in the study sample (Table 5).
COVID19-vaccine preference among vaccinated and non-vaccinated participants in the study.
| COVID-19 vaccine preference | Proportion (%) | ||
|---|---|---|---|
| Vaccinated individuals | Non-vaccinated individuals | Total | |
| No preference | 16.61 | 25.75 | 21.17 |
| Sinovac/Sinopharm | 31.89 | 28.43 | 30.17 |
| Pfizer BioNTech | 19.93 | 16.72 | 18.33 |
| AstraZeneca | 10.30 | 7.69 | 9 |
| Sputnik V | 8.31 | 12.37 | 3.53 |
| Moderna | 6.64 | 4.35 | 5.50 |
| Johnson& Johnson | 6.31 | 4.68 | 5.50 |
The most reported reasons for COVID-19 vaccine preference were their efficacy (for all vaccines), the conventional method of production and the availability for Sinovac/Sinopharm vaccine, and the confidence in the manufacturer and the country of production for the other vaccines like Pfizer-BioNTech and AstraZeneca vaccines.
DiscussionThe current study was conducted to investigate the attitude of the general population in Algeria towards COVID-19 vaccines and its associated determining factors. In Algeria, the early reports on COVID-19 vaccine acceptance rates among various populations (the general public, students, and HCWs) have shown a high rate of COVID-19 vaccine hesitancy.13–16 The findings of this study pointed to a slightly higher rate of COVID-19 vaccine acceptance that was estimated at 51.07%. This increase can be partly explained by the timing survey distribution of this study, which coincided with an intensive campaign to increase COVID-19 vaccines uptake in the country that started in August, 2021 following the third wave of COVID-19 in Algeria which was accompanied by drastic consequences.24
Looking into the results of this study from a global perspective, COVID-19 vaccine acceptance rate in this study can still be viewed as an inferior rate.7,9 For instance, the results of an early systematic review on the global rates of COVID-19 vaccine acceptance showed that the highest rates were found in Ecuador (97%), Malaysia (94.3%), Indonesia (93.3%) and China (91.3%).9 A more recent narrative review addressing the same objective showed that the COVID-19 vaccine acceptance rates in a majority of countries in Latin America, Asia, Western Europe, and North America were much higher compared to the results of this study.7 Nevertheless, our findings were consistent with generally high levels of COVID-19 vaccine hesitancy observed in the majority of the Middle East and North Africa (MENA) region and among other African countries.7–9,15,21
Specifically, the rates of COVID-19 vaccine acceptance were as high as 80.9% in Ethiopia, 79.2% in Saudi Arabia and 77% in Somalia, and as low as 15.5% in Cameroon, 21.4% in Lebanon and 25% in Egypt.25
In this study, the most common cited reasons for being in favor of COVID-19 vaccination were related to high level in vaccine confidence: “vaccination in the only way to fight COVID-19” and low levels of complacency towards the disease: "the fear of getting infected by the virus", while the most common reasons for opposing vaccination among the participants that were against COVID-19 vaccination were: “vaccines have not been sufficiently tested” and “the fear of long-term adverse effects of the vaccines” which entails low levels in vaccine confidence. Thus, vaccine confidence can be viewed as one of the most important predictors of COVID-19 vaccine acceptance/rejection. This result is in accordance with the findings of several studies where the rapidity in vaccine production, the hesitancy in vaccine effectiveness and the fear of long-term side effects were the main causes of vaccine rejection.15,26,27
Several factors were found to be associated with COVID-19 vaccine acceptance in this study. For example, healthcare workers were found to be significantly more in favor of COVID-19 vaccination compared to the general population (OR: 2.15, 95% CI: 1.20 – 3.86). Similar pattern was seen in previous studies from Mozambique and Somalia.25,28 Surprisingly, the opposite pattern was observed in the Democratic Republic of Congo where healthcare workers were more hesitant to COVID-19 vaccines compared to the general population.29
The relatively high rate of COVID-19 vaccine acceptance among healthcare workers in this study might be a starting point for improving the uptake rates for the vaccine in the country, considering their important role in providing the general public with accurate messages regarding the safety and efficacy of COVID-19 vaccines and its invaluable role to fight the ongoing pandemic.8,21
For the other factors that were found to be correlated with COVID-19 vaccine acceptance in this study, male sex was associated with higher rates of vaccine acceptance compared to female sex. Such a result was consistent with findings of previous studies where men were more favorable for vaccination than women and one possible explanation for such disparity is the previous evidence of higher embrace of conspiracy beliefs about the virus and its vaccines among females.7,8 Other potential factors that can contribute to higher rates of vaccine hesitancy among females include the higher levels of fear of injections or side effects, and the observation that the disease is more deadly in males.14,30
In this study, history of influenza vaccine uptake, age, educational level, monthly income, history of chronic disease, and being affected by COVID-19 (among the participants or their relatives) were not correlated to attitude towards COVID-19 vaccination. This could represents a genuine observation or might be a finding related to the relatively small sample size since these factors were previously considered as frequent correlates with attitude towards vaccination.8,15,23,28,29
One of the most important findings in this study was the observation that conspiracy beliefs (in the form of embracing the idea that SARS-CoV-2 is man-made) can be considered as a barrier of vaccine uptake. Our findings indicated that about two thirds of the study sample believed that the virus was manufactured, and such an observation is not unique to our study and appears widely prevalent in the MENA countries.8,21
Regarding COVID-19 vaccine type preference, our results showed that the most preferred types among the study participants were Sinovac/Sinopharm and Pfizer-BioNTech vaccines, with the later type being the preferred vaccine among HCWs in Kuwait.23
Study limitationsThis study was conducted using an online questionnaire-based cross-sectional design with a convenient and snowball sampling approach. Consequently, the generalizability of our results is limited by selection bias. The online distribution of the survey could have resulted in a biased sampling with less coverage among individuals with limited access to internet.
ConclusionsIn conclusion, this study provided an overview of the attitude of the Algerian population towards COVID-19 vaccination and the factors associated with vaccine acceptance and hesitancy. Results showed a remarkable increase in COVID-19 vaccine acceptance, especially among healthcare workers compared to previous studies; nevertheless, the rate of COVID-19 vaccine acceptance remains low in the general population. These findings suggest the need of strengthen awareness campaigns highlighting the safety, efficacy and importance of COVID-19 vaccination to reduce the burden of the disease and to control the ongoing pandemic. The high rate of vaccines acceptance among healthcare workers can be encouraging, considering their potential role as an accurate source of information about COVID-19 vaccination for the general population, which may help to increase the overall rates of vaccine uptake in the country. Another important finding was the finding that higher rates of COVID-19 vaccine hesitancy and rejection were found among individuals who embraced conspiratorial beliefs (that the virus is man-made), which highlight the importance of fighting the infodemic part of the pandemic.
FundingNone