Fever of intermediate duration (FID) is a common condition. Currently, its most frequent causes are not well defined.
MethodsProspective study of FID cases attended at a hospital in 2 periods: 1983–1989 and 2004–2005. Blood cultures and serologic studies for Brucella melitensis, Coxiella burnetii, Rickettsia typhi, Rickettsia conorii, cytomegalovirus, and Epstein-Barr virus were performed on all patients. Other microbiological, serological, radiological, or invasive procedures were performed according to clinician-in-charge criteria.
ResultsA total of 505 patients were included from 1983 to 1989, and 179 from 2004 to 2005. A diagnosis was reached in 410 (81.1%) and 109 patients (60.9%), respectively. The cause of FID was an infectious disease in 389 patients from the first period (94.8% of those with a final diagnosis) and 92 from the second (84.4%). Most were systemic infections, 328 (80%) in 1983–1989 and 74 (67.8%) in 2004–2005, followed by focal infections, 9.5% and 16.5%, respectively. Q fever was the most frequent etiology in both periods. In 2004–2005, brucellosis decreased and HIV infection emerged as a cause of FID. The origin of FID was non-infectious in 5.1% and 15.5%, respectively.
ConclusionsQ fever is the most frequent cause of FID in southern Spain. Studies over time are needed to identify changes in the etiologic spectrum of this condition. Important viral etiologies, such as HIV infection, may be detected as causes of FID. Further studies are needed to determine the importance of other agents as causes of FID.
La fiebre de duración intermedia (FDI) es una causa importante de fiebre. Las etiologías más importantes no están bien definidas en la actualidad.
MétodosEstudio prospectivo de los casos de FDI atendidos entre 1983–1989 y 2004–2005. Se realizaron cultivos y estudios serológicos para la detección de Brucella melitensis, Coxiella burnetii, Rickettsia typhi, Rickettsia conorii, citomegalovirus y virus de Epstein-Barr en todos los pacientes. Se llevaron a cabo otros estudios microbiológicos, serológicos, radiológicos y pruebas invasivas adicionales según el criterio del clínico responsable.
ResultadosEn el periodo de 1983 a 1989 se incluyeron 505 pacientes y 179 desde 2004 a 2005. Se alcanzó un diagnóstico etiológico en 410 (81,1%) y 109 (60,9%), respectivamente. La causa de FDI fue infecciosa en 389 pacientes del primer periodo (94,8% del total de pacientes con diagnóstico etiológico) y 92 del segundo (84,4%). La mayoría fueron infecciones sistémicas, 328 (80%) en 1983–1989 y 74 (67,8%) en 2004–2005, seguidas de infecciones focales, 9,5% y 16,5%, respectivamente. La fiebre Q fue la etiología más frecuente en ambos periodos. En 2004–2005, la brucelosis disminuyó mientras que la infección por el VIH se mostró como una causa emergente de FDI. El origen de la FDI fue no infeccioso en el 5,1% y el 15,5% de los casos, respectivamente.
ConclusionesLa fiebre Q es la causa más frecuente de FDI en el sur de España. Son necesarios estudios prospectivos más amplios para identificar los cambios en el espectro etiológico de esta entidad. Infecciones virales, como la infección por el VIH, deben ser contempladas como causa de FDI.
Community-acquired fever without a focal condition is frequent in clinical practice. Medical management of this syndrome is based mainly on fever duration. Along this line, there are 3 chronologically distinct types of fever: first, fever of short duration, lasting up to 7 days, is usually due to self-limiting systemic viral infections; the diagnostic and therapeutic approach to this entity is well defined;1 second, classic fever of unknown origin (FUO), for which the concept, epidemiology, most frequent etiologies, and diagnostic and therapeutic approaches have been extensively evaluated by many authors in several geographic, historic, and population contexts;2–4 and third, fever higher than 38°C lasting 7 to 28 days that remains undiagnosed or has associated findings that prompt a diagnostic procedure after performing the patient's history, physical examination, hemogram, serum creatinine determination, urine analysis, and chest radiograph, defined as fever of intermediate duration (FID). This condition has recently been considered a separate syndrome, and constitutes an entity with well-defined etiological features.5 After various prospective clinical and epidemiological analyses were carried out in southern Spain, an overall diagnostic strategy and empirical treatment for FID was proposed.6,7
Nonetheless, over the past few years, certain changes in the incidence of community-acquired infections that were frequent causes of FID have occurred in Spain. One significant example is that the incidence of brucellosis has decreased from 22 cases/100,000 inhabitants in 1984 to 1.7 cases/100,000 inhabitants in 2006.8,9 Furthermore, new pathogens/diseases may have emerged in the past years and established efficient life cycles in human populations. Lastly, we know that ecological, socioeconomic and health conditions change over time, and these variations can result in potential changes in the emergence-reemergence of endemic infections, and therefore, in the etiological spectrum of FID. Despite these facts, current studies that focus specifically on possible changes in the etiological patterns of FID over time are lacking.
The aim of the present study was to evaluate the etiologies of FID in southern Spain in a prospective study carried out between 2004 and 2005 and compare them with those found in a methodologically similar study performed between 1983 and 1989 in the same geographic area. The study was designed to assess possible changes that would prompt us to redefine the best diagnostic approach and empirical treatment of this common condition.
MethodsSetting: Two prospective studies were carried out in 1983–1989 and 2004–2005 to determine the etiology of FID in patients attended in the Infectious Diseases Department of Virgen del Rocío University Hospital in Seville, southern Spain. Virgen del Rocío is a tertiary hospital that attended a population of 881,454 and 973,200 inhabitants, respectively, in each period, mostly from urban areas (60% and 65%, respectively).
Inclusion Criteria: All patients older than 14 years with the following FID criteria were included: 1) fever higher than 38°C, with no apparent cause and lasting between 1 and 4 weeks; 2) no previous hospital admission or health care-related attention10 and no underlying immunodeficiency or chronic disease that could cause fever; and 3) no diagnosis following an initial approach, including clinical evaluation, hemogram, urinary sedimentation study, serum creatinine determination and chest radiography. All patients with known HIV infection, intravenous drug users (IDUs), immigrants that had resided for less than one continuous year in Spain, and persons who had traveled internationally in the previous 6 months were excluded.
Study protocol and variables: A basic evaluation was performed on all patients. The following data were recorded: demographic and epidemiological data, date on the onset of fever, patient from rural or urban areas, medical history, and results of a thorough physical examination. In addition to the analyses included in the definition, the erythrocyte sedimentation rate (ESR), and alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (AP), and bilirubin levels were determined.
Urine cultures were performed and blood cultures (2 samples separated by 30min, aerobic and anaerobic vials, BACTEC) if the patient had fever higher than 38°C initially. The following serologic studies were performed (acute and convalescent phases): 1) Brucella melitensis: Rose of Bengal (bioMérieux, Lyon, France) and immunofluorescence assay (IFA) (Vitaltech, Sant Cugat, Barcelona, Spain) for quantified IgG and IgM (Bio-Rad, Paris, France), previous inactivation of IgG and rheumatoid factor with Gull-sorb (Meridian, Cincinnati, Ohio, USA); 2) Coxiella burnetii, IFA (Virion, Richland, USA in 1983–1989 and Vitaltech in 2004–2005); 3) Rickettsia typhi and Rickettsia Conorii, IgG IFA (Pasteur Laboratories, Marnes, la Coquette, France until 1986 and bioMérieux from 1987); 4) cytomegalovirus (CMV), complement fixation (Virion in 1983–1989) and enzyme-linked immunosorbent assay (ELISA IgG and IgM, Dade Behring, Barcelona, Spain in 2004–2005), the positive IgM being confirmed by IFA (Meridian); and 5) Epstein-Barr virus, IFA (Meridian in 1983–1989) and chemiluminescence (IgG and IgM, DiaSorin, Vercelli, Italy in 2004–2005) confirmed by IFA (Meridian, IgG e IgM). In the first period of the study (1983–1989) serology for Leptospira spp. by IFA (Difco Laboratories, Sparks, USA) was carried out in all cases.
Other laboratory studies were also performed, depending on the clinical features of the patient: 1) auramine-rhodamine staining of sputum and urine cultures for mycobacteria; 2) thyroid-stimulating hormone and free thyroxine; 3) serology for parvovirus B19 in the second period (IFA IgM, Biotrin, Lyon, France); 4) Toxoplasma gondii IFA (BioMerièux) and IgG and IgM by ELISA (Dade Behring) in the 2 periods, respectively; 5) HIV by ELISA (Dade Behring) and Western blot (New lav Blot 1, Bio-Rad); and 6) syphilis by quantitative RPR (Biosystems, Foster City, USA) and FTA ABs-IgG and IgM (Bio Mèrieux).
All patients were followed-up for at least 1 month after the first visit and until cure, progression to FUO, or death. At the end of follow-up, the definitive diagnosis and hospital admission information were collected.
Statistical analysis: A descriptive analysis was carried out using the Epi-Info and SPSS 13.0 statistical packages.
ResultsA total of 505 patients were included in the first period (1983–1989) and 179 in the second (2004–05), with a median age of 32.6±17.4 and 39.7±15.8 years, respectively. In both periods, there was a predominance of males: 404 (80%) in the first and 117 (65.4%) in the second.
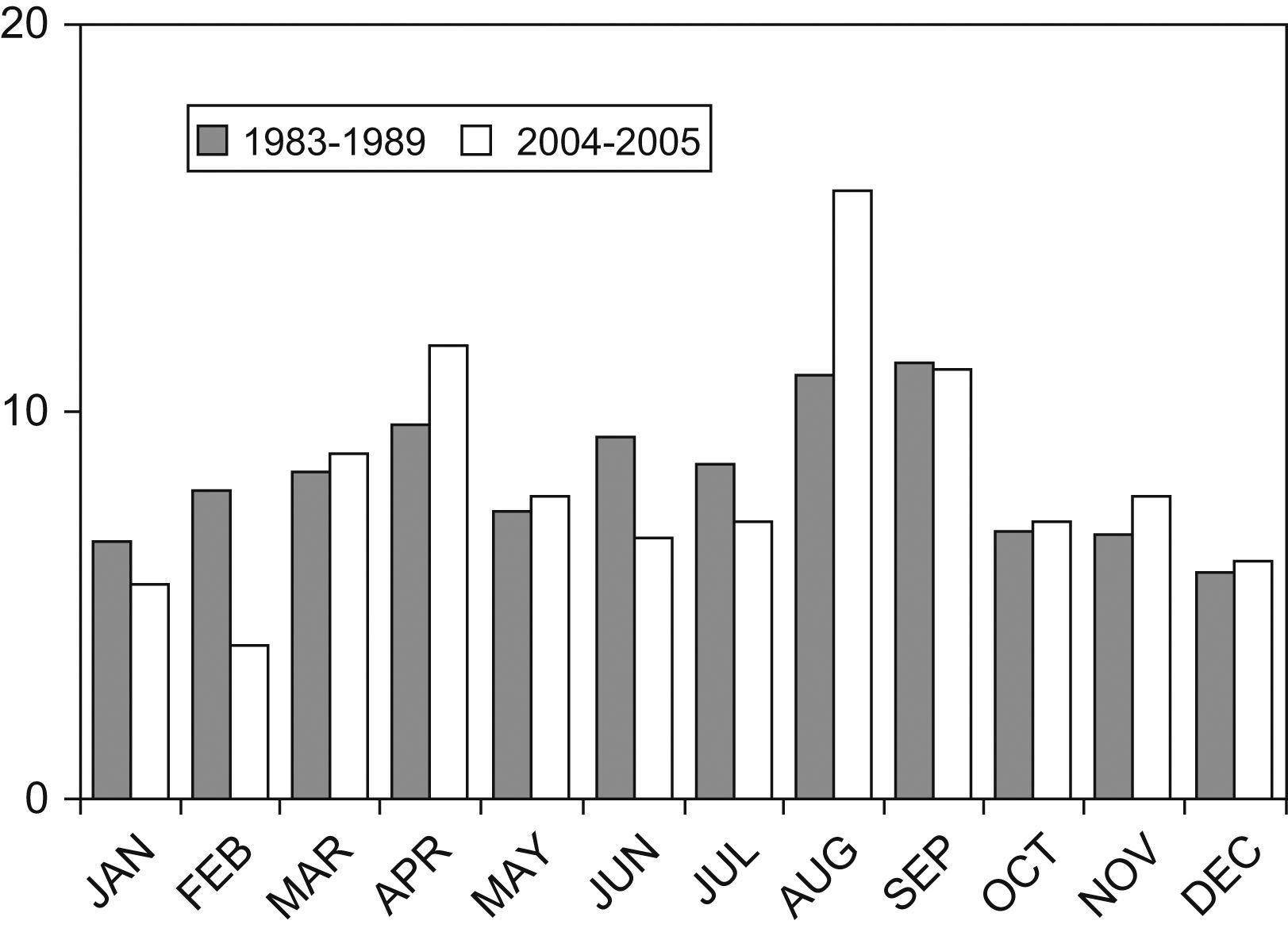
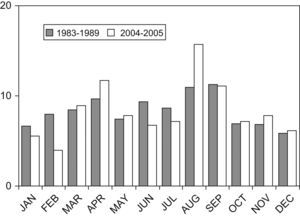
The monthly distribution showed a higher incidence of cases between March and November (479 [94.8%] in the first period and 138 [77.1%] in the second) (Fig. 1). In the first period, 42.9% of patients lived in urban areas, and in the second, 57%.
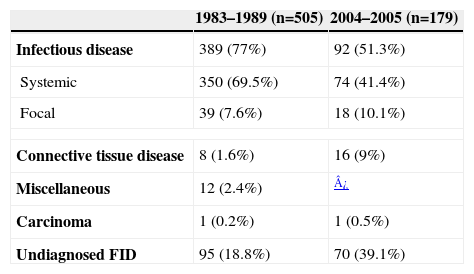
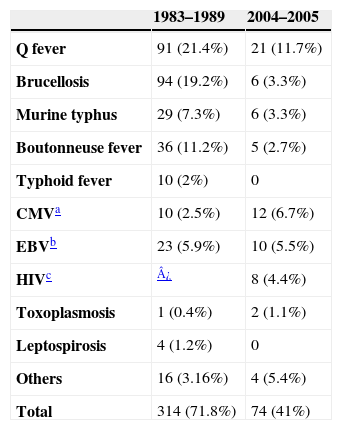
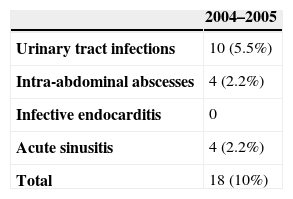
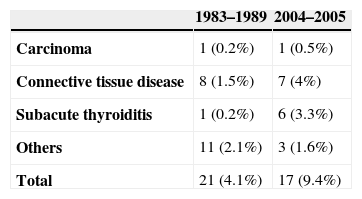
An etiologic diagnosis was attained in 410 patients (81.1%) in the first study and 109 patients (60.9%) in the second study, whereas in 95 (18.8%) and 70 (39.1%) cases, respectively, fever resolved without determining the cause, despite completion of the diagnostic workup (Table 1). The cause of fever was an infectious disease in 389 patients from the first period (77% of the total and 94.8% of those with a final diagnosis) and 92 patients from the second (51.3% and 84.4%, respectively). Most were systemic infections, with 328 cases in the first period (65% and 80%) and 74 cases in the second (41.3% and 67.8%) (Table 2), followed by focal infections, with 39 cases in the first period (7.7% and 9.5%) and 18 cases in the second (10% and 16.5%) (Table 3). The origin of FID was a noninfectious cause in 21 cases (4.1% and 5.1%) in the first period and 17 cases (9.4% and 15.5%) in the second (Table 4).
Etiologies of fever of intermediate duration (FID) in the two periods of the study
| 1983–1989 (n=505) | 2004–2005 (n=179) | |
| Infectious disease | 389 (77%) | 92 (51.3%) |
| Systemic | 350 (69.5%) | 74 (41.4%) |
| Focal | 39 (7.6%) | 18 (10.1%) |
| Connective tissue disease | 8 (1.6%) | 16 (9%) |
| Miscellaneous | 12 (2.4%) | ¿ |
| Carcinoma | 1 (0.2%) | 1 (0.5%) |
| Undiagnosed FID | 95 (18.8%) | 70 (39.1%) |
Systemic infections as cause of fever of intermediate duration in the two periods of the study
| 1983–1989 | 2004–2005 | |
| Q fever | 91 (21.4%) | 21 (11.7%) |
| Brucellosis | 94 (19.2%) | 6 (3.3%) |
| Murine typhus | 29 (7.3%) | 6 (3.3%) |
| Boutonneuse fever | 36 (11.2%) | 5 (2.7%) |
| Typhoid fever | 10 (2%) | 0 |
| CMVa | 10 (2.5%) | 12 (6.7%) |
| EBVb | 23 (5.9%) | 10 (5.5%) |
| HIVc | ¿ | 8 (4.4%) |
| Toxoplasmosis | 1 (0.4%) | 2 (1.1%) |
| Leptospirosis | 4 (1.2%) | 0 |
| Others | 16 (3.16%) | 4 (5.4%) |
| Total | 314 (71.8%) | 74 (41%) |
Diseases other than infectious disease as a cause of fever of intermediate duration in the two periods of the study
| 1983–1989 | 2004–2005 | |
| Carcinoma | 1 (0.2%) | 1 (0.5%) |
| Connective tissue disease | 8 (1.5%) | 7 (4%) |
| Subacute thyroiditis | 1 (0.2%) | 6 (3.3%) |
| Others | 11 (2.1%) | 3 (1.6%) |
| Total | 21 (4.1%) | 17 (9.4%) |
Among the 95 and the 70 patients from each period without an etiologic diagnosis, 63 (67.7%) and 53 (76%), respectively, received empiric antibiotic treatment. Doxycycline was the empiric treatment in 100% and 86%. The remaining empiric treatments (14% in the second period) consisted of amoxicillin/clavulanate, fluorquinolones, or ceftriaxone.
In the first period, 25 patients (4.9% of the total) and in the second, 3 patients (1.6%) progressed to FUO during follow-up. The etiologies of FUO in the first period were systemic infections in 9 (1.7% of the total and 36% in this group), focal infections in 3 (0.5% and 12%, respectively), connective tissue diseases in 3 (0.5% and 12%), others in 2 (0.4% and 8%), and no final diagnosis was reached in 8 patients (1.5% and 32%). The final diagnoses in the 3 patients who progressed to FUO in the second period were Still disease, rheumatic polymyalgia, and temporal arteritis, respectively.
During the first period, 301 patients (59.6%) were admitted to the hospital and 67% of these were patients who came from areas far from the hospital. During the second period, 19 patients (11%) were admitted to the hospital, in 2 cases because of severe clinical criteria, including Staphylococcus hominis bacteremia with severe sepsis, and gastrointestinal hemorrhage, respectively.
No patient died in the first period during the month after the initial visit. One patient (1.2%) died in the second period because of a gastric carcinoma with hepatic metastasis that manifested initially as FID.
DiscussionFever of intermediate duration is a common occurrence that results in a large number of medical consultations. As was seen in both study periods, a high percentage of cases are due to acute systemic infectious diseases, which are treatable and have a good prognosis in terms of survival rates, and in which, appropriate systematic medical attention for the diagnosis and treatment enables outpatient care in many cases.
The comparison of etiologies found in the 2 periods revealed considerable changes in the etiological spectrum of FID. Though the main causes are still systemic infections, mainly Q fever, the decrease of brucellosis is significant: 19% of the causes of FID between 1983 and 1989, in comparison with 3% between 2004 and 2005, probably due to Brucella eradication campaigns in Andalusian livestock, with the consequent decrease in the incidence of this disease in our country.8 Moreover, we observed an increase in the number of FID cases caused by viral infections (17.3% in 2004–2005 vs. 6.5% in 1983–1989), highlighting herpes virus and acute HIV infection, which were not registered in the first period, despite the emergence of the pandemic of HIV infection at the beginning of this period. This fact suggests that a high level of suspicion is required to detect HIV-related FID.
A substantial percentage of cases in the second period (39.1%) had no etiological diagnosis after undergoing a systematic approach, a higher value than that observed in the first period (18.9%). This may be secondary to changes in the organization of health management for patients with FID in Andalusia (the southernmost region of Spain) and in our area in 20037, which prompted a coordinated effort by primary care physicians and infectious disease physicians in the hospital. In this organizational change, the initial care of patients with FID is referred to the primary care level, with the recommendation of empiric treatment with doxycycline. This healthcare measure suggests that a number of patients with rickettsiosis and Q fever as the cause of FID would be cured without the need for hospital treatment and without requiring an etiologic diagnosis. Although the low rate of rickettsiosis and Q fever among the etiologies of FID in the latter period of the present study may question the use of doxycycline as empiric treatment for this condition, we believe it remains a useful option for this purpose because of its suggested efficacy at the primary care level. The high percentage of patients that remain undiagnosed in the hospital suggests that new serologic studies should be included in the systematic approach we are currently using, in order to detect other etiologies.
Another difference to highlight between the 2 periods studied is the number of patients admitted to the hospital, 59.6% vs. 11%, respectively. This decrease in the second period results from the fact that the prognosis of FID was proven to be benign after the first study and to the aforementioned healthcare changes for patients with FID.
The most likely cause for the significant rate of undiagnosed cases of FID in the second period may be systemic infections, since more than half the cases were limited with empirical doxycycline treatment and the remaining ones were self-limited. Rickettsia spp., especially R. felis, could explain the etiology of a small percentage of FID limited with doxycycline. This new Rickettsia sp., which belongs to the spotted fevers group, was discovered a few years ago in cats and other peridomestic animals, as well as in their parasites, and it results in clinical manifestations and serological findings that cannot be distinguished from those of murine typhus.11,16 The pathogenic role of this species in humans was initially proved in California, but isolated cases have also been recently reported in Western Europe.13,16 In our area, it has been detected in fleas belonging to the Ctenocephalides felis species and living on domestic and peridomestic mammals in western Andalusia.14 Moreover, infectious titers were recently discovered in human populations (6.5%) pertaining to the same area.15 Thus, it is possible that an undetermined number of FID cases may have been caused by this pathogen. The same may be said regarding Rickettsia Bar29, described in northern Spain and closely related to Rickettsia massiliae, which transmits to humans through Rhipicephalus sanguineus ticks. Infectious titers have recently been detected within the western Andalusian population (3.4%); hence, it can be considered a possible cause of FID.16,17 Other Rickettsia spp. have been recently described as a cause of fever with or without rash in Spain, which suggests that they may also be the cause of some cases of FID.18,20
Other pathogens with an etiological capacity to cause FID considering epidemiological concordance (proved or probable existence in our area), clinical symptoms, and response to doxycycline or self-limitation are Anaplasma phagocytophilum,21 endemic recurrent fever caused by Borrelia hispanica,22Legionella pneumophila (Pontiac fever),23 and acute infections due to Leishmania infantum.24 The presence of all of these pathogens has been proven in hosts and vectors in our environment and in aquatic environments related to human presence. Moreover, they have all caused illness in subjects from our geographic area, producing symptoms in immunocompetent patients in which fever may be the only manifestation or the predominant one. Then, they may be self-limiting or be treated with doxycycline.11–24
Finally, the moderate but significant viral etiologies of FID in the second period lead us to believe that other viruses, such as human herpes virus type 6 or B19 parvovirus, which are not commonly included in the diagnostic evaluation of FID, could produce an indeterminate number of cases.
The number of studies analyzing the etiologies of FID or short-duration fever is limited.25,26 A recent retrospective study of the etiologies of FID, carried out between 2000 and 2005, in Granada (Spain) identified the cause of FID in only 80 of 233 patients (34.3%), a much lower percentage than that found in our study (60.9%). The retrospective design of the study25 and the small number of etiologies systematically included in the diagnosis of the participating patients may explain the low number of etiologic diagnoses reached. This fact reduces the value of comparisons between the results of that study and the present one. However, Q fever remains the first cause of FID in both studies. In addition, no fatal cases were found,25 in keeping with the low mortality rate in the present study.
Other authors have analyzed the etiology of acute undifferentiated febrile illness in Thailand26 in a prospective hospital-based study. Children older than 3 years and adults with a febrile illness lasting 3 to 14 days were included. These criteria differ from those used in our study, which was carried out with older patients who had fever lasting 7 to 28 days. Once again, the etiology of the fever was found in only 38.7% of the cases. Among the more frequent etiologies was rickettsiosis (scrub typhus and murine typhus), a consequence of the different epidemiological spectrums from separate geographical areas. The mortality rate was also low, at 1.1%. Although the comparison between that study26 and the present one is difficult, taking into account the different inclusion criteria of febrile patients with regard to fever duration and age, the data from both studies stress the importance of determining the etiology of febrile illnesses that do not fulfill the criteria of FUO to establish a standardized protocol of management for these patients.
Thus, broader prospective research in different geographical areas should be performed to help establish the etiologies of FID and the consequent clinical and diagnostic approach and initial empiric treatment of patients with this condition. It might also be interesting, from a global heath perspective, to redirect preventive strategies in an epidemiological and public health dimension.
In summary, results from the 2 periods included in this study show that systemic infections (mainly Q fever in our geographic area) are the main cause of FID. Second, the studies performed during different periods have enabled us to observe etiologic changes resulting from variations in the prevalence of specific diseases, brucellosis being an example in the present study. In addition, important viral etiologies, such as acute HIV infection, can be detected through the standardized approach to the management of patients with FID. Lastly, further studies are needed to determine the importance of other agents as causes of this condition.
This study was funded in part by a research grant from the Ministry of Science and Innovation, Instituto de Salud Carlos III-FEDER, and Red Española de Investigación en Patología Infecciosa (REIPI RD06/0008).