The current study aimed to examine the relationship between Posttraumatic Stress Disorder (PTSD) symptoms and executive dysfunction in children and adolescents after psychological trauma.
MethodParticipants were 13,438 of children and adolescents aged 6 to 18 years exposed to the 2008 Wenchuan earthquake. PTSD and dysexecutive symptoms were assessed using the UCLA PTSD Reaction Index for Children and the Self-Report Dysexecutive Questionnaire. Latent Profile Analysis (LPA) was conducted using Mplus version 7.4. Subgroup differences in trauma exposure and quality of life were calculated using ANCOVA.
ResultsA 4-class parallel model was found to best describe latent PTSD symptom profiles and executive dysfunction. Individuals in higher symptom groups showed more trauma exposure and lower quality of life.
ConclusionsThis LPA study shed light on the relationship between PTSD and executive dysfunction symptoms in children and adolescents. The correlation between PTSD and executive dysfunction was maintained after individual differences were taken into consideration. Our findings provide a new view on how PTSD relates to executive dysfunction and several suggestions for treating child and adolescent PTSD patients.
Se plantea examinar la relación entre síntomas del Trastorno de Estrés Postraumático (TEPT) y disfunción ejecutiva en niños y adolescentes después de un trauma psicológico.
MétodoLos participantes fueron 13,438 niños y adolescentes de 6 a 18 años de edad expuestos al terremoto de Wenchuan de 2008, a los que se le evaluaron síntomas de TEPT utilizando el UCLA PTSD Reaction Index for Children y síntomas de disfunción ejecutiva mediante el Self-Report Dysexecutive Questionnaire. Se realizó un Análisis de Perfil Latente (APL) mediante Mplus versión 7.4. Las diferencias de subgrupos en la exposición al trauma y la calidad de vida se calcularon utilizando ANCOVA.
ResultadosUn modelo paralelo de 4-clases describe mejor los perfiles de síntomas de TEPT latentes y disfunción ejecutiva. Los grupos con síntomas más intensos mostraron mayor exposición al trauma y menor calidad de vida.
ConclusionesSe aclara la relación TEPT-síntomas de disfunción ejecutiva en niños y adolescentes. La correlación entre el trastorno de estrés postraumático y la disfunción ejecutiva se mantuvo después de considerar la heterogeneidad de la población. Se ofrece una nueva visión de cómo el TEPT se relaciona con la disfunción ejecutiva y varias sugerencias para tratar a pacientes jóvenes con TEPT.
Epidemiological studies revealed that 43% children and adolescents are directly or indirectly exposed to various traumatic events (Barzilay et al., 2018). Exposure to traumatic events causes various mental health problems in youth, with posttraumatic stress disorder (PTSD) being the most common (Yule et al., 2000). PTSD is a mental disorder triggered by traumatic events and is characterized by re-experiencing, avoidance, negative alterations in mood/cognition, and arousal symptoms (American Psychiatric Association APA, 2013). Children and adolescents are vulnerable to experiencing PTSD following natural disasters, with an estimated prevalence between 5% to 43% (Dyregrov, Yule, & Olff, 2018).
In addition to PTSD, cognitive deficits, especially impaired executive function, are also prevalent among children with traumatic experience. Executive function (EF) refers to a set of higher-order cognitive processes which are necessary for cognitive control of behavior, including behavior inhibition, working memory, cognitive flexibility, planning solving, and planning (Martínez, Prada, Satler, Tavares, & Tomaz, 2016). Children and adolescents often show deficits in executive function abilities after exposure to traumatic events. A recent meta-analysis found large effect sizes of overall EF impairments in trauma-exposed children and adolescents when compared with healthy controls (Malarbi, Abu-Rayya, Muscara, & Stargatt, 2016).
The correlation between PTSD and executive dysfunction after trauma exposure was first revealed in clinical practice (Walter & Gunstad, 2010). Better understanding of the relationship between PTSD and executive function could provide more effective and practical treatment strategies for PTSD patients, but little theoretical work has been done to help explain their relationship. Some evidence supported executive dysfunction as a risk factor for PTSD, while others suggested executive dysfunction could be the consequence of PTSD (Aupperle, Melrose, Stein, & Paulus, 2012; Woon, Farrer, Braman, Mabey, & Hedges, 2016). As described by the executive theory of PTSD (Aupperle et al., 2012), the correlation between executive dysfunction and PTSD could also be bidirectional. Although different hypotheses have been proposed, none of them have gained sufficient support from empirical studies.
Emerging meta-analyses have reported difficulties in executive functioning in people with PTSD (Malarbi et al., 2016; Polak, Witteveen, Reitsma, & Olff, 2012; Scott, 2016; Woon et al., 2016), while high heterogeneity of the results from previous studies were highlighted. This high heterogeneity could be in part explained by different measurements of executive function across different studies (Polak et al., 2012). Executive function in PTSD studies was usually measured by neuropsychological tests (Scott, 2016). Trail Making Test Part B (TMT B), Stroop interference and total correct or perseverative response of Wisconsin Card Sorting Test (WCST) are most widely used measurements of executive function in PTSD. It was reported in another review that the total score of Digit Span (DS) test was also a commonly used measurement of executive function in PTSD (Polak et al., 2012). Most studies found PTSD patients performed worse in some of these neuropsychological tests compared to controls, while others not. Neuropsychological tests mainly measure executive function in laboratory contexts, and may fail to capture executive function in daily life (Azouvi et al., 2015). Until now, few studies used measurements of executive function with more ecological validity in PTSD studies. The Self-Report Dysexecutive Questionnaire (DEX-S) is a standardized qualitative and quantitative self-report measure of behavioral difficulties associated with executive functioning (Wilson, Evans, Emslie, Alderman, & Burgess, 1998). The DEX-S scale could better deal with the open-ended nature of everyday life situations than structured neuropsychological tests (Azouvi et al., 2015), and thus address the primary limitation of previous studies (i.e., lacking ecological validity). Furthermore, the application of the DEX-S enables a better investigation into subdomains of executive dysfunctions, including inhibition, goal-directed behavior, executive memory, lack of awareness and agitation (Chaytor, Schmitter-Edgecombe, & Burr, 2006), which provides a comprehensive picture of commonly reported executive dysfunction symptoms. Therefore, the DEX-S was employed to measure difficulties in executive functioning in this study.
According to a systematic review of studies that investigated the presence of executive dysfunction in people with PTSD, although similar measurement of executive function used (predominantly measured by TMT B and DS tests), only 9 studies found significant executive function deficits, while other 7 studies did not (Qureshi et al., 2011). This result implies potential individual difference in the correlation between PTSD and executive dysfunction. However, most previous studies usually compare the executive function in PTSD patients and controls directly, or calculate the correlation between PTSD severity and executive dysfunction in diverse cohorts. These practices do not take individual differences within the sample into consideration. Inadequate information on population heterogeneity limits researchers to gain a consistent conclusion on how PTSD and executive dysfunction correlate in different samples.
Currently, latent profile analysis (LPA) enables us to have a better investigation of the PTSD-EF relationship. LPA is a novel person-centered method that uncovers unobserved heterogeneity in a population by finding meaningful groups of people that are similar in their responses to measured variables, and may therefore be suitable for exploring co-occurring symptom presentations after trauma exposure (Nylund, Asparouhov, & Muthén, 2007). By testing whether executive dysfunction co-occurs with PTSD symptoms in all subgroups, we are able to examine whether individual difference plays an important role in explaining the correlation between PTSD and executive dysfunction. LPA provides us with the best chance to overcome previous methodological limitations, and can advance our knowledge on posttraumatic executive dysfunction and PTSD.
Both PTSD and executive dysfunction have been reported to stably affect functioning outcomes of children and adolescents in daily life (Biederman, Mnonuteaux, Doyle, & Seidman, 2004; Danzi & La Greca, 2017). Therefore, we chose quality of life as an outcome variable to validate the distinction between different symptom patterns.
The key research question of this study was to investigate the association of between executive dysfunction and PTSD following trauma exposure from the perspective of population heterogeneity. In the current study, we first identified subgroups differentiated by symptom profiles of PTSD and executive dysfunction in trauma-exposed children and adolescents. Then we examined whether severity of trauma exposure and quality of life were associated with different symptom profile subgroups. We hypothesized that (1) multiple symptom profile subgroups could be differentiated; (2) trauma exposure and quality of life might be associated with different symptom profiles.
MethodParticipantsOur sample was from Beichuan County of Sichuan Province. This county suffered the most in the 2008 Wenchuan Earthquake. The current sample contained 14,465 children and adolescents in the county. In order to perform the following data analysis procedures, 1,027 potential participants were excluded because of lacking demographic data, leaving an analytic sample of 13,438 students. In the final sample, all participants were between 6 and 18 years old, with a mean age of 12.4 years (SD=2.0). Nearly half (49.7%) were boys, and ethnically identified as Qiang (53.3%), Han (45.2%), Zang (1.3%), and other Chinese ethnicities (0.2%). Those who were excluded showed significantly lower levels of executive dysfunction (p <.01, Cohen's d=0.16), but more severe PTSD symptoms (p <.01, Cohen's d=0.09) when compared with those were included in our study.
ProcedureIn order to investigate the effects of the earthquake on the mental health of children and adolescents, the local education department conducted a survey to students from grade 3 to grade 9 in all the primary schools and secondary schools in Beichuan County (including 24 primary schools and 9 secondary schools) in 2011, 2.5 years after the earthquake. All the participants completed self-report questionnaires in a group-administration format in classrooms. Trained research assistants introduced the aim of the survey to the students and administered the tests with monitoring from the school teachers. Informed consents/assents were obtained from all students and their guardians. All the investigation procedures of the current study were approved by the Ethics Review Board of the Institute of Psychology, Chinese Academy of Sciences.
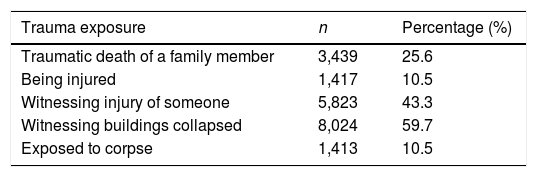
InstrumentsTrauma exposure was measured by a questionnaire asking 5 yes or no questions about traumatic events they experienced during the earthquake (see Table 1). The five items were chosen as they were most commonly reported in our earlier survey to the earthquake survivors just after the earthquake. The total score of the questionnaire was used to reflect the level of earthquake-related trauma exposure.
PTSD symptoms were measured by the UCLA PTSD Reaction Index (PTSD-RI) for DSM-IV (Child Version) (Steinberg, Brymer, Decker, & Pynoos, 2004). The PTSD-RI is a self-reported, 20-item scale designed to capture DSM-IV PTSD symptoms including re-experiencing (e.g., recurrent thoughts of trauma), avoidance (e.g., avoidance of thoughts of trauma), and hyper-arousal (e.g., sleeping difficulties). Each item is scored on a 5-point Likert scale from 0 (none of the time) to 4 (most of the time) to reflect the frequency of present of a particular symptom during the past month. Higher scores indicate more severe PTSD symptoms. Reliability and validity of the Chinese version of the PTSD-RI has been validated, and used in youths exposed to a range of traumatic events including earthquakes (e.g., Cao et al., 2018). In this study, participants were instructed to completed the scale referring to the Wenchuan earthquake, and Cronbach's α was .86 for the total scale in the current sample.
Executive dysfunction symptoms were measured by the Self-Report Dysexecutive Questionnaire (Wilson et al., 1998). The scale is a sensitive and ecologically valid instrument measuring executive functioning across different populations (Shaw, Oei, & Sawang, 2015). It contains 20 items which screen for changes in observable everyday manifestations of executive dysfunction (e.g., inability to inhibit responses), and each item is scored on a five-point Likert scale from 0 (never) to 4 (very often), higher scores indicating higher frequencies of executive function problems in everyday life. The DEX was reported to have good reliability, concurrent validity and criterion validity (Shaw et al., 2015). The Chinese version of the scale has shown good reliability and validity (Yang et al., 2018). Cronbach's α was .92 in the current study.
Quality of life was measured by Pediatric Quality of Life Inventory (PedsQL) 4.0 Generic Core Scales (Varni, Seid, & Kurtin, 2001). It is a self-reported, 23-item, instrument measuring impairments in four subdomains of quality of life for children on a 5-point Likert scale from 0 (never a problem) to 4 (almost always a problem): physical (e.g., hard to run), emotional (e.g., feel sad or blue), social (e.g., trouble getting along with peers), and school functioning (e.g., trouble keeping up with school work). Scale scores were calculated as the sum of item responses, and higher scores indicate more impairment in quality of life. The Chinese version of the PedsQL scale has demonstrated good reliability and validity (Wang et al., 2017). In this study, Cronbach's α was .91 for the total scale.
Design and data analysisIn the first step, LPA was used to investigate the pattern for co-occurrence of executive dysfunction and PTSD symptoms. It has been recommended to use factors rather than items as indicators of LPA, as this approach could minimize the correlations between observed variables within the classes (Dalenberg, Glaser & Alhassoon, 2012). Regarding PTSD symptoms, it has been well-documented that the 5-factor dysphoric arousal model comprised of intrusion, avoidance, emotional numbing, anxious arousal and dysphoric arousal generally outperformed other alternative models across DSM-IV based PTSD measures including the PTSD-RI (Elhai et al., 2013). With regard to executive dysfunction symptoms, domains including inhibition, goal-directed behavior, executive memory, lack of awareness and agitation in daily life factors better captured the factor structure of the DEX-S (Chaytor et al., 2006). Thus, scores on the five PTSD and five executive dysfunction symptom clusters were used as indicators in LPA. Skewnesses and kurtoses for scores on the five PTSD symptom clusters ranged from 0.70 to 1.34 and from 0.30 to 2.28, respectively. Skewnesses and kurtoses for scores on the five executive dysfunction symptom clusters ranged from 0.70 to 0.96 and from 0.35 to 0.85, respectively. All the ten scores were further transformed to T scores for a more clear and consistent interpretation of the results. Given possibly moderate effects of age, sex and ethnicity on the relationship between PTSD and executive function (Polak et al., 2012), effects of these covariates on latent classes were estimated by a 3-step procedure (Vermunt, 2010). The 3-step procedure was selected because it regresses the dependent variable (the latent class) on the covariates, meanwhile taking into account misclassification from posterior probability estimation.
LPA was conducted with Mplus 7.4 using maximum likelihood estimation. We compared latent class models ranging from one to five classes, and the best model was determined using these guidelines: (1) lower Bayesian Information Criterion (BIC) or lower Akaike Information Criterion (AIC) values indicated better model fit. (2) Lo–Mendell–Rubin likelihood ratio test (LMR LRT), adjusted LMR LRT (ALMR LRT) and bootstrapped likelihood ratio test (BLRT) were used to evaluate whether a model with k classes fit better than a model with k-1 classes. Significant LRT values mean the k class model is better than the k-1 class model. (3) Entropy scores closer to 1 suggest a greater proportion of individuals were classified accurately.
Subsequently, ANCOVA was conducted with SPSS 20.0 to examine between-class differences in trauma exposure and quality of life. Considering the big range of age in the current sample, age was controlled as a covariate. If ANCOVA findings were significant at the 0.05 level, we then performed post-hoc pairwise comparisons using Games–Howell tests. Bonferroni correction was used to control for multiple comparisons. Skewness and kurtosis for trauma exposure score was 0.55 and 0.94, respectively. Skewness and kurtosis for quality of life score was 0.85 and 0.98, respectively.
ResultsFor all the participants, mean earthquake trauma exposure values were 1.5 (SD=1.3; range: 0-5). Mean scores on the PTSD-RI were 14.1 (SD=9.3) in our sample, ranging from 0 to 68. Probable PTSD diagnosis was inferred using the DSM-IV diagnostic algorithm of at least one re-experiencing, three avoidance/numbing and two arousal symptoms endorsed at the level of 2 or higher (scale range: 0-4), and 12.1% (n=1,629) of the trauma-exposed students met the diagnostic criteria. The average score for DEX-S was 20.0 (SD=13.0; range: 0-80), and the mean level of impairments in quality of life was 21.5 (SD=14.0; range: 0-92).
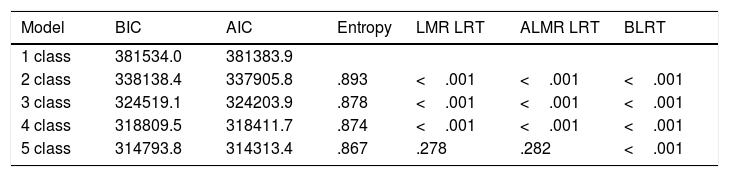
We found a 4-class model yielded the best fit to the data. The fit indices for LPA are shown in the table (see Table 2). The LMR LRT and ALMR LRT values were significant for the 5-class solution but not the 4-class solutions. Entropy of the 4-class solution was higher than the 5 class solutions, which means higher classification accuracy. Thus, based on all available evidence, the 4-class model was determined as the optimal model in terms of fit, parsimony and interpretability.
Fit indices for LPA between 1-5 classes.
| Model | BIC | AIC | Entropy | LMR LRT | ALMR LRT | BLRT |
|---|---|---|---|---|---|---|
| 1 class | 381534.0 | 381383.9 | ||||
| 2 class | 338138.4 | 337905.8 | .893 | <.001 | <.001 | <.001 |
| 3 class | 324519.1 | 324203.9 | .878 | <.001 | <.001 | <.001 |
| 4 class | 318809.5 | 318411.7 | .874 | <.001 | <.001 | <.001 |
| 5 class | 314793.8 | 314313.4 | .867 | .278 | .282 | <.001 |
Note. N=13438. BIC=Bayesian information criterion; AIC=Akaike information criterion; LMR LRT=Lo–Mendell–Rubin likelihood ratio test; ALMR LRT=Lo–Mendell–Rubin adjusted likelihood ratio test; BLRT=bootstrap likelihood ratio test.
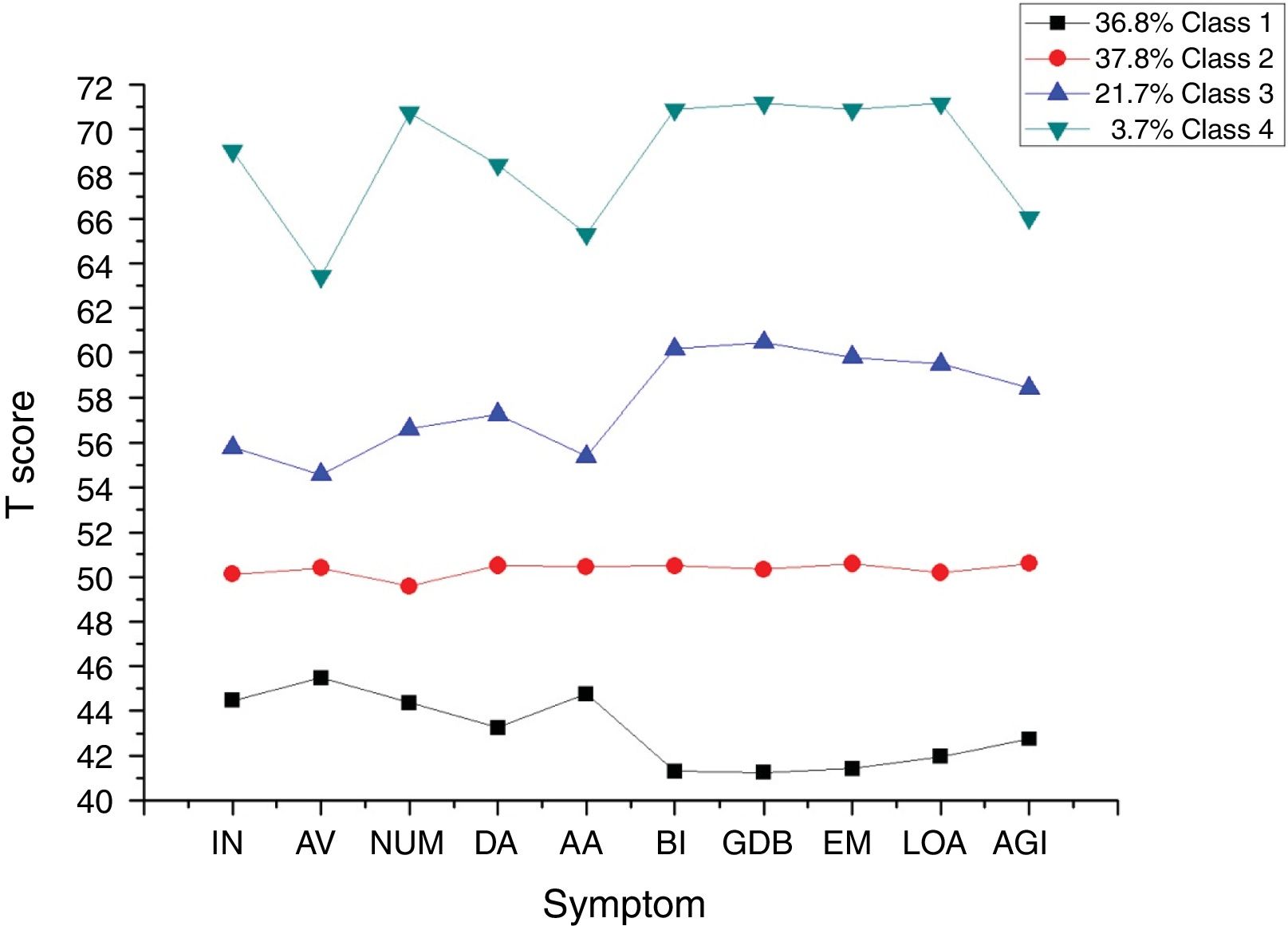
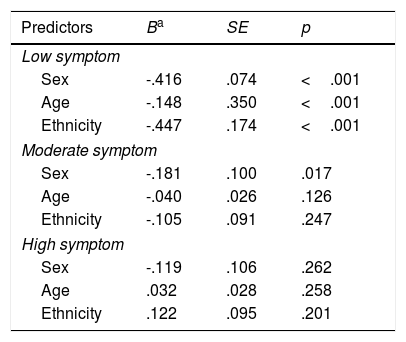
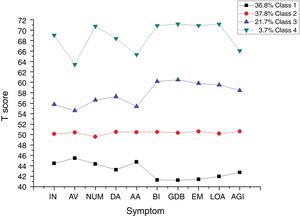
The 4-class solution was characterized by low symptom, moderate symptom, high symptom and extremely high symptom patterns. Figure 1 shows the corresponding profile plot for the ten summed scores of PTSD and executive dysfunction. Within each class, executive dysfunction severity co-occurred with comparable PTSD symptom severity. None of the four classes reflected a high-PTSD/low-executive dysfunction or high-executive/low-PTSD profile. The 3-step procedure tested covariates in relation to class membership (see Table 3). Significant relations with class membership for age, sex and ethnicity were found between the low symptom and extremely high symptom classes. The results show that more females, more non-Han ethnicity and younger age children were present in the extremely high symptom group when compared with the low symptom group. Sex difference was also found between moderate symptom and extremely high symptom classes. More females were present in the extremely high symptom group when compared with the moderate symptom group.
Demographic variables as predictors of different groups.
| Predictors | Ba | SE | p |
|---|---|---|---|
| Low symptom | |||
| Sex | -.416 | .074 | <.001 |
| Age | -.148 | .350 | <.001 |
| Ethnicity | -.447 | .174 | <.001 |
| Moderate symptom | |||
| Sex | -.181 | .100 | .017 |
| Age | -.040 | .026 | .126 |
| Ethnicity | -.105 | .091 | .247 |
| High symptom | |||
| Sex | -.119 | .106 | .262 |
| Age | .032 | .028 | .258 |
| Ethnicity | .122 | .095 | .201 |
Note. N=13,438. Extreme high symptom group was set as reference.
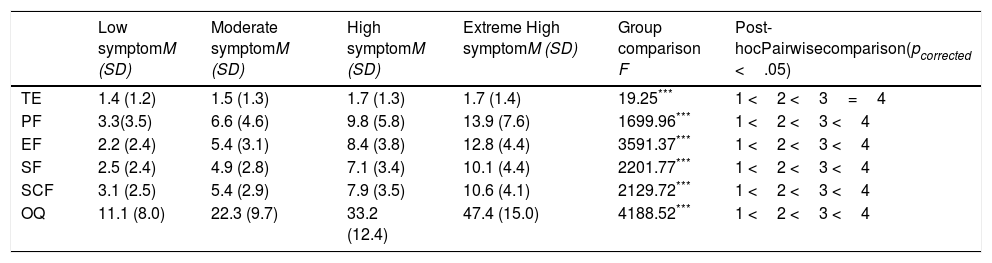
ANCOVAs revealed significant differences for trauma exposure and total impairment in quality of life between different symptom patterns (see Table 4). Four sub-dimensions of quality of life deficits were further examined and the results were consistent with the total score analyses. With regard to trauma exposure, those in the higher co-occurring symptoms group rated higher on trauma exposure measures. As for quality of life, groups with more severe symptoms reported more impairment in total and all dimensions of quality of life. The effect sizes of the difference between groups are presented in Table 5.
Differences in trauma exposure and impairments in quality of life between different subgroups.
| Low symptomM (SD) | Moderate symptomM (SD) | High symptomM (SD) | Extreme High symptomM (SD) | Group comparison F | Post-hocPairwisecomparison(pcorrected <.05) | |
|---|---|---|---|---|---|---|
| TE | 1.4 (1.2) | 1.5 (1.3) | 1.7 (1.3) | 1.7 (1.4) | 19.25*** | 1 <2 <3=4 |
| PF | 3.3(3.5) | 6.6 (4.6) | 9.8 (5.8) | 13.9 (7.6) | 1699.96*** | 1 <2 <3 <4 |
| EF | 2.2 (2.4) | 5.4 (3.1) | 8.4 (3.8) | 12.8 (4.4) | 3591.37*** | 1 <2 <3 <4 |
| SF | 2.5 (2.4) | 4.9 (2.8) | 7.1 (3.4) | 10.1 (4.4) | 2201.77*** | 1 <2 <3 <4 |
| SCF | 3.1 (2.5) | 5.4 (2.9) | 7.9 (3.5) | 10.6 (4.1) | 2129.72*** | 1 <2 <3 <4 |
| OQ | 11.1 (8.0) | 22.3 (9.7) | 33.2 (12.4) | 47.4 (15.0) | 4188.52*** | 1 <2 <3 <4 |
Note. N=13,438;
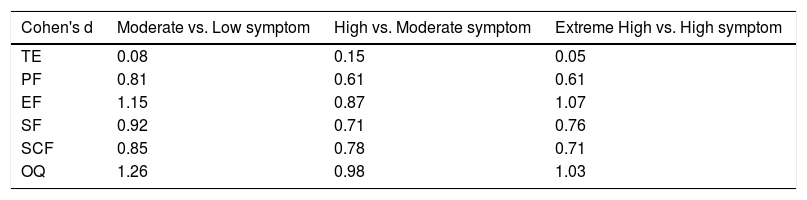
Cohen's ds for comparisons of trauma exposure and impairments in quality of life between different subgroups.
| Cohen's d | Moderate vs. Low symptom | High vs. Moderate symptom | Extreme High vs. High symptom |
|---|---|---|---|
| TE | 0.08 | 0.15 | 0.05 |
| PF | 0.81 | 0.61 | 0.61 |
| EF | 1.15 | 0.87 | 1.07 |
| SF | 0.92 | 0.71 | 0.76 |
| SCF | 0.85 | 0.78 | 0.71 |
| OQ | 1.26 | 0.98 | 1.03 |
Note. N=13,438; TE=trauma exposure; PF=physical functioning; EF=emotional functioning; SF=social functioning; SF=school functioning; OQ=overall quality of life.
We found that a 4-class parallel model best described the profile of PTSD symptoms and executive dysfunction in a large epidemiological sample of Chinese child and adolescent earthquake survivors using latent profile analysis. Low symptom, moderate symptom, high symptom, and extremely high symptom profiles were identified based on five PTSD and five executive dysfunction subscales. Individuals in the extremely high symptom group showed the most severe PTSD symptoms and executive deficits while those in the low symptom group showed the least. The severity of PTSD and dysexecutive symptoms tightly cohered within each class and none of the classes showed predominant PTSD or executive dysfunction symptoms. Individuals in the low symptom group differed from those in the extremely high symptom group by sex, age, and ethnicity. Further analysis showed that children and adolescents in the higher co-occurring PTSD and executive dysfunction symptom group experienced more severe trauma exposure and showed more impairment in quality of life including physical, emotional, social, and school functioning, with small to high effect sizes.
This parallel symptom pattern revealed in our study provides support for a correlation between PTSD and executive dysfunction in trauma exposed children and adolescents, by using a measurement of executive function with more ecological validity. The result was in consistent with some studies using neuropsychology tests to assess executive function (DePrince, Weinzierl, & Combs, 2009; Malarbi et al., 2016). As previously reviewed (Qureshi et al., 2011), there seems to be some evidence of executive impairment in survivors of natural disasters. Another study did not find executive function deficits in those diagnosed with PTSD in a Chinese sample of children and adolescents following the 2008 Wenchuan earthquake (Yang et al., 2014). However, the orphan samples in their study moved away from the disaster area one month after the earthquake and received substantial social support. The effect of social support on the relationship between PTSD and executive dysfunction was not assessed in their study. Furthermore, our results showed that those with moderate PTSD severity also demonstrate executive dysfunction symptoms. This current finding is consistent with a previous finding that once PTSD develops, executive dysfunction often occurs regardless of PTSD severity (Woon et al., 2016). Additionally, our results revealed the association between PTSD and general executive dysfunction as none of the five subscales of executive dysfunction showed a specific significant correlation with PTSD symptoms according to the symptom profiles identified by LPA. This was consistent with the findings of a meta-analysis (Polak et al., 2012), which supports a link between PTSD and general executive dysfunction.
Our current findings have important theoretical implications. Current theoretic work has described a bidirectional relationship between PTSD and deficits in executive function, which may further form a negative feedback loop between them (Jacob, Dodge & Vastering, 2019). This negative feedback theory would be important for our understanding of the relationship between PTSD and executive function. The theory was based on the assumption of no individual difference in the relationship between PTSD and executive function. By addressing the issue of individual difference, the current study provided critical support for the negative feedback theory. The lack of a class with mainly PTSD or mainly executive dysfunction suggests no individual difference in the relationship between PTSD and executive function, the PTSD-EF association might exist in all populations, rather than restricted to a particular subpopulation.
In addition, the parallel symptoms patterns also enable us to propose a novel hypothesis to explain the relationship between PTSD and executive dysfunction. Previous researchers believe executive dysfunction can either be a risk factor or consequence of PTSD (Aupperle et al., 2012; Woon et al., 2016). While in the current study, the lack of a class with mainly PTSD or mainly executive dysfunction symptoms suggests that they typically co-occur and share comparable underlying etiology. This implies that PTSD and executive dysfunction could represent different aspects of a general pathological response following trauma exposure. Differences in co-occurring symptom severity between low, moderate, high and extremely high symptom classes reflects different severity of the general posttraumatic maladaptive response. This hypothesis is also supported by other previous studies. A previous study on trauma-exposed people found weaknesses in executive functioning were present as soon as PTSD developed and that they were not necessarily a long-term consequence of PTSD (LaGarde, Doyon, & Brunet, 2010). Another study uncovered abnormal inhibitory control reflected common posttraumatic psychological distress rather than symptoms unique to PTSD (DeGutis et al., 2015). Thus, it would be interesting to test this hypothesis in future studies.
Our study also provides potential insights into clinical practices. First, according to our current study, those with severe PTSD symptoms usually show higher of executive dysfunction severity. As children with severe PTSD symptoms might have more impairments in executive function, therapies demanding greater executive function may not be optimal (Woon et al., 2016). Instead, therapies such as behavioral therapies or pharmacotherapies might be a better approach. Second, considering PTSD and executive dysfunction were reflective of one another, it gives theoretical evidence to use executive function as a hallmark of PTSD during treatment for PTSD patients. As executive function can be measured by neuropsychological tests, results could be more objective and reliable than PTSD symptoms measured by self-report questionnaires and thus better reflect the outcome of PTSD treatment. Moreover, PTSD symptom scales may not apply to some populations such as young children, and executive function tests could be used instead to monitor their PTSD symptoms during intervention. There are examples of clinicians using baseline and post-treatment executive tests to assess trauma-focused therapy outcome in PTSD patients (Walter & Gunstad, 2010). Last but not least, our study found sex could be an important moderating variable of different symptom patterns, girls are more likely to be in extreme high symptom group when compared with low and moderate symptom group, suggesting that more attention should be paid to PTSD and executive dysfunction symptoms of trauma-exposed girls.
Some limitations of the study should be mentioned. First, measurement of PTSD was based on DSM-IV. In DSM-5, several symptoms of PTSD were changed and new symptoms were added. Relationship between PTSD and executive dysfunction still need to be investigated using new diagnostic criteria for PTSD. Second, our study was conducted in Chinese children and adolescents after experiencing an earthquake. Studies using examples from different populations exposed to various trauma types are necessary for a thorough understanding our research question. Specially, it would be interesting to investigate their relationship among child maltreatment-exposed population, given the high prevalence of PTSD after maltreatment (Dias, Sales, Mooren, Mota-Cardoso & Kleber, 2017). Finally, our survey used a cross-sectional design, and was conducted 2.5 years after the earthquake, which reflects the chronic effects of trauma exposure. Future studies using longitudinal designs are needed for further understanding of the relationship between PTSD and executive function.
Despite the aforementioned limitations, our study is the first to use a person-centered approach to identify symptom patterns of co-occurring PTSD and executive dysfunction in a large epidemiological sample of children and adolescent earthquake survivors. A 4-class parallel model of PTSD and executive dysfunction symptoms was revealed, which supports a correlation between PTSD and executive dysfunction in children and adolescents. We found this correlation was maintained after we took individual differences into consideration. Our findings provided a novel view on how PTSD relates to executive dysfunction and offer several suggestions for clinical practices when treating PTSD patients.
FundingThis study was partially supported by the External Cooperation Program of Chinese Academy of Sciences (No. 153111KYSB20160036), the National Natural Science Foundation of China (No.31271099, 31471004), the Key Project of Research Base of Humanities and Social Sciences of Ministry of Education (No.16JJD190006), and the Beijing Municipal Science and Technology Commission (No. Z171100000117014) the Key Research Program of the Chinese Academy of Sciences (No. ZDRW-XH-2019-4).