Food allergy, which becomes an important public health problem, can lead to important morbidity and mortality. Patients with food allergies are more likely to first present to their primary care physicians. We aimed to determine the knowledge of primary care physicians with regard to management of food allergies and anaphylaxis.
MethodsPrimary care physicians were surveyed via a questionnaire aimed to document their knowledge and attitudes about food allergy and anaphylaxis management.
ResultsA total of 297 participants completed questionnaires, 55.6% of which were female. Participating physicians had a mean of 17.0±6.1 years of experience. Participants answered 47.2% of knowledge-based items correctly. Overall, participants fared poorly with regard to their knowledge on the treatment of food allergies and anaphylaxis. For example while 60.7% knew that a child can die from the milk allergy reaction, only 37.5% were aware that a child with IgE mediated milk allergies cannot eat yoghourts/cheese with milk. Besides, 53.1% of them chose epinephrine as their first treatment of choice in case of anaphylaxis, yet only 16.6% gave the correct answer about its dosage. Nearly a third of participants (36.7%) felt they were knowledgeable enough regarding the management of patients with food allergies, while 98.2% extended their request for future periodic educational meetings on allergic disorders.
ConclusionKnowledge of food allergy and anaphylaxis among primary care physicians was unsatisfactory. Provision or periodic educational programmes should be aimed at improving the standard of practice as acknowledged by the participants.
Food allergy is a term used to describe immunological reactions that develop against foods, and is believed to actively affect nearly 4% of children.1,2 Food allergy can lead to atopic dermatitis, failure to thrive, malnutrition and may cause death owing to anaphylaxis.3,4 It has been widely accepted that food allergies are the initial step of the atopic march, which means that these patients will have a tendency to develop respiratory allergies like asthma and allergic rhinitis in the future. The last 2–3 decades have witnessed a sharp increase in the prevalence of food allergies with increased worldwide concern to what is now considered an important public health problem.2,5
Inappropriate dietary recommendations by physicians due to over or under diagnosis, rooted in poor knowledge of the subject matter, would detrimentally affect the quality of life of patients and their relatives alike and may cause malnutrition, while also posing a great risk for the development of potentially fatal anaphylaxis.6,7 Patients with food allergies are more likely to first present to their primary care physicians and at the very least the primary care physicians are expected to recognise the signs of food allergy to make an appropriate referral to an allergist and urgent management of the emergencies during follow up of the patients. Accordingly, the physicians having enough knowledge about the food allergies and treatment of its related risks such as anaphylaxis will improve patients’ quality of life by means of providing a decrease in morbidity and mortality.8 Therefore it is essential to improve the knowledge gaps of primary care physicians regarding the management of food allergies.
The aim of this study was to determine the knowledge as well as the attitudes of primary care physicians with regards to food allergies and anaphylaxis, so that educational programmes can be organised in order to improve the missing aspects of their knowledge.
MethodsStudy populationThe study population consisted of primary health care physicians practicing in Ankara, the capital of Turkey. Officially, the primary health care system has been active in Ankara since the middle of 2010. There were also primary care services before 2010 but the patients had the right to apply to any hospitals (including university hospitals) and to any specialists without going to the primary care physicians. After this date, the Ministry of Health made it mandatory for health care application. In a three month period, between March and May 2010, three education meetings were held to which primary care physicians from all of Ankara's districts were invited, with an estimated turnout of 350 physicians. Although there might be small differences between the medical schools, all participants had at least 15–20h allergy teaching in the curriculum of their medical school studies.
The study was approved by the institutional review board of Ankara Children's Hematology Oncology Education and Research Hospital and informed consent was obtained from the participants by orally.
Study designIt was during these meetings that physicians were asked to fill out questionnaires which were distributed on the morning of the meetings and collected on the same day by the end of each day. Participating physicians did not have prior knowledge on the objectives of the study. The survey consisted of questions that were mainly based on the validated questionnaire formed by Gupta et al. and guidelines.9,10 The distributed questionnaires included questions on the demographic characteristics of the participating physicians and their knowledge and attitudes regarding the diagnosis, symptoms, severity, triggers, risk factors and treatment of food allergies. It also included questions related to treatment of anaphylaxis. Participants were divided into two groups based on their own perceptions on their level of knowledge, and into independent two groups based on whether they or their close relatives have been diagnosed with a food allergy.
Statistical analysisDescriptive statistics were provided for demographic characteristics and responses to each question on the questionnaire. Each participant was awarded a score based on the number of correct responses. Comparisons were made in groups of two, based on gender, years of experience, presence of a close relative diagnosed with a food allergy, and self-perception of participants regarding their knowledge on the subject matter. Categorical variables and continuous variables were compared with Chi-square test and Man Whitney U test respectively. A p-value of ≤0.05 was considered indicative of statistical significance. SPSS-15 statistical software package (SPSS, Inc., Chicago, IL, USA) was used for the analyses.
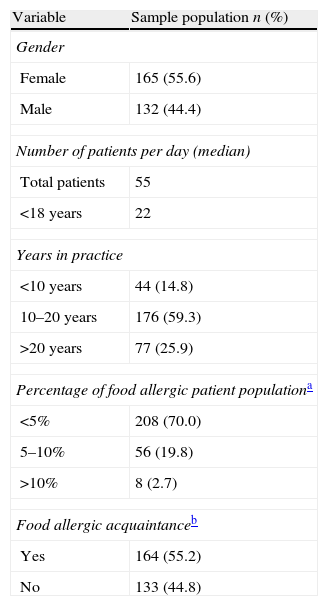
ResultsCharacteristics of participantsA total of 297 participants, who were practicing primary care physicians at primary care health centres, returned completed questionnaires suitable for evaluation, 55.6% of whom were female. Participating physicians had a mean of 17.0±6.1 years of experience (range 1–33 years), most of whom reported caring for 500–600 patients a week from all age groups, including 150–200 children per week. Ninety-two percent of physicians responded as having patients with food allergies in their care, although such patients only compromised <5.0% of their patient load (Table 1).
Demographic characteristics of primary care physicians (n: 297).
| Variable | Sample population n (%) |
| Gender | |
| Female | 165 (55.6) |
| Male | 132 (44.4) |
| Number of patients per day (median) | |
| Total patients | 55 |
| <18 years | 22 |
| Years in practice | |
| <10 years | 44 (14.8) |
| 10–20 years | 176 (59.3) |
| >20 years | 77 (25.9) |
| Percentage of food allergic patient populationa | |
| <5% | 208 (70.0) |
| 5–10% | 56 (19.8) |
| >10% | 8 (2.7) |
| Food allergic acquaintanceb | |
| Yes | 164 (55.2) |
| No | 133 (44.8) |
To the question on the three most common food allergies, most participants responded that they were eggs, milk and strawberry.
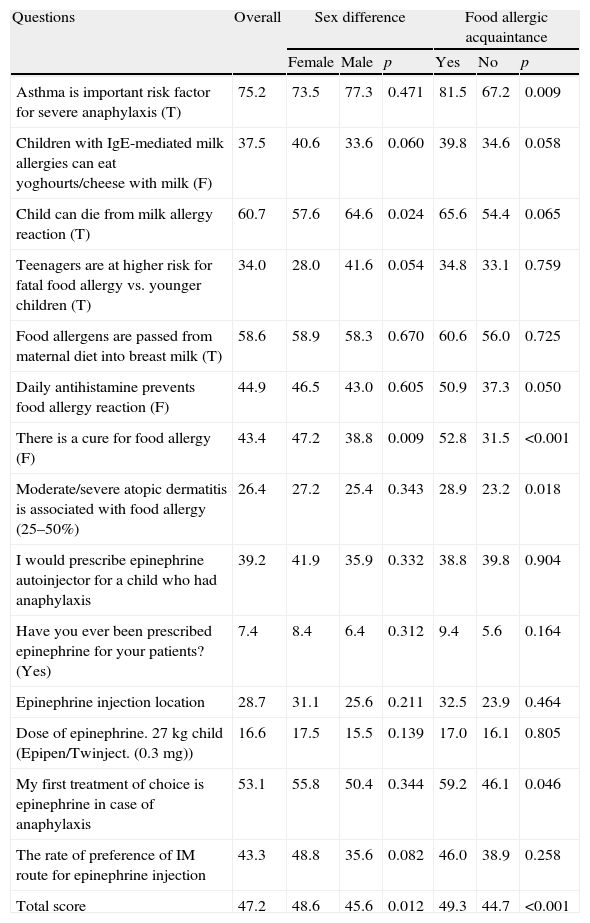
The average score to questions testing their knowledge on food allergies and anaphylaxis was 47.2% (8–71%). More than half of the participants knew that food allergens can pass through to child via breast milk but 26.4% of them have correct knowledge about the relationship between moderate–severe AD and food allergy. The rates of correct responses for each question are summarised in Table 2. While a majority of participants responded correctly to questions on asthma as a risk factor for anaphylaxis and cow's milk allergy related mortality (75.2% and 60.7%, respectively), rate of correct responses to questions on the treatment of anaphylaxis was very low. While nearly half of them prefer epinephrine as their first treatment of choice in case of anaphylaxis only 16.6% of the participants knew the correct dosage of epinephrine. Besides this although 39.2% of them reveal that epinephrine autoinjector should be prescribed for a child who had anaphylaxis, only 7.4% of them prescribed the former treatment during their practice.
Percentage of correct answers of the participants and comparisons according to sex, self confidence and food allergic acquaintance.
| Questions | Overall | Sex difference | Food allergic acquaintance | ||||
| Female | Male | p | Yes | No | p | ||
| Asthma is important risk factor for severe anaphylaxis (T) | 75.2 | 73.5 | 77.3 | 0.471 | 81.5 | 67.2 | 0.009 |
| Children with IgE-mediated milk allergies can eat yoghourts/cheese with milk (F) | 37.5 | 40.6 | 33.6 | 0.060 | 39.8 | 34.6 | 0.058 |
| Child can die from milk allergy reaction (T) | 60.7 | 57.6 | 64.6 | 0.024 | 65.6 | 54.4 | 0.065 |
| Teenagers are at higher risk for fatal food allergy vs. younger children (T) | 34.0 | 28.0 | 41.6 | 0.054 | 34.8 | 33.1 | 0.759 |
| Food allergens are passed from maternal diet into breast milk (T) | 58.6 | 58.9 | 58.3 | 0.670 | 60.6 | 56.0 | 0.725 |
| Daily antihistamine prevents food allergy reaction (F) | 44.9 | 46.5 | 43.0 | 0.605 | 50.9 | 37.3 | 0.050 |
| There is a cure for food allergy (F) | 43.4 | 47.2 | 38.8 | 0.009 | 52.8 | 31.5 | <0.001 |
| Moderate/severe atopic dermatitis is associated with food allergy (25–50%) | 26.4 | 27.2 | 25.4 | 0.343 | 28.9 | 23.2 | 0.018 |
| I would prescribe epinephrine autoinjector for a child who had anaphylaxis | 39.2 | 41.9 | 35.9 | 0.332 | 38.8 | 39.8 | 0.904 |
| Have you ever been prescribed epinephrine for your patients? (Yes) | 7.4 | 8.4 | 6.4 | 0.312 | 9.4 | 5.6 | 0.164 |
| Epinephrine injection location | 28.7 | 31.1 | 25.6 | 0.211 | 32.5 | 23.9 | 0.464 |
| Dose of epinephrine. 27kg child (Epipen/Twinject. (0.3mg)) | 16.6 | 17.5 | 15.5 | 0.139 | 17.0 | 16.1 | 0.805 |
| My first treatment of choice is epinephrine in case of anaphylaxis | 53.1 | 55.8 | 50.4 | 0.344 | 59.2 | 46.1 | 0.046 |
| The rate of preference of IM route for epinephrine injection | 43.3 | 48.8 | 35.6 | 0.082 | 46.0 | 38.9 | 0.258 |
| Total score | 47.2 | 48.6 | 45.6 | 0.012 | 49.3 | 44.7 | <0.001 |
F: false; IgE: Immunoglobulin E; T: true
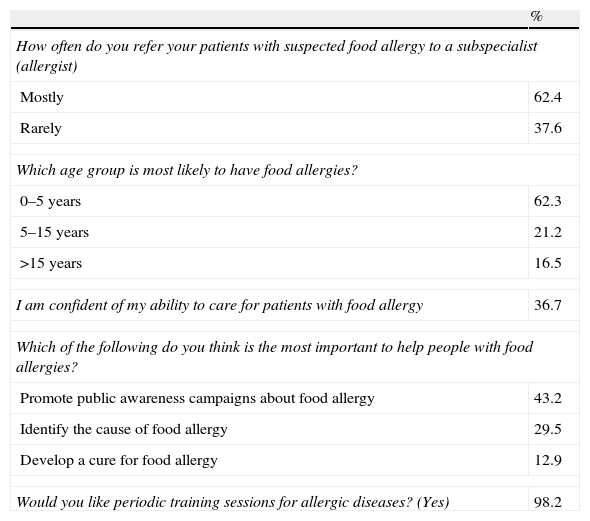
Regarding questions on attitude and approach of participants to food allergies, 62.4% responded that they commonly refer such patients to allergy specialists, while only 37.6% responded that they rarely refer such patients for further evaluation. To the question on the best approach to help patients with food allergies, 43.2% of participants cited campaigns aimed at raising awareness, 29.5% cited the identification of the causes of food allergy and 12.9% cited development of new treatment strategies to cure food allergies as the most suitable approach. Nearly a third of participants (36.7%) felt they were knowledgeable enough regarding the management of patients with food allergies, while 98.2% extended their request for future periodic educational meetings on allergic disorders (Table 3).
Participants’ attitudes and approaches to food allergy.
| % | |
| How often do you refer your patients with suspected food allergy to a subspecialist (allergist) | |
| Mostly | 62.4 |
| Rarely | 37.6 |
| Which age group is most likely to have food allergies? | |
| 0–5 years | 62.3 |
| 5–15 years | 21.2 |
| >15 years | 16.5 |
| I am confident of my ability to care for patients with food allergy | 36.7 |
| Which of the following do you think is the most important to help people with food allergies? | |
| Promote public awareness campaigns about food allergy | 43.2 |
| Identify the cause of food allergy | 29.5 |
| Develop a cure for food allergy | 12.9 |
| Would you like periodic training sessions for allergic diseases? (Yes) | 98.2 |
Comparisons with regards to correct responses to each question were made in groups of two based on gender, years of experience presence of a close relative diagnosed with a food allergy, and self-assessment of participants regarding their knowledge on the subject matter.
Female physicians were older than the males (40±5.6 years vs. 44.8±6.18 years, respectively, p<0.001) and had a higher duration of experience (15.6±5.8 vs. 18.8±6.2, respectively, p<0.001). Female participants scored significantly higher than their male counterparts (48.5% vs. 45.6%; p=0.012), however the difference between sexes regarding the approach and treatment of anaphylaxis was statistically insignificant.
Participants were divided into three groups according to the duration of their experience: (1) lower than 10 years; (2) between 10 and 20 years; and (3) higher than 20 years. There was no significant difference between these groups according to their total scores (p: 0.330). Participants had a median of 17 years of experience (44.7% >17 years). We also did not find any difference by using 17 years of experience as a cut-off point in terms of total score or knowledge on the diagnosis and treatment of food allergies and prophylaxis (data not shown).
Particularly for the questions on the treatment of anaphylaxis, such as the correct location of epinephrine and its dosage, participants who believed themselves knowledgeable enough with regards to the management of treatment of patients of food allergies scored higher than those who perceived themselves as less knowledgeable. However, there was no significant difference on food allergy and in mean overall scores (Table 2).
Participants suffering from food allergies or with close relatives having such an affliction scored significantly higher on questions regarding risk factors for anaphylaxis and the treatment of food allergies compared to participants without first-hand experience. They also gave the correct response, adrenalin, as the first choice of treatment in anaphylaxis more commonly than those without personal experience (59.2% and 46.1% respectively; p: 0.046).
DiscussionOverall, participants fared poorly with regard to their knowledge on the treatment of food allergies and anaphylaxis. Although most participants correctly identified cow's milk allergy as potentially fatal, more than half responded that children with cow's milk allergy could consume cheese and yoghurt. Similarly, most participants were aware that as a risk factor, some food allergens may be transferred to children via breast milk, whereas only 26.4% believed that moderate–severe atopic dermatitis could be associated with food allergies. Most of the participating physicians did not know the correct dose or the most appropriate route and site for the application of adrenalin. Despite the lack of knowledge regarding food allergies, 40.0% of participants reported that they do not refer such patients to allergy specialists.
The mean score of all participants was 47.2%, a value close to that observed in a similar study on primary care physicians by Gupta et al.10 The similarity of the scores, despite the differences in educational background of physicians representing different populations, highlights the shared concerns regarding the diagnosis and treatment of food allergies.
A vast majority of participants correctly identified that food allergies are most commonly observed in the first five years of life, however, only 62.4% claimed to refer such patients under their care to allergy specialists. While 43.4% of participating physicians were aware that there is as yet no cure for food allergies, 55.1% believed that antihistamines could be used to manage such patients. Food allergies generally develop within the first three years of life, decreasing gradually with time.11 The treatment of food allergies involves elimination of the offending food allergen from the diet, and despite the promising results of studies on food allergy immunotherapy, this treatment modality is yet to take its place in routine clinical practice.12
There were several discrepancies in the responses to questions on food allergies and associated risk factors. For example, while 60.7% of participants were aware that cow's milk was capable of instigating a fatal reaction, and 58.6% knew that food allergens may pass to the baby via breast milk, only 37.5% of physicians knew that yoghourt and cheese should also be avoided in such situations. In patients with confirmed allergy to cow's milk protein, all dairy products should be completely eliminated from the diet, and in breast-feeding infants, the mother should also avoid dairy products in her diet until ceasing breast-feeding. Moreover, only a third of participants were aware that adolescents are a group at high risk for the development of fatal allergic reactions to foods. Adolescents tend to spend most of their time away from home, and this along with their predilection for inappropriate behaviour puts them at high risk for the development of allergic reactions.13
Nearly a quarter of participants responded correctly to the question on the link between moderate–severe atopic dermatitis and food allergy. Atopic dermatitis is the most commonly encountered chronic recurrent inflammatory disorder of the skin in children. Moderate–severe atopic dermatitis has been reported to occur in association with food allergy in 30–35% of patients.14,15 As such, primary care physicians should always consider the presence of a food allergy in patients with moderate–severe atopic dermatitis. In cases who have food allergy related clinically with atopic dermatitis, the allergen should be eliminated from the diet, otherwise it will be difficult to control the dermatological findings.15
Participants’ responses to what they believed were the most frequently encountered food allergens were eggs, milk and strawberries, in decreasing order. It has been reported that the most common childhood food allergens are milk, eggs, soya, wheat and seafood.16 Participants in our study failed to recognise cereals and seafood as common offenders. Interestingly, strawberries, which participants believed to be the third most common food allergens, are not a frequent cause of food allergies. However, it is important to mention that strawberries contain histamine and tyramine which may trigger a response mimicking a type 1 hypersensitivity reaction.17 In addition, several foods, including strawberries, may show cross-reactivity with pollens.18 All of these factors may cause confusion, explaining the frequency of participants incorrectly selecting strawberry among the more common allergens.
The lowest scores obtained were with questions on the treatment of anaphylaxis. While 53.1% of physicians correctly choose adrenalin as the drug of choice for the treatment of patients with anaphylaxis, 43.3% preferred intramuscular application compared to 56.7% who advocated subcutaneous administration of the drug. Only 27.0% of participants responded correctly for the most appropriate site of administration for adrenalin. Furthermore, only 16.6% of participating physicians calculated the preferred dose of adrenalin for child weighing 27kg. With regards to adrenalin autoinjectors, 7.4% of physicians admitted to having prescribed them, although only 5.8% were aware of instructions of use. Adrenalin is the first choice of drug in the management of anaphylaxis and is known to significantly decrease mortality due to anaphylaxis.19,20 It is recommended to administer adrenalin at a dose of 0.01mg/kg (1:1000) intramuscularly into the lateral thigh.21 Effective plasma concentrations are achieved much faster with intramuscular application compared to the subcutaneous route.
Use of epinephrine autoinjectors is advocated as a practical approach to the management of anaphylaxis and food allergens are the leading cause of anaphylaxis during childhood.22 When available, self-injectable epinephrine should be immediately administered as an intramuscular (IM) dose to all children with signs and symptoms suspicious of anaphylaxis before arrival to hospital.23 Therefore doctors should be able to demonstrate the correct administration of the autoinjector to the family. For this reason, primary care physicians should be well-informed regarding the proper use of autoinjectors. Taking into consideration the pivotal role of adrenalin in the treatment of anaphylaxis, improving the level of knowledge among primary care physicians is of grave importance.
In our study, physicians with food allergy themselves, or those with relatives affected responded better to questions on risk factors of food allergies and anaphylaxis as well as correctly identifying adrenalin as the drug of choice for the treatment of anaphylaxis. Having the disease himself/herself or acquaintance may influence the physicians to seek for the disease and improve their knowledge about the subject which presumably results in better management of the disease.
Although nearly 300 participants completed our survey, the limitation of this study was that the subjects were not randomly selected and all the primary care physicians were not included in the study. Even though all the primary care physicians were invited to the education meetings only the volunteers came into the programme. Some may speculate that those who have sufficient knowledge might not participate in the education. Although this may be true, physicians claiming to be proficient in the follow-up and treatment of food allergies did not differ from those physicians who did not profess sufficient knowledge on the matter.
In conclusion, primary care physicians were not sufficiently knowledgeable regarding the diagnosis treatment and risk factors for food allergies and related anaphylaxis in Turkey. Patients with food allergies are more likely to first present to their primary care physician, and particularly in the event of a potentially fatal anaphylactic attack, it is prudent that physicians are “up to par” with regard to their knowledge on the management and treatment of food allergies. Provision or periodic educational programmes should be aimed at improving the standard of practice among primary care physicians regarding allergic disorders in general, and food allergies in particular. Any improvement sustained regarding this matter would increase the quality of health care and the quality of life of affected individuals.
Ethical disclosuresPatients’ data protectionConfidentiality of data. The authors declare that no patient data appears in this article.
Right to privacy and informed consentRight to privacy and informed consent. The authors declare that no patient data appears in this article.
Protection of human subjects and animals in researchProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Conflict of interestAll of the authors have no conflicts of interest in the manuscript.