Novel predictors of prognosis in cirrhotic patients have been emerging in recent years and studies show that the lactate/albumin ratio can serve as an early prognostic marker in different patient groups. We aimed to uncover the clinical significance of the lactate/albumin ratio in hospitalized patients with acutely decompensated cirrhosis.
Materials and MethodsA retrospective single-center cohort study was conducted in a tertiary medical center. Subjects included had an established diagnosis of liver cirrhosis and were admitted to the ICU or the Internal Medicine department with a clinical picture of acute-on-chronic liver failure between the years 2010 and 2021. The primary outcome was to assess the utility of the lactate/albumin ratio as a prognostic marker to predict mortality in hospitalized cirrhotic patients with acute-on-chronic hepatic failure.
ResultsTwo hundred seventy-nine patients were included in this study. Univariate analysis revealed that mean WBC count, platelet/creatinine ratio, aspartate transaminase (AST), lactate, and MELD score were all significantly associated with the primary outcome. Multivariate analysis showed that the lactate/albumin ratio was the strongest statistically significant (p < 0.001) predictor of death during hospitalization - OR 13.196 (95% CI 3.6–48.3), followed by mean WBC count, MELD score, and serum lactate levels. A ROC curve was constructed, which resulted in an area under the curve (AUC) equal to 0.77. Crosstabs from the ROC showed a sensitivity of 66.7% and a specificity of 76.2% when the lactate/albumin ratio chosen as a cutoff was 0.9061
ConclusionsElevated lactate/albumin ratio predicts in-hospital mortality in hospitalized cirrhotics with acute-on-chronic hepatic failure.
Cirrhosis is the final pathological outcome of many chronic liver diseases. Although several different etiologies can give rise to cirrhosis, the histopathological features are common: degeneration and necrosis of hepatocytes, replacement of liver parenchyma by fibrotic tissues with regenerative nodules, and loss of liver function. Cirrhotic patients are at an increased risk for significant morbidity and mortality that may stem from complications of portal hypertension or decompensation of their liver function [1].
Novel predictors of prognosis in cirrhotic patients have been emerging in recent years. Liver biopsy and hepatic venous pressure gradient (HVPG) may be used but are finite due to the invasive nature that they possess. The Child-Pugh and the model for end-stage liver disease (MELD) Scores are used to assess the prognosis of cirrhotic patients non-invasively. The former is used to grade the severity of liver disease, and the latter is employed as a verifiable system to prioritize candidates for liver transplantation [2]. The Child-Pugh score has the inherent disadvantage of the subjective nature of the variables used to score, such as hepatic encephalopathy and ascites. On the other hand, the MELD score is more applicable for end-stage patients [2,3]. Several studies have attempted to compare the utility of both scores as prognostic markers for cirrhotic patients, but all were limited by the heterogeneous nature of the populations included. It is, therefore, imperative that new scores are proposed to assess the prognosis of patients with liver cirrhosis.
In recent years, the CLIF-COF (CLIF- consortium organ failure) score, which takes into account variables such as bilirubin, creatinine, INR, and more, has emerged as a superior predictor of prognosis in acute on chronic liver failure than the MELD score [4]. Moreover, studies have shown that serum copeptin level is a predictor of mortality in cirrhotic patients admitted for acute decompensation, independently of MELD and CLIF-COF scores [5].
Albumin is a protein that is secreted from the liver. In cirrhosis patients, the albumin protein undergoes both qualitative and quantitative negative changes. Long-term albumin administration to patients with decompensated cirrhosis has been shown to improve survival and prevent complications [6,7]. Lactate is one of the end-products of anaerobic glycolysis, and the liver is responsible for up to 70% of the human body's lactate clearance. Lactate levels and clearance have been proven to predict the outcome of critically ill patients in the ICU and, specifically, improve the prediction of short-term mortality in critically ill patients with cirrhosis as well as cirrhotic elderly patients [8,9]. Studies show that the lactate/albumin ratio can serve as an early prognostic marker in critically ill patients, as well as specifically in critically ill patients with heart failure [9,10].
The clinical syndrome of Acute-on-chronic liver failure was defined according to the European Association for the Study of the Liver–Chronic Liver Failure (EASL-CLIF) Consortium, which defines Acute-on-chronic liver failure as a clinical syndrome that encompasses three major components: Acute decompensation (inclusion criterion, present in all patients), organ failure (predefined by the SOFA-CLIF score), and high 28-day mortality rate (predefined threshold of 15%) [11]. Patients presenting with the clinical syndrome of acute-on-chronic liver failure tend to exhibit certain unique hemodynamic and inflammatory changes. The high level of nitric oxide (NO) produced in the splanchnic circulation leads to a reduction in the effective circulatory volume, which triggers renal dysfunction in the form of hepatorenal syndrome. On the other hand, severe systemic inflammation and oxidative stress may result in mitochondrial dysfunction and reduced ATP synthesis, culminating in the buildup of lactate as an end-product of anaerobic glycolysis [12]. It may therefore seem intuitive to assume that the high levels of lactate coupled with the loss of albumin due to the impairment of the synthetic hepatic function may give rise to an increased lactate/albumin ratio in patients with advanced cirrhosis and acute-on-chronic liver disease. In this study, we aimed to uncover the clinical significance and provide new insight into the predictive value of these simple and readily available routine serum markers as predictors of adverse events in the setting of hepatic decompensation.
2Materials and methods2.1Setting & designWe conducted a retrospective single-center cohort study in a tertiary medical center in Jerusalem, Israel.
2.2Inclusion and exclusion criteriaIncluded in the study were subjects with an established diagnosis of liver cirrhosis confirmed either histologically or in the setting of compatible clinical, radiological, and laboratory pictures that were admitted to the ICU or the Internal Medicine department with a clinical picture of acute-on-chronic liver failure between the years 2010-2021. Subjects for whom no clear diagnosis of cirrhosis was documented in the medical file or for whom no relevant medical or laboratory data were available were excluded.
2.3Primary & secondary outcomesThe primary outcome of this study was to assess whether the lactate/albumin ratio may be used as a prognostic marker to predict morbidity & mortality in hospitalized cirrhotic patients with acute on chronic hepatic failure. Secondary outcomes included the feasibility of the Lactate/albumin ratio for predicting 30-day mortality and one-year mortality.
2.4Data collectionClinical records of all patients hospitalized between the years 2010-2021 that had cirrhosis were retrieved. Following the extraction of all the relevant data, data was collected including demographic characteristics (age and gender), clinical data (pre-existing medical conditions such as diabetes, hypertension, and chronic kidney disease, the reason for admission, and cirrhosis etiology), laboratory test results (WBC, Platelets, Hemoglobin, Sodium, Potassium, BUN, Creatinine, Bilirubin, Albumin, Alkaline Phosphatase, Aspartate Transaminase (AST), Alanine Transaminase (ALT), Gamma-Glutamyltransferase (GGT), INR, Lactate, MELD Score) and outcomes (death during hospitalization, 30-day mortality, re-admission during one year and death during one year). Biochemistry was measured using the Architect c16000 by Abbot, CBC was measured using the Xe-2100 and XN-2000 by Sysmex, and Coagulation was measured using the ACL Top 800 and ACL Top 500 by Werfen, Lactate was measured using the ABL800 by Radiometer and GEM Premier 5000 by Werfen. All the collected data were then arranged into ad-hoc excel tables.
2.5Timing of Blood tests and the standard of care treatmentAs this study is focused on predicting outcomes in decompensation of cirrhosis (acute on chronic liver failure), the blood tests that were chosen to be collected were those taken during the acute decompensation stage of the patient - defined as the day of admission to the Intensive care unit or admission to the high dependency unit. Routine blood tests including albumin and lactate are performed for all the subjects upon their admission to the intensive care unit/high-dependency unit, in accordance with our institution's protocol. Therefore, and for all the subjects included, the albumin and lactate tests were taken simultaneously.
Upon their admission to the ICU unit, all of the patients were offered the standard of care treatment protocol which is based on early recognition and correction of any underlying decompensation trigger, coupled with invasive monitoring and adequate support for any organ failure.
2.6DefinitionsThe clinical syndrome of Acute-on-chronic liver failure was defined according to the European Association for the Study of the Liver–Chronic Liver Failure (EASL-CLIF) Consortium, which defines Acute-on-chronic liver failure as a clinical syndrome that encompasses three major components: Acute decompensation (defined as the development of ascites, hepatic encephalopathy, gastrointestinal hemorrhage and/or bacterial infection), organ failure (predefined by the SOFA-CLIF score), and high 28-day mortality rate (predefined threshold of 15%). The acute compensation stage of the patient was defined as the day of admission to the Intensive care unit or high dependency unit.
2.7Statistical analysisData was inserted into a Microsoft Excel (version 16.0) spreadsheet and then transferred for analysis to SPSS (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.). Quantitative variables were compared using either the T-Test or the Mann–Whitney test according to variable distribution. For categorical variables, the χ2 test or Fisher's Exact test was similarly chosen. Statistical significance was set at a p-value less than 0.05. To simultaneously assess the effect of several variables (whether quantitative or categorical) on the dichotomous outcome (survival/hospitalization), the multivariate logistic regression model was applied. Lastly, ROC analysis was performed to find an optimal cutoff, based on lactate/albumin values, for achieving the best balance between sensitivity and specificity.
2.8Ethical statementsThe study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution's human research committee. Due to the non-interventional design, the study was granted a waiver from the informed consent by the hospital's ethical committee (Helsinki Committee 0131-21-SZMC). The data was coded to ensure patient confidentiality.
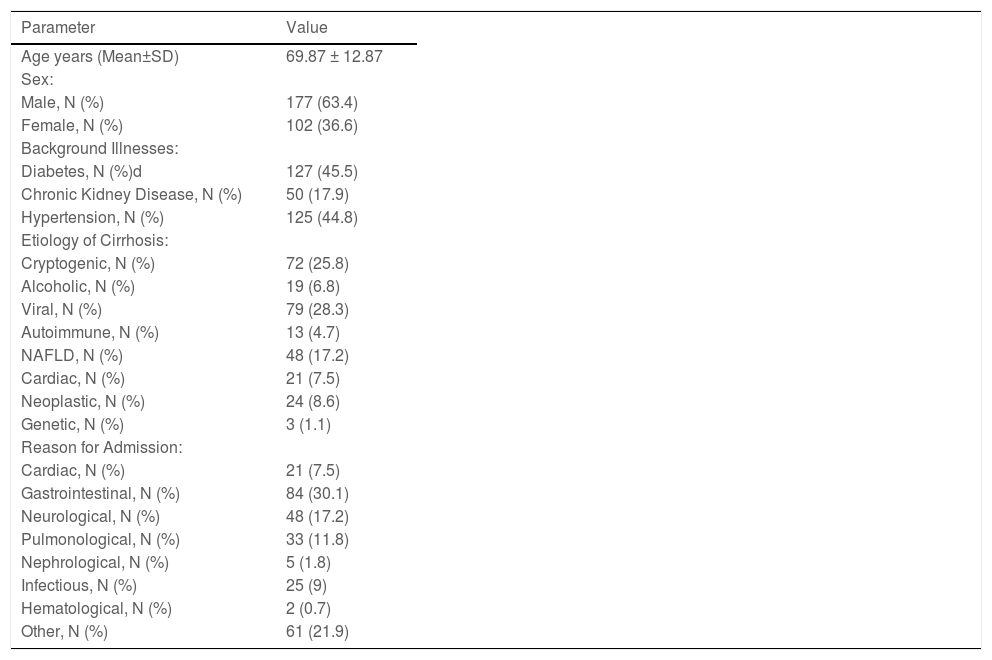
3ResultsTwo hundred seventy-nine patients were hospitalized at our tertiary medical center between the years 2010-2021 with a diagnosis of acute-on-chronic liver failure on the background of cirrhosis. The mean age of the subjects was 69.87 ± 12.87 years, and 177 (63.4%) were males. One hundred and twenty-seven patients were diabetics (45.5%), one hundred and twenty-five patients had hypertension (44.8%) and fifty patients had chronic kidney disease (17.9%) (Table 1). The most common reason for admission was gastroenterological complaints that were reported in 84 (30.1%) of the study subjects. Viral hepatitis was the leading etiology of cirrhosis in our study population (79 subjects (28.3%)), followed closely by cryptogenic cirrhosis (72 subjects (25.8%)) and NAFLD (48 subjects (17.2%)) (Table 1).
Descriptive statistics, etiology of cirrhosis and reason for admission in the study population.
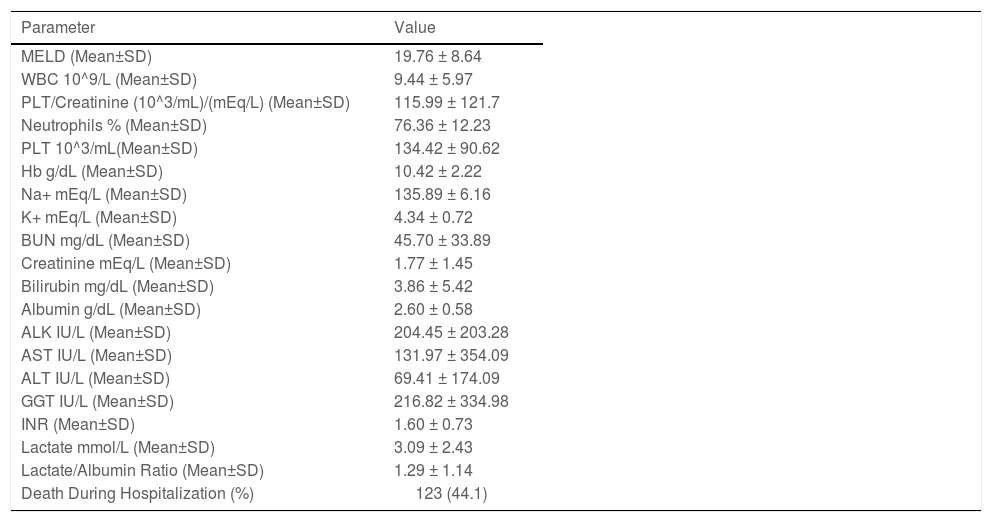
Twenty-four patients (8.6%) had cirrhosis due to secondary neoplastic metastases to the liver. These patients were excluded from the statistical analysis because of their different disease course and their grave prognosis, which could have adversely impacted the primary outcome that we intended to measure (Table 1). The mean MELD score of our study population was 19.76 ± 8.64 with an average serum lactate level of 3.09 ± 2.43 mmol/l and albumin level of 2.60 ± 0.58 g/dl, thus corresponding to a lactate/albumin ratio of 1.29 ± 1.14 for the whole of our study population (Table 2).
Laboratory values in the study population.
NAFLD, Non-Alcoholic Fatty Liver Disease; MELD, Model for End-stage Liver Disease; WBC, White Blood Cell Count: PLT, Platelets; Hb, Hemoglobin; Na+, Sodium; K+, Potassium; BUN, Blood Urea Nitrogen; ALK, Alkaline Phosphatase; AST, Aspartate Transaminase; ALT, Alanine Transaminase; GGT, Gamma-Glutamyltransferase; INR, International Normalized Ratio.
One hundred twenty-three (44.1%) cirrhotic patients with acute-on-chronic liver failure died during hospitalization. The mean lactate/albumin ratio was significantly higher among subjects who died during hospitalization (1.796 ± 1.42) compared to patients who survived until discharge (0.9 ± 0.7) (p < 0.001). In addition, the lactate/albumin ratio was higher statistically among patients that died within 30 days of their hospitalization: (1.1 ± 0.4) as opposed to patients that survived past 30 days (0.89 ± 0.71) (N = 9, p = 0.03). However, no statistically significant difference in the mean lactate/albumin ratio was seen when applied to patients who died within one year (N = 43, p = 0.249) from the index hospitalization (Fig. 1). Similarly, sex (p = 0.9), diabetes (p = 0.472), chronic kidney disease (p = 0.08), hypertension (0.287), etiology of cirrhosis, and the reason for admission (p = 0.161 and p = 0.4, respectively) were all found to be statistically insignificant pertaining to the outcome of death during hospitalization, therefore proving that the lactate/albumin ratio was an independent prognostic factor on death during hospitalization.
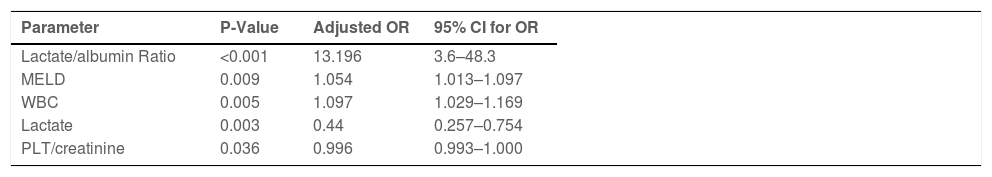
To ascertain the effect of several different variables on the primary outcome, logistic regression was performed in a stepwise fashion. Univariate analysis revealed that mean WBC count, platelet/creatinine ratio, aspartate transaminase AST, lactate, and MELD score were all significantly associated with the primary outcome. Multivariate analysis was then performed and showed that the lactate/albumin ratio was the strongest statistically significant (p < 0.001) predictor of death during hospitalization - OR 13.196 (95% CI 3.6-48.3), followed by mean WBC count, MELD score, and serum lactate levels. (Table 3). Finally, a ROC curve was built, which showed an area under the curve (AUC) equal to 0.77. Crosstabs from the ROC showed a sensitivity of 66.7% and a specificity of 76.2% when the lactate/albumin ratio chosen as a cutoff was 0.90616 – Fig. 2.
Logistic regression, stepwise approach.
MELD, Model for End-stage Liver Disease; WBC, White Blood Cell Count; PLT, Platelets
The main finding of our study is that the lactate/albumin ratio in cirrhotic patients is an independent prognostic factor for mortality during hospitalization. The association was statistically significant even after adjusting for comorbidities, the reason for admission, and the etiology of cirrhosis, thus providing further evidence of the strength of the association. To the best of our knowledge, this is the first report to address this important clinical association in the setting of cirrhotic patients.
Numerous papers in recent years have reported that the lactate/albumin ratio may predict mortality in several different clinical settings. Gharipour et al. found that the lactate/albumin ratio is an early prognostic marker in critically ill patients in the intensive care unit [10], Arroyo et al. reported that the lactate/albumin ratio is a predictor of in-hospital mortality in septic patients presenting to the emergency department [13], Cakir and Turan found that the lactate/albumin ratio was more effective than lactate or albumin alone in predicting outcomes in intensive care patients with sepsis [15], Bou Chebl et al. reported that the lactate/albumin ratio could be used as a prognostic factor in lower respiratory tract infection patients [14].
Our findings may have several important implications. First, the lactate/albumin ratio can be readily measured and easily incorporated into clinical decision-making, which could serve to prioritize patients that may benefit more from intensive care services considering the increased risk of death among this patient population.
Moreover, owing to the objective nature of its two parameters, the lactate/albumin ratio seems to overcome the limitations that are associated with other widely adopted prognostic scoring systems, such as the Child-Pugh score and the MELD score. Originally proposed by Child and Turcotte back in 1964 to predict the prognosis of cirrhotic patients, the CTP score encompasses subjective elements such as ascites and encephalopathy, which are both amenable to subjective assessment of the treating physician and, as such, are prone to human error and lapses in clinical judgment [2,15]. On the other hand, the MELD score seems to function better when employed as an organ allocation tool rather than as a mere prognostic marker [15,16]. This is also implied by the results of the multivariate logistic regression in our study, where the albumin/creatinine ratio correlated better with mortality during hospitalization when compared to the MELD score.
Our results indicate that the lactate/albumin ratio predicts mortality primarily during the acute period of hospitalization (p < 0.001) but fails to predict mortality when the same patient population is followed for one year. We hypothesize that this ratio does not function well as a long-term outcome predictor because a substantial portion of cirrhotic patients develop the final common pathway of liver insufficiency with poor outcomes and high mortality rates, thereby effectively eliminating any effect this ratio may have on mortality. With regard to short-term mortality after the index hospitalization, the lactate/albumin ratio seemed to correlate well with the 30-day mortality (p = 0.03), although the relatively small sample size of patients who died within this specific time window (n = 9) limits our ability to draw any conclusions with absolute certainty. More robust data based on larger populations are needed to confirm whether any possible association does exist.
The univariate analysis also revealed that mean WBC count (p = 0.005), platelet/creatinine ratio (p = 0.036), lactate (p = 0.003), and MELD score (p = 0.009) were all significantly associated with mortality during hospitalization. These findings are in line with what was reported elsewhere in the literature: Wiesner et al. found that leucocyte ratios are biomarkers of mortality in patients with acute decompensation of cirrhosis and acute-on-chronic liver failure [17], Tas et al. reported that lactate levels improve the prediction of short-term mortality in critically ill patients with cirrhosis [8], Christensen found that lactate levels predict 6-months mortality in patients with hepatitis B virus-related decompensated Cholongitas and Burroughs conducted a meta-analysis study that showed the high diagnostic accuracy of the MELD score as a prognostic tool in acute on chronic liver failure [2,18]. Of note, the platelet/creatinine ratio was proposed during this study as a novel ratio that may help predict the outcome of cirrhotic patients in the future. Larger prospective trials are needed to fully understand the significance of this ratio.
Lastly, a ROC curve was constructed to evaluate the sensitivity and specificity of our model to predict mortality during hospitalization in cirrhotic patients using the lactate/albumin ratio. The AUC was 0.77 (95% CI, 0.712-0.828). When crosstabs were chosen from the ROC at lactate/albumin ratio = 0.90616, a sensitivity of 66.7% and a specificity of 76.2% were achieved. These results are comparable to those of the well-established prediction models of the MELD score and the CLIF-C OF score [19,20]. A study conducted by Kamath PS et al. reported a MELD score with an AUC of 0.78 for a 3-month mortality prediction (95% CI 0.74-0.81) [21]. Marroni CP et al. found that the MELD score had an AUC of 0.79 (95% CI 0.72-0.87) when predicting three- and six-month mortality in cirrhotic patients on the waiting list for liver transplantation [22]. In contrast, the AUC for the CLIF-C OF score for predicting 28-day mortality among Portuguese ACLF patients was 0.844 [23].
Our study has several limitations – namely, the retrospective single-center design, which limits the generalizability of the conclusions. The acute decompensation stage of the patient's hospitalization (defined as the day of admission to the intensive care unit) may have been difficult to identify precisely and as such, it may not be necessarily reflective of the point of maximal hepatic decompensation. This may have precluded the use of single-serum sample lactate as a marker for decompensation and in that sense, it could be argued that the average serum lactate level during hospitalization might have been a more reliable marker of hepatic decompensation. Furthermore, serum lactate and albumin might have been affected by the condition of the patients before the institution of treatment or by medical therapy (such as albumin infusion for hepatorenal syndrome or following large-volume paracentesis). This explains, at least in part, the modest sensitivity and specificity of our prediction model and highlights the need for future prospective studies to confirm the validity of our findings. Finally, a small proportion of patients may have also been referred to other healthcare institutions following their index hospitalization, thus rendering the data on their outcomes potentially inaccessible, which could potentially influence their secondary outcomes of 30-day and 1-year mortality. However, many of the patients were known to our liver clinic and internal medicine wards and, as such, were more likely to present to our hospital rather than other healthcare facilities.
On the other hand, the obvious strengths of our study are the relatively large sample size of a cirrhotic patient population with different etiologies, including less abundant etiologies (such as alpha1-antitrypsin deficiency), which closely reflects the real-world population of cirrhotic patients. The albumin/creatinine ratio was examined using three different statistical models: the t-test, logistic regression, and ROC curve, therefore providing a sound methodological basis for the performance of the prediction model and the conclusions inferred from it.
Lastly, our model enables the prediction of clinical outcomes in a very feasible and objective way using readily available standard blood tests to help identify patients that are at an increased risk of adverse outcomes.
5ConclusionsIn conclusion, the lactate/albumin ratio was found to be an independent predictor of in-hospital mortality of cirrhotic patients. Future research should include prospective multicentric studies to examine the applicability of our findings to broader clinical settings.
Data availability statementAvailable from the corresponding author upon request.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of interestNone.
Author contributionsItamar Krispin: Conceptualization, Methodology, Formal analysis, Data curation, Writing – original draft. Mahmud Mahamid: Conceptualization, Methodology, Writing – review & editing. Eran Goldin: Conceptualization, Methodology, Writing – review & editing. Bashar Fteiha: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Formal analysis, Supervision.