Background/Objectives: Binge Eating Disorder (BED) is often associated with obesity. In order to identify the variables that allow to better detect the presence of BED, people with overnutrition were compared with and without BED in the presence of cognitive conflicts, eating symptoms and anxious-depressive symptoms. The inclusion of cognitive conflicts had been relevant in bulimia studies but had not been investigated with respect to BED. Method: Two groups with obesity were evaluated, one without BED (OB, n=54) and the other with BED (OB-BED, n=48), using a social-demographic questionnaire as well as a semi-structured interview to assess BED, questionnaires (DASS-21, EDE-Q, EEQ) and the Repertory Grid Technique. Results: Overall, the OB-BED group presented more conflicts and more symptoms. The model that best differentiated between the groups included emotional eating and level of cognitive conflicts, correctly classifying 91.4% of the sample. Conclusion: These results highlight the role played by cognitive conflicts and emotional eating as differentiating elements between OB and OB-BED, with a high level of predictive accuracy.
Antecedentes/Objetivos: El trastorno por Atracón (TA) es un trastorno de la conducta alimentaria asociado frecuentemente con la obesidad. Con el objetivo de identificar las variables que permiten detectar mejor la presencia de TA se compararon personas con malnutrición por exceso con y sin TA respecto a la presencia de conflictos cognitivos, sintomatología alimentaria y sintomatología ansioso-depresiva. La inclusión de los conflictos cognitivos había resultado relevante en estudios con bulimia pero no habían sido investigados con respecto al TA. Método: Se evaluó a dos grupos con obesidad, uno sin TA (OB, n=54) y otro con TA (OBTA, n=48), utilizando un cuestionario sociodemográfico, una entrevista semiestructurada para evaluar TA, cuestionarios (DASS-21, EDE-Q, EEQ) y la Técnica de la Rejilla. Se realizaron análisis de comparación de grupos y de regresión logística. Resultados: El grupo OBTA presentó más conflictos y más sintomatología. El modelo que mejor diferenció entre los grupos incluyó la alimentación emocional y el nivel de conflictos cognitivos, clasificando correctamente al 91,4% de la muestra. Conclusiones: Estos resultados resaltan el rol que juegan los conflictos cognitivos y la alimentación emocional como aspectos diferenciadores entre OB y OBTA, con un alto nivel de precisión predictiva.
Overweight and obesity have become a serious problem worldwide, and Spain is no exception. The World Health Organization (WHO, 2015) estimates that approximately 1900 million adults across the world now have a higher than normal body mass index (BMI), while data for Spain suggest that around half the population aged over 18 are at least overweight (Instituto Nacional de Estadística, 2016). These are worrying figures, since obesity is directly linked to medical, psychological, and social problems. As a phenomenon it, therefore, requires a multidisciplinary approach.
Relevant to the psychological perspective is the fact that obesity is often comorbid with binge eating disorder (BED), which is estimated to be present in between 30% and 50% of people who seek weight-loss treatment for obesity (Spitzer et al., 1992; Vinai et al., 2015). This disorder is characterized by the regular occurrence of binges, defined as an excessive intake of food associated with a sense of loss of control (American Psychiatric Association, APA, 2013).
Although obesity itself is associated with psychiatric comorbidity (Baile & González, 2011), the presence of binges makes it more likely that forms of psychopathology other than BED will also be present, the most common being affective and anxiety disorders (Escandón-Nagel, 2016; Klatzkin, Gaffney, Cyrus, Bigus, & Brownley, 2015).
Binges appear to be triggered by a breakdown in emotion regulation, such that food itself becomes a regulator, even though no substantial and stable improvement in mood occurs after the binge episode (Munsch, Meyer, Quartier, & Wilhelm, 2012). The phenomenon of overeating in response to unpleasant emotions has been referred to as ‘emotional eating’ (Ganley, 1989), and it tends to occur more often in obese individuals with BED than in those without such comorbidity (Leehr et al., 2015).
Despite being a relatively common problem in the context of obesity, less than half of individuals with BED receive treatment (Kessler et al., 2013), perhaps due to a lack of awareness of this disorder. It is worth noting that although obesity itself is not formally classified as an eating disorder, some studies (Ugazio, Negri, & Fellin, 2015) have blurred the distinction, as if it were indirectly synonymous with BED, thereby highlighting the lack of diagnostic clarity. However, as Castiglioni, Pepe, Gandino, and Veronese (2013) point out, although obesity and BED are related, the differences and similarities in the psychological processes that underpin them are yet to be clearly understood, this being a question that requires a doubling of research efforts.
A further and related issue, highlighted by Tanofsky-Kraff et al. (2013), is that the majority of studies to date have been conducted within independent fields, either from the perspective of eating disorders or in the context of research on obesity, and hence there is a need for studies that integrate the two lines. The present study focuses precisely on the twin aspects of obesity and BED, and also considers the notion of internal or cognitive conflict, a concept used frequently in psychology when describing the various elements that influence behaviour, but which has been overlooked in many studies of the psychological factors underpinning eating disorders, probably due to the difficulty of measuring it. In this context, personal construct theory (PCT) offers both an operational definition of cognitive conflicts (Feixas, Saúl, & Ávila-Espada, 2009) and a tool for measuring them - the Repertory Grid Technique (RGT).
Underlying PCT is the metaphor of the scientist, the idea being that each person develops implicit hypotheses about the self and the world which are then subjected to continuous testing (mostly without the person being aware of doing so). If these hypotheses serve to predict events then they are functional, but otherwise they should be revised. Hypotheses of this kind are comprised of personal constructs, defined as bipolar abstractions or attributes that individuals use to discriminate between things, events, or people. The person usually regards one of the two poles as being more desirable (Botella & Feixas, 1998).
A useful tool for understanding a person's system of constructs is the RGT, which can yield several indices, including two main types of cognitive conflict: dilemmatic constructs and implicative dilemmas (Feixas & Saúl, 2004). The former refer to those constructs that do not offer a clear course of action, since both poles of the construct are deemed undesirable by the individual, who therefore finds it difficult to choose between them. A person who experiences numerous dilemmatic constructs may enter a state of insecurity, doubt, and inaction (Feixas & Saúl, 2004).
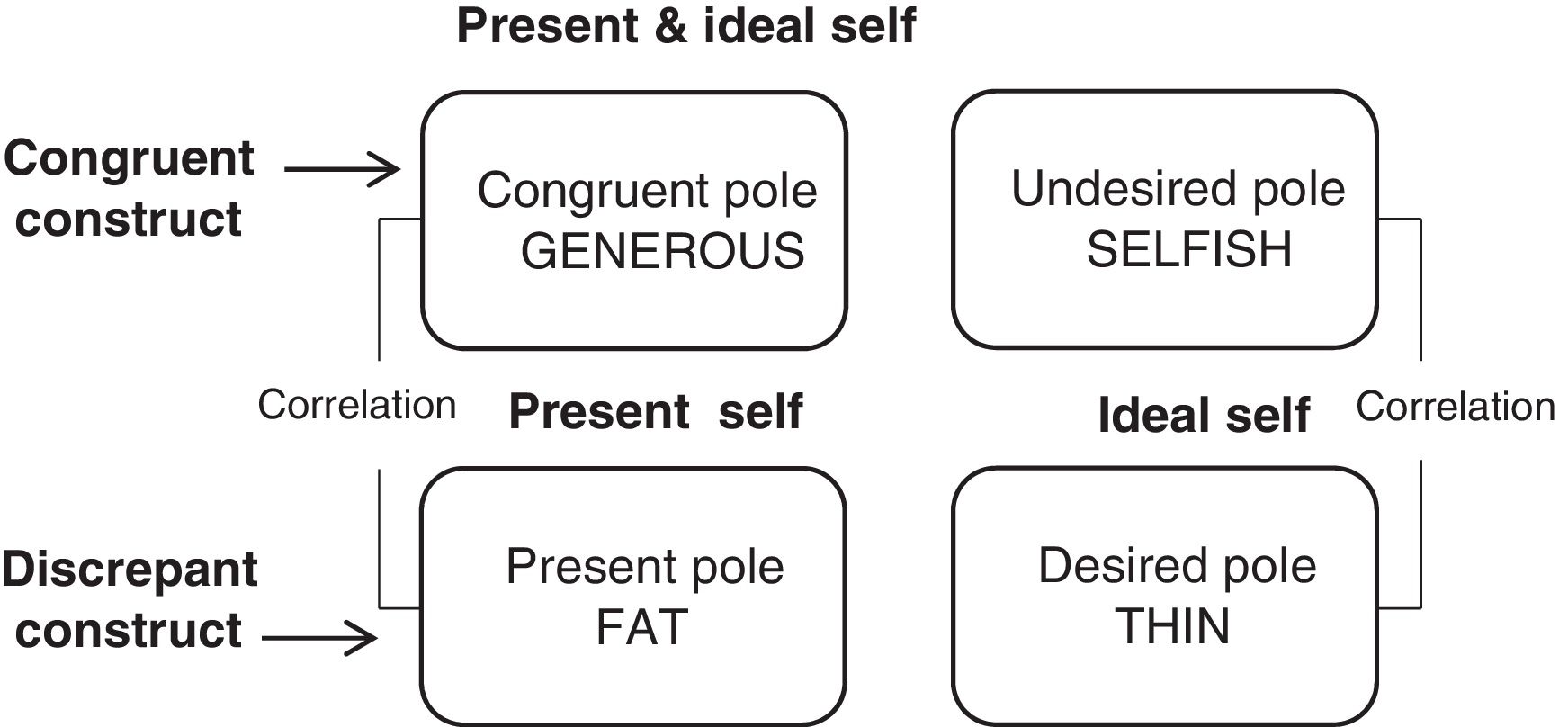
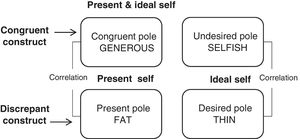
Implicative dilemmas, on the other hand, result from the implicit association between two constructs, one which the individual would like to change (referred to as the discrepant construct) and another which the person values as positive (congruent construct). The ratings given to these two constructs may correlate in a way such that acquiring the desired attribute (in the discrepant construct) implies modifying the position of the self in the congruent construct, a change the person does not wish. Thus, while a person may wish to be rid of a symptom or problem this can be perceived or felt as having negative repercussions in other areas, thus hindering the possibility of change (Feixas & Saúl, 2004). Figure 1 illustrates this through an implicative dilemma experienced by one of the participants in the present study, for whom the conflict arised because the desired change (becoming “thin”) implied a change in a congruent construct (becoming “selfish” instead of “generous”).
According to Feixas, Saúl, and Ávila-Espada (2009), implicative dilemmas are more prevalent among clinical samples. Studies suggest that between 52.1% and 76.7% of clinical subjects experience this kind of conflict, as compared to 33.9-46.7% of non-clinical participants (Compañ et al., 2011; Feixas et al., 2009; Feixas et al., 2014; see, also, the meta-analysis by Montesano, López-González, Saúl, & Feixas, 2015). As for dilemmatic constructs, these were reported to be present in 73.2% of the clinical sample and 66.1% of the non-clinical sample, a difference that was not statistically significant (Feixas et al., 2009).
The aim of the present study is to compare obese individuals, with and without BED, in relation to the presence of cognitive conflicts, eating disorder symptoms, emotional eating, and symptoms of anxiety and depression, analysing which of these variables is best able to predict the presence of BED.
MethodParticipantsThis was a non-probabilistic convenience sample gathered from four health care centres in the Barcelona area, as well as through advertisements posted on social media and in public places. Two study groups were formed: obese individuals with BED (OB-BED, n=48) and non-BED obese individuals (OB, n=54). Of participants in the OB-BED group, 60.4% were recruited through the health care centres and 39.6% through public advertisements. The corresponding figures for the OB group were 46.3% and 53.7%, respectively.
In order to be eligible for inclusion, participants had to be aged over 18 and to have a BMI of 27 or higher, a value chosen as it represents the lower bound of the Grade II overweight (pre-obesity) category, as defined by the Spanish Society for the Study of Obesity (Rubio et al., 2007). To ensure that they could understand the assessment instruments used, all participants were required to have at least primary level education and to be competent in Spanish. Potential participants were excluded if they had undergone or had considered undergoing bariatric surgery, as such individuals might present serious psychosocial problems (Baile & González, 2011).
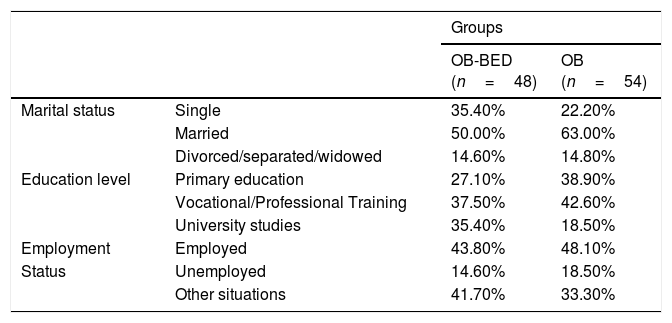
In terms of gender, women accounted for 91.7% of the OB-BED group and 92.6% of the OB group. Mean age was 44.13 years (SD=11.49, range 18-68) in the OB-BED group and 39.46 years (SD=11.93, range 18-58) in the OB group. Mean BMI was 38.51kg/m2 (SD=5.79, range 27.40-50.26) in the OB-BED group and 37.15kg/m2 (SD=6.21, range 27.19-55.84) in the OB group, which in both cases corresponds to type II obesity (Rubio et al., 2007). Table 1 shows sociodemographic information for both groups.
Description of sociodemographic variables.
| Groups | |||
|---|---|---|---|
| OB-BED (n=48) | OB (n=54) | ||
| Marital status | Single | 35.40% | 22.20% |
| Married | 50.00% | 63.00% | |
| Divorced/separated/widowed | 14.60% | 14.80% | |
| Education level | Primary education | 27.10% | 38.90% |
| Vocational/Professional Training | 37.50% | 42.60% | |
| University studies | 35.40% | 18.50% | |
| Employment | Employed | 43.80% | 48.10% |
| Status | Unemployed | 14.60% | 18.50% |
| Other situations | 41.70% | 33.30% | |
Semi-structured interview for the assessment of BED. This tool was developed ad hoc for the purposes of this study and was based on the diagnostic criteria for BED, as described in DSM-5 (APA, 2013). Its application enabled us to assign participants to one of the two study groups.
Short form of the Depression Anxiety Stress Scales (DASS-21). This is a 21-item version of the original Depression Anxiety Stress Scales developed by Lovibond and Lovibond (1995). It was adapted into Spanish by Bados, Solanas, and Andrés (2005), who reported Cronbach's alphas of .84 for the Depression scale, .70 for the Anxiety scale, and .82 for the Stress scale.
Eating Disorder Examination-Questionnaire (EDE-Q). Originally developed by Fairburn and Beglin (1994), this self-report instrument assesses various eating habits and styles over the past month. It comprises four sub-scales, labelled Shape Concern, Eating Concern, Weight Concern, and Restraint, and it also yields a total score. Cronbach's alphas for the 38-item Spanish adaptation of the EDE-Q were .81 for Restraint, .92 for Shape Concern, .82 for Eating Concern, .83 for Weight Concern, and .95 for the total score (Villarroel, Penelo, Portell, & Raich, 2011).
Emotional Eater Questionnaire (EEQ). This is an instrument developed in Spain by Garaulet et al. (2012) to assess emotional eating in overweight and obese individuals. It comprises 10 items which measure the influence of emotions on eating behaviour. The psychometric study of the EEQ identified three factors: Disinhibition (α=.77), Type of food (α=.66), and Guilt (α=.61) (Garaulet et al., 2012).
Repertory Grid Technique (RGT). This tool was devised by Kelly (1955) as a way of assessing an individual's system of personal constructs (for more recent descriptions, see Feixas & Cornejo, 2002; Fransella, Bell, & Bannister, 2004). By interviewing the individual, a data matrix is obtained with the interplay of three components: elements, which refer to the things or people that are important to the individual in question; constructs, which are the terms used by the individual to make sense of these elements (elicited by exploring similarities and differences between the elements); and the ratings on a 7-point Likert-type scale given by the individual to each element along each construct. As the RGT can provide information about implicative dilemmas and dilemmatic constructs (Feixas & Saúl, 2004), the grid data were used in the present study to generate a variable labelled ‘level of cognitive conflict’: no conflict, moderate level, and high level. The moderate level was characterized by the presence of just one type of conflict (i.e., implicative dilemmas or dilemmatic constructs), whereas individuals regarded as showing a high level presented both these types of cognitive conflict.
A sociodemographic questionnaire was also used to gather data about marital status, level of education, and employment status, as well as the information required to calculate BMI (i.e., the person's weight and height).
ProcedureParticipants were recruited through four health care centres in the Barcelona area, as well as through public advertisements. Each participant was assessed individually in a session lasting approximately two hours. Written informed consent was obtained at the start the session and it was made clear that all collected data would remain confidential. The study was approved by the Bioethics Committee of the University of Barcelona.
Statistical analysisThe first step involved a descriptive and comparative analysis, using the Student's t test for independent samples or, in the case of categorical variables, the chi-square test. Binary logistic regression, with the forward stepwise method, was then performed to detect the variables that were best able to predict membership of the OB-BED group. For this analysis, we excluded six individuals whose repertory grid revealed no cognitive conflicts, as the majority of participants were classified as presenting either a moderate or high level of conflict. Consequently, the sample for the regression analysis comprised 96 participants (n OB-BED=47; n OB=49). The level of statistical significance was set at p<.05, with Bonferroni correction being applied, due to the fact that multiple comparisons were made. Measures of effect size were also calculated. Data from repertory grids were analysed using the RECORD 5.0 program (Feixas, Cornejo, & Laso, 2012), while all other analyses were performed using IBM SPSS for Windows, Version 21.0 (IBM Corp., Armonk, NY, USA).
ResultsThe between-group comparison of sociodemographic variables required a critical alpha value of .007 (α=.05/7) after Bonferroni correction. Following this criterion, application of the chi-square test with Yates’ continuity correction indicated that there were no statistically significant differences between the groups in terms of gender (χ2 (1)=0.00, p=1.00, Cramer's V=.017). As regards age, the OB-BED group was older but not significantly so (t(100)=1.75, p=.082, d=0.35). Neither were any group differences observed in relation to BMI (t(100)=1.15, p=.255, d=0.18), marital status (χ2 (2)=2.31, p=.315, Cramer's V=.150), level of education (χ2 (2)=3.97, p=.137, Cramer's V=.197), or employment status (χ2 (2)=0.82, p=.664, Cramer's V=.09). Comparison of the two groups in terms of the source of recruitment (i.e., heath care centres or public advertisements) also revealed no significant differences (χ2 (1)=3.23, p=.072, Cramer's V=.178). The effect sizes were small for all these comparisons, and the results thus suggest that the two groups can be considered equivalent in terms of gender, age, BMI, marital status, level of education, employment status, and source of recruitment.
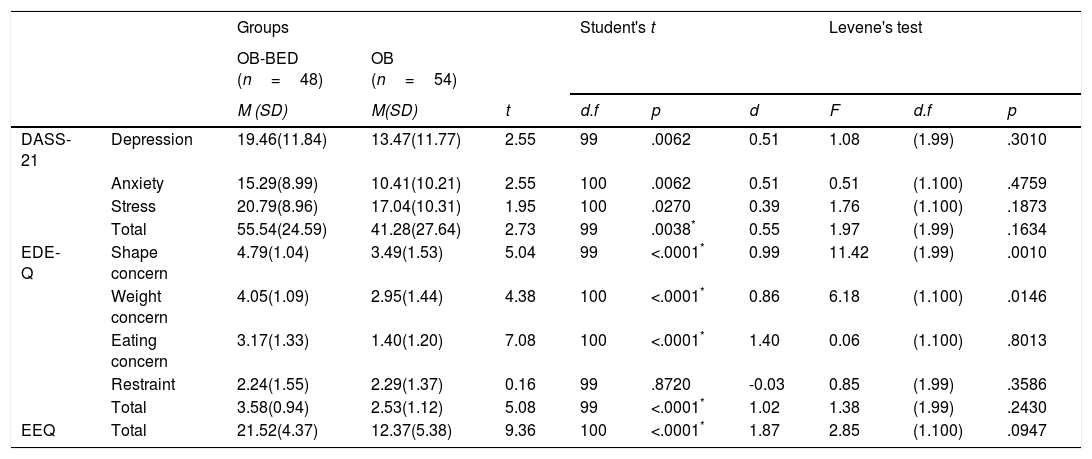
Table 2 shows descriptive and comparative results for the DASS-21, the EDE-Q, and the EEQ (corrected alpha value=.005). We found statistically significant differences between the groups in the total score on the DASS-21 and the EEQ, and for the total score and three of the four sub-scales of the EDE-Q, the exception being Restraint. In all cases, scores were higher in the OB-BED group, with a large effect size, except for the DASS-21 total score, where the effect size was moderate.
Descriptive and comparative results of anxiety, depression and eating symptomatology.
| Groups | Student's t | Levene's test | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OB-BED (n=48) | OB (n=54) | |||||||||
| M (SD) | M(SD) | t | d.f | p | d | F | d.f | p | ||
| DASS-21 | Depression | 19.46(11.84) | 13.47(11.77) | 2.55 | 99 | .0062 | 0.51 | 1.08 | (1.99) | .3010 |
| Anxiety | 15.29(8.99) | 10.41(10.21) | 2.55 | 100 | .0062 | 0.51 | 0.51 | (1.100) | .4759 | |
| Stress | 20.79(8.96) | 17.04(10.31) | 1.95 | 100 | .0270 | 0.39 | 1.76 | (1.100) | .1873 | |
| Total | 55.54(24.59) | 41.28(27.64) | 2.73 | 99 | .0038* | 0.55 | 1.97 | (1.99) | .1634 | |
| EDE-Q | Shape concern | 4.79(1.04) | 3.49(1.53) | 5.04 | 99 | <.0001* | 0.99 | 11.42 | (1.99) | .0010 |
| Weight concern | 4.05(1.09) | 2.95(1.44) | 4.38 | 100 | <.0001* | 0.86 | 6.18 | (1.100) | .0146 | |
| Eating concern | 3.17(1.33) | 1.40(1.20) | 7.08 | 100 | <.0001* | 1.40 | 0.06 | (1.100) | .8013 | |
| Restraint | 2.24(1.55) | 2.29(1.37) | 0.16 | 99 | .8720 | -0.03 | 0.85 | (1.99) | .3586 | |
| Total | 3.58(0.94) | 2.53(1.12) | 5.08 | 99 | <.0001* | 1.02 | 1.38 | (1.99) | .2430 | |
| EEQ | Total | 21.52(4.37) | 12.37(5.38) | 9.36 | 100 | <.0001* | 1.87 | 2.85 | (1.100) | .0947 |
Notes. DASS-21: Short form of the Depression Anxiety Stress Scales; EDE-Q: Eating Disorder Examination-Questionnaire; EEQ: Emotional Eater Questionnaire.
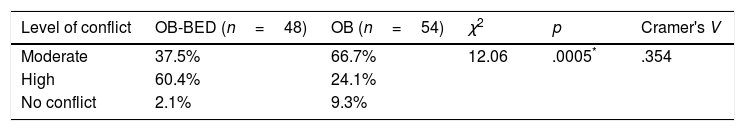
In the comparison of cognitive conflicts the corrected alpha value was .017 (α=.05/3). The proportion of participants presenting implicative dilemmas was 62.5% in the OB-BED group and 32.5% in the OB group, the difference being statistically significant (χ2 (1)=7.60, p=.006, Cramer's V=.273). As regards dilemmatic constructs, these were present in 95.8% of individuals in the OB-BED group and 79.6% of those in the OB group, also a statistically significant difference (χ2 (1)=6.00, p=.014, Cramer's V=.243). Table 3 shows a comparison of the two groups with respect to the level of cognitive conflict, which was higher in the OB-BED group. The value of the effect size (Cramer's V=.354) underlines the importance of this difference between the two groups.
Comparison of the level of cognitive conflict between groups.
| Level of conflict | OB-BED (n=48) | OB (n=54) | χ2 | p | Cramer's V |
|---|---|---|---|---|---|
| Moderate | 37.5% | 66.7% | 12.06 | .0005* | .354 |
| High | 60.4% | 24.1% | |||
| No conflict | 2.1% | 9.3% |
Note.
Correlational analyzes were performed to determine the association between psychological variables and sociodemographic variables. The educational level negatively correlated with Anxiety (rs=-.24, p=.015), Stress (rs=-.22, p=.027) and total DASS-21 score (rs=-.24; p=.015), while age showed a negative association with Weight Concerns (r=-.25; p=.010) and Eating Concern (r=-.20; p=.050).
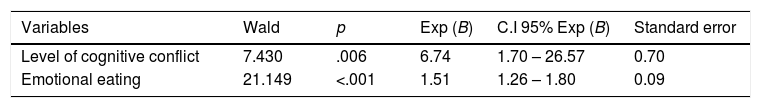
Regarding the logistic regression analyses performed with all the study variables, including BMI, age and educational level, the model that best predicted the presence of BED in obese individuals included the score on the EEQ and the level of cognitive conflict (χ2 (2)=68.69, p<.001), which together explained 69.6% of the variance (Nagelkerke's R2) with respect to the presence of this eating disorder. The results of the Hosmer and Lemeshow test confirmed the goodness of fit of this model (χ2 (8)=8.25, p=.087). Table 4 shows the value of the statistics corresponding to the two variables in this model, indicating that individuals with a high level of cognitive conflict and a high score on emotional eating were more likely to present BED. This model was able to correctly classify 91.4% of our participants. More specifically, it correctly identified 91.3% of individuals with BED and 91.5% of those without this eating disorder.
The same analyzes were performed excluding the male sample (n=7), obtaining similar results, therefore it was decided to report the results of the total group.
DiscussionComparison of our two study groups in terms of symptoms of depression, anxiety, and stress showed that the OB-BED group reported a significantly higher level of general psychological distress, a finding that supports the notion that obese individuals with BED usually present more eating-related psychopathology than do their counterparts without this disorder (Ivezaj, White, & Grilo, 2016; Klatzkin et al., 2015).
Individuals in the OB-BED group also reported greater concern with weight, shape, and eating, as well as more disordered eating in general, a result consistent with previous research by Herbozo, Schaefer, and Thompson (2015) and Klatzkin et al. (2015). Interestingly, our two groups did not differ in terms of eating restraint, a finding contrary to the results of Klatzkin et al. (2015), who reported greater restraint among obese women with BED, compared with an obese non-BED group. However, our results are in line with those of Calderone et al. (2015) and Herbozo, Schaefer, and Thompson (2015), who likewise found no difference between BED and non-BED obese individuals in this regard. This suggests that what leads overweight and obese individuals to restrain their eating is not the presence of BED but, rather, excess weight, a factor which is common to both groups.
As regards to emotional eating, Leehr et al. (2015) observed, in agreement with our findings, that obese individuals with BED were more likely than their non-BED counterparts to turn to food in the face of negative emotions. These results are in line with the findings of Zeeck, Stelzer, Linster, Joos, and Hartmann (2011) who argue that people with BED manifest more negative emotions than those who do not have BED, a variable which was associated with a higher probability of presenting binge.
A study conducted by Dakanalis et al. (2015) confirms this idea, since it was observed that negative emotions referred to body shape or appearance influence the development of binge eating. If these unpleasant internal states are accompanied by a constant attitude of self-criticism, then the severity of binges increases (Lucena-Santos, Carvalho, da Silva Oliveira, & Pinto-Gouveia, 2017).
With respect to cognitive conflicts, our OB-BED group reported more implicative dilemmas, a finding consistent with previous research showing that this type of conflict is more common among a variety of clinical populations (Montesano et al., 2015). Dilemmatic constructs were also more frequent in the OB-BED group, a result contrary to what was observed in the study of Feixas et al. (2009), who found that this type of conflict did not differentiate between clinical and non-clinical samples. These authors do acknowledge though that dilemmatic constructs tend to be more common among individuals with some form of psychopathology, although the previous research that supports this finding was conducted in populations with types of conditions other than eating disorders and obesity. Interestingly, research by Dada (2014) —comparing individuals with different eating disorders, and therefore more pertinent to the present study— found that this type of cognitive conflict was significantly more common in clinical groups than among controls, a result consistent with our own. A possible explanation for our finding is that, as Winter and Button (2011) suggest, eating-related symptomatology is a strategy for regaining control, and in our participants with BED the perceived loss of control is reflected in the higher proportion of dilemmatic constructs, illustrating the uncertainty these individuals feel about what course of action to take.
Our two groups also differed in the level of cognitive conflict they experienced. Specifically, the majority of individuals in the OB-BED group presented a high level of conflict, whereas most of those in the OB group showed a moderate level. These findings are again in line with Dada's (2014) aforementioned research, who found that individuals with a clinically diagnosed eating disorder presented a higher level of conflict than did controls.
Feixas et al. (2014) pointed out that although the notion of internal conflict has a long history in psychology few studies have examined its role in relation to the origins and maintenance of psychopathology. The results of the present study are relevant in this respect, since they suggest that the presence of BED alongside obesity is associated with higher levels of cognitive conflict than is observed with obesity alone. Here, a high level of cognitive conflict was defined as the simultaneous presence of both dilemmatic constructs and implicative dilemmas. This means that the individual not only finds it difficult to choose a course of action in certain spheres of her life but also feels blocked in any attempt to change certain aspects of her identity, since the desired change would imply modifying the position of the self in other constructs, a change which would threaten her sense of identity. Our results indicate that these twin obstacles to change are more commonly experienced by obese individuals with BED than by obese persons without this eating disorder.
The fact that cognitive conflicts play such a key role in the psychological processes of individuals with BED highlights the need not only to incorporate these conflicts into explanatory models of the disorder but also to develop specific interventions for tackling them. These interventions could be modelled on a recently reported treatment manual for depression (Feixas & Compañ, 2015, 2016), which has shown a more than acceptable degree of efficacy (Feixas et al., 2016).
One of the limitations of this study concerns the under-representation of men, despite our intention to recruit participants of both genders. However, the two study groups were comparable in this respect, and hence the results are not influenced by this gender imbalance. Differences in the source of recruitment could potentially have been another limitation, although our analysis suggests that the two groups were also equivalent in this respect. At all events, further studies involving obese males with and without BED are now needed, since the between-group differences may vary by gender. It would also be important to analyse differences between obese individuals with BED and persons of normal weight. Another avenue of interest would be to explore the content of the constructs involved in cognitive conflicts. This would not only add to our understanding of the specific aspects that produce internal conflicts in different eating disorders but would also serve as a conceptual base on which to develop treatment manuals for dilemma-focused interventions.
In conclusion, these results pave the way for further research into the role that cognitive conflicts play in relation to BED, as well as highlighting the importance of emotional eating as a variable that differentiates obese individuals with and without BED.
Acknowledgements and fundingThe authors wish to acknowledge the Department of Clinical Psychology and Psychobiology, and the Department of Social Psychology and Quantitative Psychology both at the University of Barcelona for their support during the conduction of this study. This work was supported by the Comisión Nacional de Investigación Científica y Tecnológica (CONICYT), from the Chilean Government and also by the “Secretariat” for Universities and Research, “Conselleria” of Economy and Knowledge, “Generalitat de Catalunya” (Government of Catalonia, Spain) for their funded recognition of our research group (ref. SGR2014-717).