The aim of this paper was to evaluate the diferential efficacy of cognitive behavioral family treatment in children under 8 years of age with Obsessive-Compulsive Disorder (OCD) in the reduction of obsessive-compulsive responses and secondary outcomes in three treatment conditions: (a) Treatment of parents and child, (b) Treatment of mother and child, and (c) Treatment of mother.
MethodForty-four children with obsessive-compulsive disorder, aged 5.2-7.9 years old and their parents, were randomized to one of three groups in a 1:1:1 ratio. Seventy-five percent was male and 100% Caucasian (White-European). Treatment involved 12 individual sessions of is Cognitive-Behavioral Family-Based Treatment delivered.
ResultsThe three conditions produced clinical improvements in post-test and follow-up in the primary (symptom severity OCD) and secondary outcomes. The results showed no intergroup differences in variables related to OCD symptom severity, although statistically significant differences were found in groups in Internalizing and Externalizing problem, mother and fathers accomodation.
ConclusionsThe most efficient condition was that including a greater number of family members even when there was high family accommodation. The direct involvement of the child in the psychological treatment was important in achieving better results.
El objetivo fue analizar la eficacia diferencial de un tratamiento cognitivo-conductual para la reducción de obsesiones y compulsions y otras medidas secundarias en niños menores de 8 años con Trastorno Obsesivo-Compulsivo (TOC). Las tres condiciones de tratamiento fueron: (a) Tratamiento a los padres y al niño, (b) Tratamiento a la madre y al niño, (3) Tratamiento a la madre.
MétodoCuarenta y cuatro niños, con edades comprendidas entre 5,2–7,9 años, y sus padres fueron asignados al azar a uno de los tres grupos, ratio de 1:1:1. El 75% eran varones y el 100% españoles. El tratamiento consistió en 12 sesiones individuales de Terapia familiar cognitivo-conductual.
ResultadosLas tres condiciones de tratamiento produjeron mejorías clínicas en el postest y seguimiento en las medidas primarias (severidad TOC) y secundarias. Los resultados mostraron que no existían diferencias entre los grupos en las variables relacionadas con síntomas de severidad, mientras que sí se hallaron en problemas internalizantes y externalizantes, y acomodación de la madre y del padre.
ConclusionesLa condición más eficiente fue la que incluía mayor número de miembros familiares, sobre todo cuando había una mayor acomodación familiar. La participación directa del niño en el tratamiento psicológico fue importante para lograr mejores resultados.
Several studies report early onset Obsessive-Compulsive Disorder (OCD) indicating that children are often under diagnosed for various reasons. Among these are that parents consider symptoms of this behavior as simply transitory. In addition, some children might hide these symptoms from their parents. Both children and parents are unable to assess the frequency of the rituals and intensity of the distress. It has also been shown that a high percentage of adults suffering OCD have reported that their symptoms began in childhood or adolescence (Geller & March, 2012).
Treatment options for children with OCD include Cognitive Behavioral Therapy (CBT), pharmacotherapy or both (Geller & March, 2012; Selles et al., 2018). The American Academy of Child and Adolescent Psychiatry Committee on Quality Issues (2012) considers that the standard of care in very young children with OCD is Cognitive-Behavioral Family-Based Treatment (CBFT), which includes the same core components of CBT with significant family involvement. Parent involvement in treatment for young children with OCD is of particular importance for several reasons. First, the absence or little introspection of minors regarding obsessions and compulsions hinders their involvement in treatment and motivation for change (Bornas, Torre-Luque, Fiol-Veny, & Balle, 2017; Chou, DeSerisy, Garcia, Freeman, & Comer, 2017). Second, high levels of distress, anxiety and conflict have been observed in relatives of children with OCD (Ho, Dai, Mak, & Liu, 2018; Peris et al., 2012). Third, behavioral family accommodation can have important implications in the course and maintenance of a child's OCD (Lebowitz, 2016; Wu & Storch, 2016). Finally, the fact that the parents participate as co-therapists and carry out the exposure tasks at home allows us to come closer to ideal treatment as this contributes both to generalizing and maintaining achievements (Fernández-Sogorb, Inglés, Sanmartín, Gonzálvez, & Vicent, 2018; Kreuze, Pijnenborg, de Jonge, & Nauta, 2018; Stewart et al., 2017).
The first study exclusively with young children with OCD (4-8 years olds) was carried out by Freeman et al. (2008). Freeman et al. (2014) conducted a study with 127 children (4-8 years), reported on the efficacy of CBFT in a multicenter RCT, where CBFT was superior to family-based relaxation training in reducing obsessive-compulsive symptoms. Lewin et al. (2014) used the CBFT with children 3-8 years, more focused on EPR, compared to treatment in Muscle Relaxation and Education in positive emotions. The effect size in reducing obsessive-compulsive symptoms was high (d=1.8). Clinical response percentage was 58.8% (mean CY-BOCS ≤ 12) in CBFT. In addition, improvements were obtained in other secondary measures. Other researchers have reported a series of single case studies, obtaining positive results in very young children (Comer et al., 2017) even when treatment was performed on the Internet (Aspvall el al., 2018). Rosa-Alcázar et al. (2017) presented the results of the comparison of two intervention (mother and child and only mothers) of a program developed and adapted to young children (Rosa-Alcázar, 2012a). Some limitations of this study were its reduced sample size (n=10), the need to increase exposure sessions and the failure to include measures to evaluate the accommodation of both parents.
The main aims of the study was: (1) to test differential efficacy of a modified family intervention program (Rosa-Alcázar, 2012a, 2012b, 2012c) for children with OCD between 5-8 years old in the primary outcome (CY-BOCS) through three treatment conditions (a) Treatment of parents and child, (b) Treatment of mother and child, and (c) Treatment of mother. (2) To analyze the percentage of participants in post-test and in follow-up who met the clinical remission criteria, defining it as a reduction in the Total CY-BOCS. (3) To examine the differential outcome on secondary measures (Global assessment, Child problem behavior, Family Accomodation).
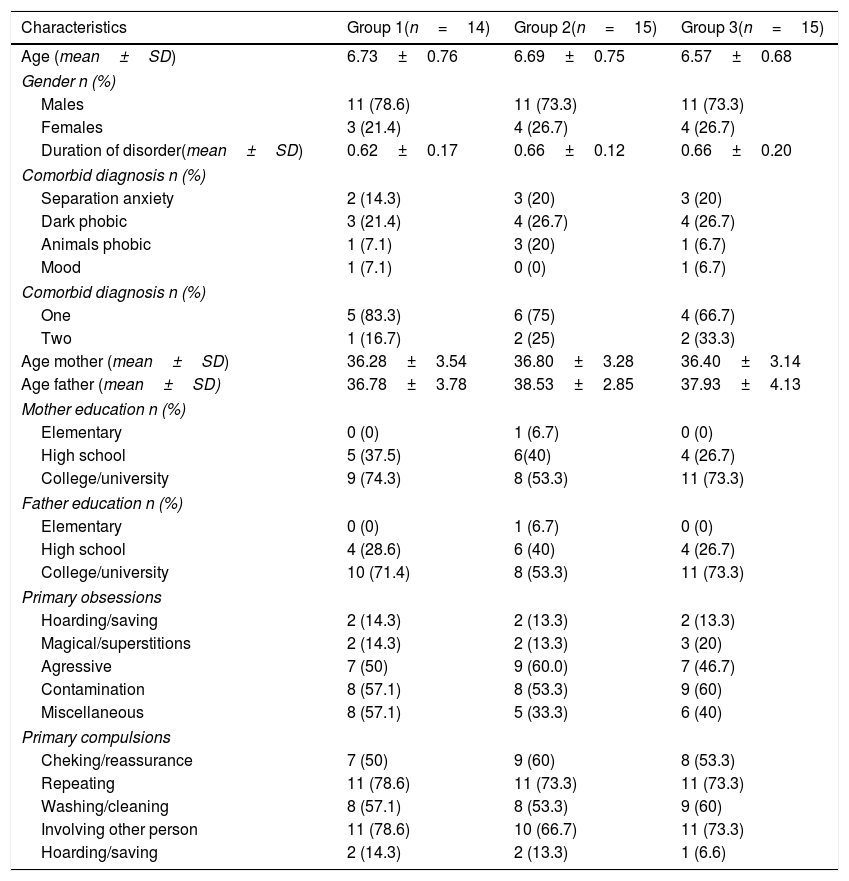
MethodParticipantsParticipants were 44 children (75% males) between 5.20-7.90 years old (M=6.66, SD=0.72) recruited from eight public and private clinics in Murcia (n=3), Castilla-La Mancha (n=2) and Valencia Regions (n=3) of Spain from 2012 to Dicember 2018. Five clinics –psychological consultations- were private and three public (Mental Health Units for Children and Youth). All were caucasian (white-european) and urban. The inclusion criteria were: (a) primary diagnosis of OCD according to DSM-IV-TR, DSM-5 criteria (American Psychiatric Association, 2000, 2014); (b) a clinical severity rating of ≥16 in Childreńs Yale-Brown Obsessive-Compulsive Scale (CY-BOCS; Scahill et al., 1997); and (c) the parents having available to actively participate in the therapeutic process. Upon study entry, all parents of participating children were married and cohabitating. Exclusion criteria included: (a) comorbid autism spectrum disorder, attention deficit hyperactivity disorder, psychotic symptoms, developmental disorder that would affect the child's ability to participate in treatment, or intellectual disability; (b) concurrent psychological therapy; and (c) medications not stable for> 8 weeks. Sample characteristics are presented in Table 1.
Demographic and diagnostic information by group.
| Characteristics | Group 1(n=14) | Group 2(n=15) | Group 3(n=15) |
|---|---|---|---|
| Age (mean±SD) | 6.73±0.76 | 6.69±0.75 | 6.57±0.68 |
| Gender n (%) | |||
| Males | 11 (78.6) | 11 (73.3) | 11 (73.3) |
| Females | 3 (21.4) | 4 (26.7) | 4 (26.7) |
| Duration of disorder(mean±SD) | 0.62±0.17 | 0.66±0.12 | 0.66±0.20 |
| Comorbid diagnosis n (%) | |||
| Separation anxiety | 2 (14.3) | 3 (20) | 3 (20) |
| Dark phobic | 3 (21.4) | 4 (26.7) | 4 (26.7) |
| Animals phobic | 1 (7.1) | 3 (20) | 1 (6.7) |
| Mood | 1 (7.1) | 0 (0) | 1 (6.7) |
| Comorbid diagnosis n (%) | |||
| One | 5 (83.3) | 6 (75) | 4 (66.7) |
| Two | 1 (16.7) | 2 (25) | 2 (33.3) |
| Age mother (mean±SD) | 36.28±3.54 | 36.80±3.28 | 36.40±3.14 |
| Age father (mean±SD) | 36.78±3.78 | 38.53±2.85 | 37.93±4.13 |
| Mother education n (%) | |||
| Elementary | 0 (0) | 1 (6.7) | 0 (0) |
| High school | 5 (37.5) | 6(40) | 4 (26.7) |
| College/university | 9 (74.3) | 8 (53.3) | 11 (73.3) |
| Father education n (%) | |||
| Elementary | 0 (0) | 1 (6.7) | 0 (0) |
| High school | 4 (28.6) | 6 (40) | 4 (26.7) |
| College/university | 10 (71.4) | 8 (53.3) | 11 (73.3) |
| Primary obsessions | |||
| Hoarding/saving | 2 (14.3) | 2 (13.3) | 2 (13.3) |
| Magical/superstitions | 2 (14.3) | 2 (13.3) | 3 (20) |
| Agressive | 7 (50) | 9 (60.0) | 7 (46.7) |
| Contamination | 8 (57.1) | 8 (53.3) | 9 (60) |
| Miscellaneous | 8 (57.1) | 5 (33.3) | 6 (40) |
| Primary compulsions | |||
| Cheking/reassurance | 7 (50) | 9 (60) | 8 (53.3) |
| Repeating | 11 (78.6) | 11 (73.3) | 11 (73.3) |
| Washing/cleaning | 8 (57.1) | 8 (53.3) | 9 (60) |
| Involving other person | 11 (78.6) | 10 (66.7) | 11 (73.3) |
| Hoarding/saving | 2 (14.3) | 2 (13.3) | 1 (6.6) |
Note. Group 1: Parents and child; Group 2: Mother and child; Group 3: Mother; SD: Standard Deviation.
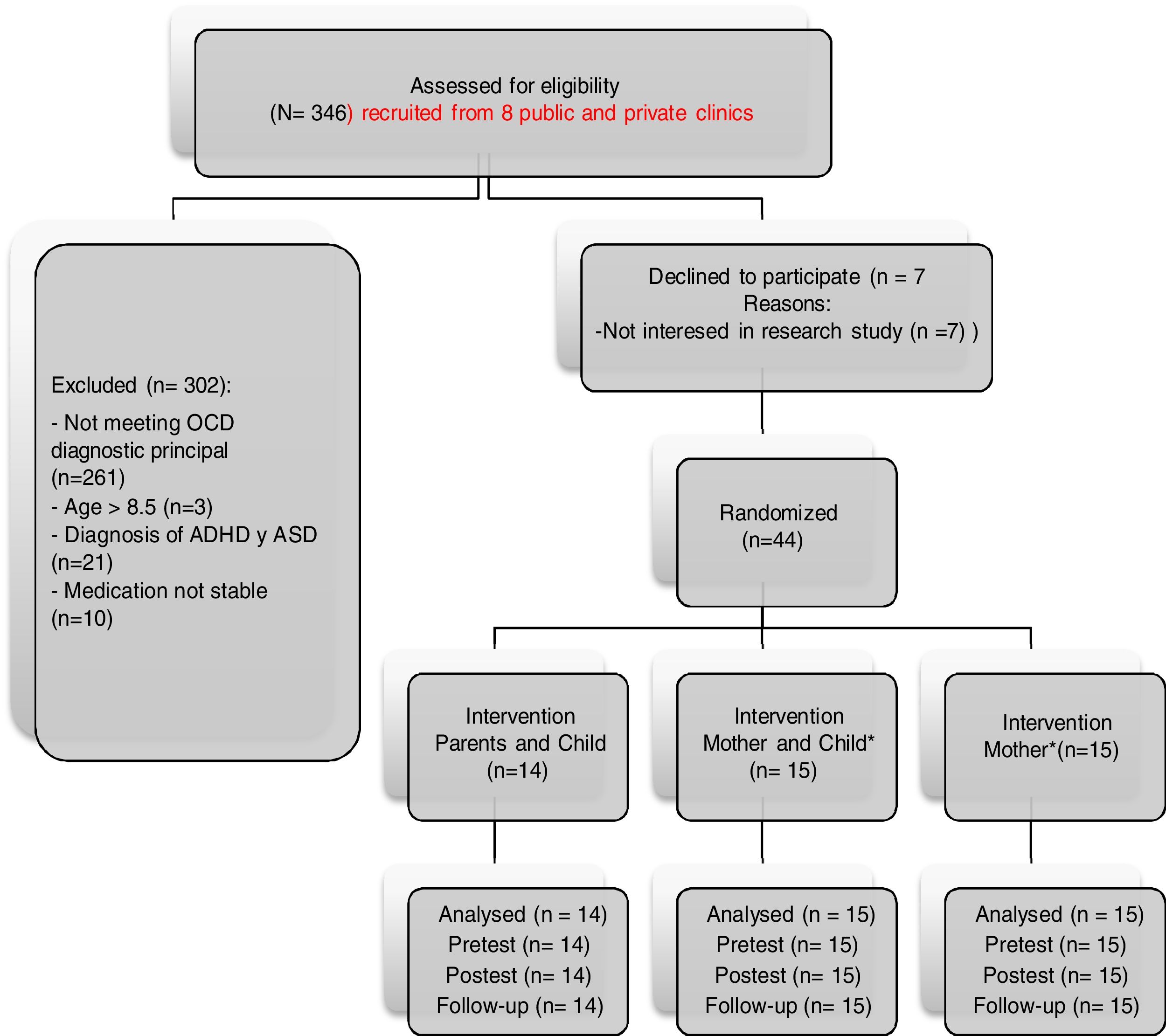
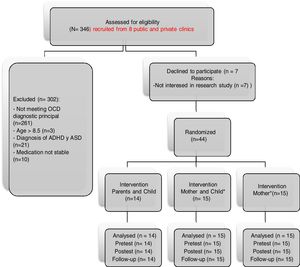
The study met ethical standards according to the Declaration of Helsinki and has been approved by the Ethics Committee of the University of Murcia (Spain). All families provided written informed consent. The recruitment flow is shown in Figure 1. The procedure was as follows: (1) Information from eight clinics about study performance (from 2012 to 2018); (2) the first and the second authors carried out an unstructured clinical interview (DSM-IV-TR and DSM-5). Two specialized child-psychologists administered the Initial Assessment Interviews Involved (ADIS-P/C; Silverman, Albano, & Sandín, 2003) and the CY-BOCS (Scahill et al., 1997) a parents. (3) The children with CY-BOCS≥ 16 met inclusion criteria and formed part of the program.
Assessments were done in three time points (pre-treatment, post-treatment and 3-month follow-up period) by two clinicians specialized in childhood anxiety disorders blinded to group assignment. Sessions were attended by both parents and children. After obtaining written informed consent from the parents, families were randomized to treatment conditions at a 1:1:1 ratio using pre-prepared, sealed envelopes. The randomization sequence was generated by a research assistant using a computer and blocking assignments as a function of the child age and sex and age of the parents. Treatment was implemented by two clinicians specialized in OCD (over 15 years of experience). Clinicians were trained to administer CBT protocol in the uniform fashion prior to initiating the study. Considering their years of experience, we can assume that the both clinicians exhibited similar competence. Half of the patients in the group were treated by each of the two therapists. Forty four families whose children met inclusion criteria were offered a discount (−30%) off the treatment price if they participated in the study.
InstrumentsAnxiety Disorders Interview Schedule for DSM-IV-Child and Parents (ADIS-IV-C/P; Silverman, Albano, & Barlow, 1996). This interview was administered to the children and parents. It has been widely used, demonstrating validity and inter-rater in samples with very young children.
Children's Yale Brown Obsessive Compulsive Scale (CY-BOCS; Scahill et al., 1997). This interview was jointly administered to children and parents to assess overall OCD symptom severity. The CY-BOCS yields an Obsessions Severity score, Compulsion Severity and Total score. This scale has shown excellent psychometric properties in very young children. A Total score greater or equal to 16 is considered clinically significant. In this study Cronbach́s alpha was .87
Childreńs Global Assessment Scale (CGAS; Shaffer et al., 1983). The CGAS assesses global functioning (psychological, social and occupational) across a 0–100 scale with higher scores representing better functioning.
Child Behavior Checklist (CBCL; Achenbach, 1991). The CBCL includes 118-items to assess behavioral and emotional problems in children (externalizing and internalizing problems) during the prior 6 months. This measure has shown adequate internal consistency, convergent validity, and sensitivity and specificity. In this study, Cronbach́s alpha for internalizing and externalizing problems was high (α=.89; α=.90, respectively).
Family Accomodation Scale (FAS; Calvocoressi et al., 1999). Items are rated according to a 5-point Likert scale from 0 (Never) to 4 (Extreme). This instrument has shown strong internal consistency and convergent validity. It is considered the gold standard in measuring family accommodation (Francazio et al., 2016). In this study, Cronbach́s alpha was .90.
Satisfaction Scale (Rosa-Alcázar, Iniesta-Sepúlveda, Parada-Navas, & Rosa-Alcázar, 2012). This self-report measure was developed by the research team to assess satisfaction with the treatment program. It includes 4-items rated in a 4-point Likert scale from 1 (very unsatisfied) to 4 (very satisfied) regarding the following issues: (1) Satisfaction about treatment, (2) Satisfaction with number and duration of sessions, (3) Satisfaction with therapist, and (4) Satisfaction with program outcome.
Adherence treatment: weekly homework accomplishment and attendance at treatment sessions.
TreatmentThe treatment protocol was based on other programs on best practice guidelines and research evidence. This included workbooks for parents and children (Rosa-Alcázar, 2012a, 2012b, 2012c). Treatment is CBFT involving 12 weekly sessions each running for 1 hr. and 1 booster session (3 months post-treatment). The workbook for children contained child-friendly examples, and the concept of OCD was presented metaphorically (i.e., an annoying ball that the child tries to throw away, but which repeatedly comes back). Ten ERP sessions were applied. A summary of the protocol can be requested from the corresponding author. Treatment conditions were:
Group 1: Treatment parents and child. Parents and child carried out the sessions. Exposure tasks at home had to be guided and supervised by parents. These reinforced the achievements of the child. All applied techniques in the intervention were described in manuals provided to parents.
Group 2: Treatment mother and child. In this condition, all the participants were mothers. The mother and child carried out the sessions. ERP at home were guided and supervised by the mother. In this condition, the father was required to read the workbooks with the aim of being able to collaborate in the reduction of responses in Family Accommodation, the control of problems at home and the reinforcement of exposure to fear stimulus or in the worst case not to obstruct the performance of the mother.
Group 3: Treatment mother. All the participants were mothers. These attended the 12 weekly sessions with the psychologist. Treatment was the same but the time invested in the child focussed on instructing and training the mother (Role-playing) on what to be done at home with the child (as in consultation). As in the condition 2, the father was required to read the workbooks to collaborate with the mother in reducing responses to Family Accomodation as in the problematic conduct of the child and reinforcing exposure tasks.
Data analysisChi-square and one-factor ANOVA were used to examine potential group differences in clinical and demographic (age/gender) variables at pretreatment. Two-factor repeated-measures ANOVA was conducted to test the effect of the treatments as a function of time (pre-treatment, post-treatment, and 3-month follow-up) and group (treatment parents-child; treatment mother-child; treatment mother). Results of Greenhouse-Geisser correction were reported Mauchly's test of sphericity was significant. Statistically significant time by condition interactions were followed up by Sidak's post-hoc comparisons. Cohen's ds (standardized mean differences) were calculated to estimate the magnitude of the between-groups differences. To interpret the magnitude of Cohen's ds, they were compared with the meta-analyses on the effectiveness of clinical psychology treatments (Rubio-Aparicio, Marín-Martínez, Sánchez-Meca, & López-López, 2017).
To allow comparisons with previous studies (Piacentini et al., 2011), the clinical remission was defined as a reduction in Total CY-BOCS in four levels: Remitted (CY-BOCS <11), Subclinical (11-15), Moderate (16-24) and Severe (> 24). Group comparisons of remission status were performed using χ2 or likelihood ratio tests. Clinically significant change was based on Jacobson and Truax (1991). All participants were included in the analyses, not missing cases being produced. SPSS Statistic 22.00 was used for statistical analysis.
ResultsAnalysis of group differences at pre-treatmentThe three groups were equivalent with regard to all demographic variables. In particular, no statistically significant differences were found in childreńs age (p=.820), motheŕs age (p=.910), fatheŕs age (p=.430), childreńs gender in group (p=.930), duration of disorder (p=.755), fatheŕs education (p=.560), and motheŕs education (p=.590). In addition, the baseline scores for the outcome variables did not differ significantly between the groups: CY-BOCS total score (p=.954), CY-BOCS obsessions (p=.213), CY-BOCS compulsions (p=.671), CBCL-Externalizing (p=.870), CBCL-Internalizing (p=.062), FAS-mothers (p=.608), FAS-fathers (p=.266), and CGAS (p=.832). Similarly, no differences were found between groups regarding presence of comorbid disorders: Dark phobia (p=.93), Separation anxiety disorder (p=.901), Animal phobia (p=.430) and Mood (p=.581). See Table 1.
The most common obsessions were contamination (56.8%) and aggressive obsessions (52.3%). The compulsions most frequent were involving any person (79.5%), repeating (75%), cleaning/washing (56.8%), and checking/reassurance (54.5%).
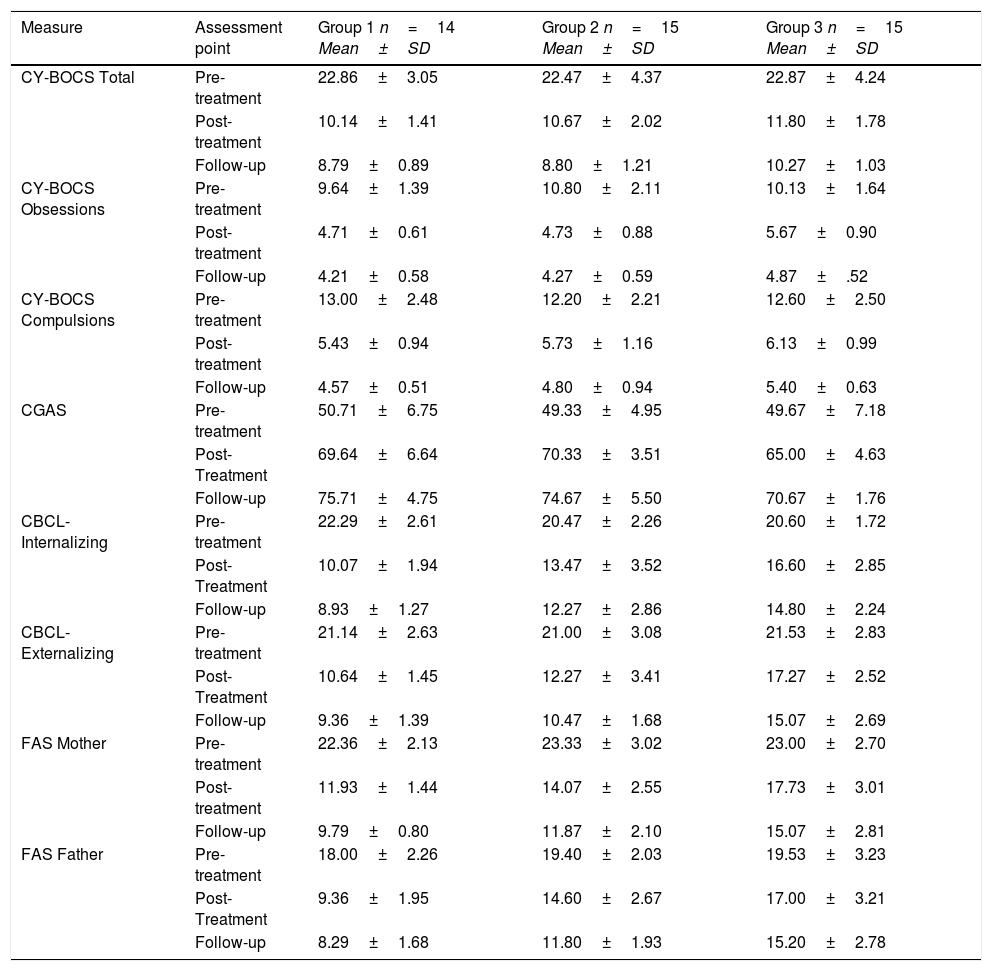
Primary outcome analysisTable 2 presents the means and standard deviations for the three treatment conditions through the three assessment points on the CY-BOCS. The results of the mixed ANOVAs shows a statistically significant time effect for the CY-BOCS total, Obsessions, and Compulsions scores, with a significant improvement in obsessive-compulsive symptoms across assessment points, with a large percentage of variance accounted for (η2 ≥ .93). There were also significant group differences in interaction in CY-BOCS Obsessions (p=.021).
Means and standard deviations CY-BOCS and secondary outcomes.
| Measure | Assessment point | Group 1 n=14 Mean±SD | Group 2 n=15 Mean±SD | Group 3 n=15 Mean±SD |
|---|---|---|---|---|
| CY-BOCS Total | Pre-treatment | 22.86±3.05 | 22.47±4.37 | 22.87±4.24 |
| Post-treatment | 10.14±1.41 | 10.67±2.02 | 11.80±1.78 | |
| Follow-up | 8.79±0.89 | 8.80±1.21 | 10.27±1.03 | |
| CY-BOCS Obsessions | Pre-treatment | 9.64±1.39 | 10.80±2.11 | 10.13±1.64 |
| Post-treatment | 4.71±0.61 | 4.73±0.88 | 5.67±0.90 | |
| Follow-up | 4.21±0.58 | 4.27±0.59 | 4.87±.52 | |
| CY-BOCS Compulsions | Pre-treatment | 13.00±2.48 | 12.20±2.21 | 12.60±2.50 |
| Post-treatment | 5.43±0.94 | 5.73±1.16 | 6.13±0.99 | |
| Follow-up | 4.57±0.51 | 4.80±0.94 | 5.40±0.63 | |
| CGAS | Pre-treatment | 50.71±6.75 | 49.33±4.95 | 49.67±7.18 |
| Post-Treatment | 69.64±6.64 | 70.33±3.51 | 65.00±4.63 | |
| Follow-up | 75.71±4.75 | 74.67±5.50 | 70.67±1.76 | |
| CBCL-Internalizing | Pre-treatment | 22.29±2.61 | 20.47±2.26 | 20.60±1.72 |
| Post-Treatment | 10.07±1.94 | 13.47±3.52 | 16.60±2.85 | |
| Follow-up | 8.93±1.27 | 12.27±2.86 | 14.80±2.24 | |
| CBCL-Externalizing | Pre-treatment | 21.14±2.63 | 21.00±3.08 | 21.53±2.83 |
| Post-Treatment | 10.64±1.45 | 12.27±3.41 | 17.27±2.52 | |
| Follow-up | 9.36±1.39 | 10.47±1.68 | 15.07±2.69 | |
| FAS Mother | Pre-treatment | 22.36±2.13 | 23.33±3.02 | 23.00±2.70 |
| Post-treatment | 11.93±1.44 | 14.07±2.55 | 17.73±3.01 | |
| Follow-up | 9.79±0.80 | 11.87±2.10 | 15.07±2.81 | |
| FAS Father | Pre-treatment | 18.00±2.26 | 19.40±2.03 | 19.53±3.23 |
| Post-Treatment | 9.36±1.95 | 14.60±2.67 | 17.00±3.21 | |
| Follow-up | 8.29±1.68 | 11.80±1.93 | 15.20±2.78 |
Note. Group 1: Parents and child; Group 2: Mother and child; Group 3: Mother; CY-BOCS: Childreńs Yale-Brown Obsessive-Compulsive Scale. CGAS: Children's Global Assessment Scale. CBCL: Child Behavior Checklist, FAS: Family Accommodation Scale.
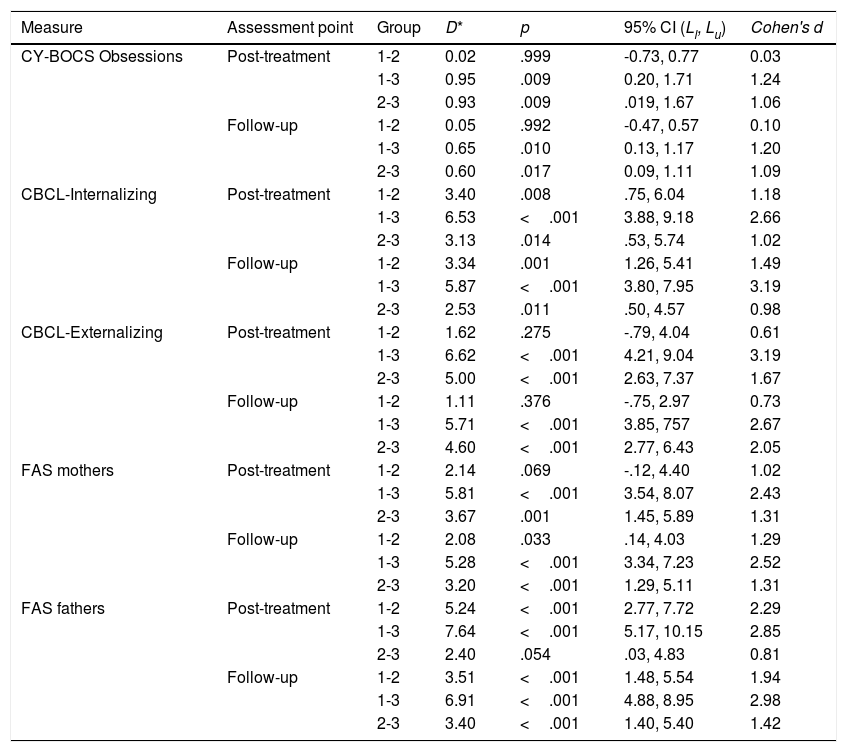
Table 3 shows significant differences between Group 1 vs. Group 3 in post-treatment and follow-up in CY-BOCS Obsessions. In this variable a better result was found from Group 1 vs. Group 3 in post-treatment (d=1.24).
Sidak post-hoc comparisons and effect size.
| Measure | Assessment point | Group | D* | p | 95% CI (Ll, Lu) | Cohen's d |
|---|---|---|---|---|---|---|
| CY-BOCS Obsessions | Post-treatment | 1-2 | 0.02 | .999 | -0.73, 0.77 | 0.03 |
| 1-3 | 0.95 | .009 | 0.20, 1.71 | 1.24 | ||
| 2-3 | 0.93 | .009 | .019, 1.67 | 1.06 | ||
| Follow-up | 1-2 | 0.05 | .992 | -0.47, 0.57 | 0.10 | |
| 1-3 | 0.65 | .010 | 0.13, 1.17 | 1.20 | ||
| 2-3 | 0.60 | .017 | 0.09, 1.11 | 1.09 | ||
| CBCL-Internalizing | Post-treatment | 1-2 | 3.40 | .008 | .75, 6.04 | 1.18 |
| 1-3 | 6.53 | <.001 | 3.88, 9.18 | 2.66 | ||
| 2-3 | 3.13 | .014 | .53, 5.74 | 1.02 | ||
| Follow-up | 1-2 | 3.34 | .001 | 1.26, 5.41 | 1.49 | |
| 1-3 | 5.87 | <.001 | 3.80, 7.95 | 3.19 | ||
| 2-3 | 2.53 | .011 | .50, 4.57 | 0.98 | ||
| CBCL-Externalizing | Post-treatment | 1-2 | 1.62 | .275 | -.79, 4.04 | 0.61 |
| 1-3 | 6.62 | <.001 | 4.21, 9.04 | 3.19 | ||
| 2-3 | 5.00 | <.001 | 2.63, 7.37 | 1.67 | ||
| Follow-up | 1-2 | 1.11 | .376 | -.75, 2.97 | 0.73 | |
| 1-3 | 5.71 | <.001 | 3.85, 757 | 2.67 | ||
| 2-3 | 4.60 | <.001 | 2.77, 6.43 | 2.05 | ||
| FAS mothers | Post-treatment | 1-2 | 2.14 | .069 | -.12, 4.40 | 1.02 |
| 1-3 | 5.81 | <.001 | 3.54, 8.07 | 2.43 | ||
| 2-3 | 3.67 | .001 | 1.45, 5.89 | 1.31 | ||
| Follow-up | 1-2 | 2.08 | .033 | .14, 4.03 | 1.29 | |
| 1-3 | 5.28 | <.001 | 3.34, 7.23 | 2.52 | ||
| 2-3 | 3.20 | <.001 | 1.29, 5.11 | 1.31 | ||
| FAS fathers | Post-treatment | 1-2 | 5.24 | <.001 | 2.77, 7.72 | 2.29 |
| 1-3 | 7.64 | <.001 | 5.17, 10.15 | 2.85 | ||
| 2-3 | 2.40 | .054 | .03, 4.83 | 0.81 | ||
| Follow-up | 1-2 | 3.51 | <.001 | 1.48, 5.54 | 1.94 | |
| 1-3 | 6.91 | <.001 | 4.88, 8.95 | 2.98 | ||
| 2-3 | 3.40 | <.001 | 1.40, 5.40 | 1.42 |
Note. Group 1: Parents and Child; Group 2: Mother and Child; Group 3: Mother; CY-BOCS: Childreńs Yale-Brown Obsessive-Compulsive Scale. CGAS: Children's Global Assessment Scale, CBCL: Child Behavior Checklist, FAS: Family Accommodation Scale. D=Mean difference between the two conditions. * Positive Ds indicated that the group compared in first place reached greater improvements than the group appearing in second place. Ll and Lu: lower and upper confidence limits of 95% confidence intervals around the mean difference.
Table 2 presents the means and standard deviations for the three treatment conditions and assessment points on secondary outcomes. Mixed ANOVAs showed a significant time effect improvement in all outcomes across assessment points, with a large proportion of variance accounted (η2 ≥ .887). In addition, statistically significant differences were found among the three treatment conditions in CBCL-Internalizing (p <.001), CBCL-Externalizing (p <.001), FAS-mother (p <.001), and FAS-father (p <.001), being marginally significant in CGAS (p=.058). Within-group analyses revealed significant decreases in the three treatment conditions in all outcomes, with the largest effect sizes when comparing pre-treatment with follow-up.
Post-hoc comparisons showed significant differences between Group 1 vs. Group 3 in post-treatment and follow-up in all secondary outcome measures (Table 3). Significant differences were also found between Group 2 vs. Group 3 in post-treatment and follow-up in all outcome measures, except for FAS-father post-treatment (p=.54). The comparison between Group 1 vs. Group 2 reached significant differences for CBCL Internalizing in the post-treatment (p=.008) and follow-up (p=.001), for FAS-mother in the follow-up (p=.033) and for FAS-father in the post-treatment and follow-up (p <.001). All effect sizes were of large magnitude (Rubio-Aparicio et al., 2017).
RemissionThe CY-BOCS was chosen as the primary outcome variable as it is a more objective, reliable, and valid instrument compared to others. Clinically significant change at an individual level was defined as two standard deviations below the mean at posttreatment (criteria based on Jacobson & Truax, 1991). Based on these criteria 100% of the sample evidenced clinically significant change from pre to posttreatment on the CY-BOCS.
Nonstatistically significant differences among the three conditions in the pre-treatment were found, χ2 (2)=3.73, p=.155. Statistically significant differences were found between the three treatment conditions on severity categories in the post-treatment, χ2(2)=7.90, p=.019, and follow-up LR(2)=13.65, p=.001, indicating that all participants moved from moderate and severe to in remission or subclinical categories. Group 1 showed the highest remission rates (71.4%) compared to 40% and 20% of Groups 2 and 3, respectively. In follow-up, the remission rates were as follows: Group 1 (100%), Group 2 (93.3%) and Group 3 (53.3%). Post hoc comparisons performed in post-treatment and follow-up showed Group 1 exhibiting larger remission rates than Group 3 in post-treatment (51.4%, χ2(2)=7.74, p=.015) and follow-up (46.7%; χ2(2)=11.33, p=.003). In follow-up, Group 2 showed a significantly greater remission rate than Group 3 (40%, χ2(2)=6.72, p=.030).
Treatment adherence and satisfactionTreatment adherence was evaluated in terms of weekly homework accomplishment and attendance at treatment sessions. The percentage of homework completion was very high (Group 1=95.6%; Group 2=93.8% y Group 3=93.7%), no differences being found among them. Regarding attendance at treatment sessions, two mothers (one from Group 2 and one from Group 3), and one father (Group 1) missed one session for personal reasons.
As for results on Satisfaction Scale, statistically significant differences were found regarding the treatment format, F(2, 43)=23.25, p <.001, and frecuency and duration of sessions, F(2, 43)=35.08, p <.001. There were no differences in satisfaction with the therapist and program outcomes (p> .05). Post-hoc comparisons on “Satisfaction with the format” showed significant diferences between Group 1 vs. Group 3 (p <.001) and Group 2 vs. Group 3 (p=.001). Post-hoc comparisons on frequency and duration of sessions were higher in Group 1 vs. Group 3 (p <.001) and higher in Group 2 vs. Group 3 (p <.001).
Discussion and conclusionsThe main objective was to evaluate the differential efficacy of cognitive behavioral family treatment for children ages 4 to 8 with OCD (Rosa-Alcázar, 2012a, 2012b, 2012c). The protocol used was effective in reducing obsessive-compulsive symptoms and secondary outcomes in post-treatment and follow-up. The three ways of implementation produced clinical improvements and were well-accepted by parents and children, being the first study to carry out these three types of implementation. These results are similar to those observed in previous studies highlighting the importance of ERP and family involvement in these interventions (Comer et al., 2017; Freeman et al., 2014; Lebowitz, 2016; Lewin et al., 2014).
The active inclusion of parents in treatment, acting as co-therapists, has not only allowed the reduction of “Family accommodation”, but also to maintain and generalize achievements (between contexts: from the clinical context to the home, among people: non-attending parents; and over time: increasing improvements in follow-up measures). This study provides follow-up measures only found at these ages in the study by Lewin et al. (2014), maintaining the same improvement trend in both investigations. This is in line with what is recommended, not only for OCD, but also for other psychological disorders (Taboas, McKay, Whiteside, & Storch, 2015). These results agree with those provided by different meta-analytic studies focused on children and adolescents (Choate-Summers et al., 2008, Farrell, Schlup, & Boschen, 2010; Lebowitz, 2016). In particular, Rosa-Alcázar et al. (2015) found that 34% of children improved more when parents were trained as assistants in managing their children's dysfunctional behaviors and performing ERP at home.
Results on the differential efficacy of the three intervention formats lead us to conclude that although there were no intergroup differences in the variables related to the severity of OCD (CY-BOCS), there were some in the following secondary variables: “CBCL-Internalizing/Externalizing” and “Family-Accommodation father and mother”. Nevertheless, to understand the scope of the changes among the groups as regards time, the values ??of the interaction were analyzed, verifying that in “CY-BOCS Obsessions” there was a significant difference between the Parents and child Group, and Mother and child Group compared to the Mother Group. These data indicated that groups including children in direct interventions with the therapist were more effective than those that did not.
These findings are complemented by those found in the study of clinical significance showing that all participants, moved from moderate and severe to remission or subclinical categories of OCD severity, although outstanding was the highest percentage reached in the Parents and child Group compared to Mother Group in post-treatment, maintaining this improvement in follow-up. All in line with what was pointed out by Freeman et al. (2014) and Rosa-Alcázar et al. (2015) on the importance of the involvement of parents in intervention with children and adolescents, therefore it is expected that high parental involvement will be followed by better results, with a high probability.
Regarding clinical significance, the percentages of participants in remission was high across groups, outstanding being the Parents and child Group, in post-treatment (71.4%), similar to others such as Freeman et al. (2014) and superior to those obtained by Lewin et al. (2014), in follow-up at three months. Therefore, our findings lead us to affirm that the psychologist's direct work with the child is essential in the treatment of OCD.
Analysis of results of the secondary variable “CBCL-Internalizing” revealed that the Parents and child Group obtained the best results, followed by the Mother and child Group; In the “CBCL-Externalizing” the same tendency could be observed, but no differences were found between the first groups. These results lead us to consider that in cases where children present internalizing or externalizing problems, their inclusion in direct treatment with the therapist could help to reduce these behaviors. This may be because observation of the psychologist's performance could enhance the security of the parents, by exposing themselves to “Mastery Modeling“, in addition to the fact that the parents could thus better apply ERP (American Academy of Child and Adolescent Psychiatry Committee on Quality Issues, 2012; Cancilliere et al., 2018; Lebowitz, 2016; Wu & Storch, 2016).
Results in Family accommodation indicated that all groups improved in the reduction of the”FAS-fathers and mothers“, therefore, the different formats are effective. These results coincide with others provided on CBFT (Freeman et al., 2014; Lebowitz, 2016; Lewin et al., 2014), although these studies did not separately analyze the measures of”Accommodation of the father and the mother“, therefore, as already indicated, analysis carried out in the present study is novel. In FAS-mother, the Parents and child Group and Mother and child Group achieved best results both in posttest and follow-up. Regarding the behaviors of father accommodation, best results were obtained in the Parents and child group compared to other groups, confirming the need that, in order to increase improvement, the involvement of both parents in the application of treatment is necessary. These data suggest that, despite improving the both parentś accommodation (even if neither the father nor the child attended treatment), the best condition seems to be that where all attend.
Likewise, from the perspective of clinical implications, we can conclude that the implementation of interventions focused on parents of young children with OCD is needed not only to overcome their problem but also to reduce family accommodation, whose existence would constitute an almost insurmountable barrier for effective application of psychological treatment. The direct involvement of the child in the treatment is relevant, both in increasing their motivation and to encourage and intensify the security of parents in the handling of problematic behaviors that may arise during treatment in non-clinical contexts (Pascual-Vera & Belloch, 2018)
There are several study limitations. First, the small and homogenous characteristics of participants in terms of their sociodemographic and clinical profile limit the generalizability of our results. Second, follow-up outcomes are insufficient, i.e., they have a provisional nature and follow-up is required at 6, 12 and 24 months to more rigorously assess the scope of achievement stability.
As future perspectives, we believe it is required to continue increasing the number of subjects with this treatment in its different formats. Likewise, the study of more predictors should be included, increasing sample size; studying relationships between the role of”Parent Accommodation” and different educational styles, couple relation shit problems and other clinical variables such as depression and parental anxiety.
FundingThis article was supported by the Ministerio de Economía and Competitividad of the Spanish Government (Projects No.PSI2016-78185-P).