Although the management of the invasive candidiasis has improved in the last decade, controversial issues yet remain, especially in the diagnostic and therapeutic approaches to Candida peritonitis and other forms of intra-abdominal fungal infections.
AimsWe sought to identify core clinical knowledge about intra-abdominal fungal infections and to achieve high-agreement recommendations required to care for critically ill adult patients with Candida peritonitis and other forms of intra-abdominal fungal infection.
MethodsA biregional Spanish survey, to elucidate the consensus about the already mentioned fungal infections by means of the Delphi technique, was conducted anonymously by e-mail with 29 multidisciplinary experts in invasive fungal infections from 14 hospitals in the Valencia and Murcia communities during 2014. Respondents included intensivists, anesthesiologists, microbiologists, pharmacologists, and infectious disease specialists, who answered 31 questions prepared by a coordination group after a strict review of the literature from the 5 previous years. The educational objectives spanned 6 categories: epidemiology, microbiological diagnosis, clinical diagnosis, antifungal treatment, de-escalation therapy, and special situations. The agreement required among the panelists for each item to be selected had to be higher than 70%. After extracting the recommendations from the selected items, a meeting at which the experts were asked to validate the previously selected recommendations in a second round of scoring took place.
ResultsAfter the second round, 36 recommendations were validated according to the following distribution: epidemiology (5), microbiological diagnosis (4), clinical diagnosis (4), antifungal treatment (3), de-escalation therapy (4), and special situations (16).
ConclusionsTreatment of Candida peritonitis and other forms of intra-abdominal fungal infections in ICU patients requires a broad range of knowledge application and skills that our recommendations address. Based on the DELPHI methodology, these recommendations might help to optimize the therapeutic management of these patients in special situations and in various scenarios to improve their outcome.
Aunque en la última década se ha observado una mejoría en el manejo de la candidiasis invasora todavía existe controversia, especialmente en la aproximación diagnóstico-terapéutica de la candidiasis peritoneal y otras formas de infección fúngica invasora intraabdominal en el paciente crítico no neutropénico.
ObjetivosIdentificar los principales conocimientos clínicos sobre las infecciones fúngicas intraabdominales y elaborar recomendaciones con un alto nivel de consenso, necesarias para el diagnóstico y el tratamiento de la candidiasis peritoneal y otras infecciones fúngicas intraabdominales en pacientes adultos críticos no neutropénicos.
MétodosSe realizó un cuestionario prospectivo en dos comunidades autónomas para estimar mediante la técnica Delphi el consenso en el diagnóstico y tratamiento de las infecciones mencionadas. El cuestionario se realizó en el año 2014, de forma anónima y por correo electrónico, con 29 expertos de varias disciplinas, especialistas en infecciones fúngicas invasivas de 14 hospitales de la Comunidad Valenciana y Murciana, entre los que se incluían intensivistas, anestesistas, microbiólogos, farmacéuticos y especialistas en enfermedades infecciosas, que respondieron a 31 preguntas preparadas por el grupo de coordinación, tras una revisión exhaustiva de la literatura de los 5 años previos. Los objetivos educativos contemplaron 6 categorías que incluían epidemiología, diagnóstico microbiológico, diagnóstico clínico, tratamiento antifúngico, desescalado del tratamiento farmacológico y situaciones especiales. El nivel de acuerdo alcanzado entre los expertos en cada una de las categorías debía superar el 75% para ser seleccionada. En un segundo término, después de extraer las recomendaciones de los temas seleccionados, se celebró una reunión presencial con 29 especialistas y se les solicitó la validación de las recomendaciones preseleccionadas.
ResultadosDespués de la segunda ronda, 36 recomendaciones fueron validadas siguiendo la siguiente distribución: epidemiología (5), diagnóstico microbiológico (4), diagnóstico clínico (4), tratamiento antifúngico, (3), desescalado (4) y situaciones especiales (16).
ConclusionesEl manejo de la peritonitis candidiásica en pacientes de UCI requiere la aplicación de los conocimientos y destrezas que se detallan en nuestras recomendaciones. Estas recomendaciones, basadas en la metodología DELPHI, ayudan a optimizar el tratamiento de los pacientes críticos con candidiasis invasiva en distintos escenarios y situaciones clínicas y a mejorar su pronóstico.
Invasive fungal infections have been increasing worldwide in recent decades. Intra-abdominal candidiasis (IAC), which includes peritonitis and intra-abdominal abscesses, occur in approximately 40% of patients following repeat gastrointestinal (GI) surgery, GI perforation, or necrotizing pancreatitis. It is the predominant invasive candidiasis (IC) after candidemia in intensive care units (ICUs), with approximately 25–60% mortality rates.9,41,55 In immunologically competent patients, IAC normally stems from gastrointestinal barrier breaches, causing a confined or diffuse spread of fungi in the abdominal cavity. However, the pathological importance of intra-abdominal Candida isolation is not clear in many clinical situations. In patients with perforation of hollow viscera or with intra-abdominal surgical drains, the recovery of bacteria along with Candida in peritoneal fluid samples is common, and the role of Candida as a pathogen, co-pathogen, or innocent spectator is undefined.52
Fungal etiology accounts for at least 12% of all cases of intra-abdominal infection. Candida is the most common cause of fungal peritonitis, whereas other fungi, such as Aspergillus, Paecilomyces, Penicillium, and Zygomycetes, are infrequent protagonists of intra-abdominal fungal infections (IAFI). Although Candida albicans remains the most frequent yeast causing intra-abdominal infection, a shift toward other Candida species, such as Candida glabrata, Candida parapsilosis, Candida tropicalis, Candida krusei, and Candida lusitaniae, has been observed (some of them with reduced susceptibility to antifungal drugs).42
Despite its high incidence in surgical ICUs (59.1% of all IC),3 the etiological diagnosis of non-candidemic IC remains elusive. Neither the guidelines from the Infectious Diseases Society of America (IDSA) nor the European consensus (ESCMID) provide any clarification on IAC diagnosis.13,46
The high mortality associated with IAC could be related to diagnostic problems, such as the low sensitivity and specificity of both culture- and non-culture-based techniques. It is also still unclear which patients could benefit from empiric antifungal treatment and which might be infected by fluconazole-resistant strains; IAC has recently been described as a hidden reservoir of echinocandin-resistant Candida.57 In recent years, new antifungal agents have offered various alternatives in the treatment of IC. However, the most effective therapeutic strategy for IAC has not yet been established, resulting in a remarkable lack of consensus when establishing the diagnosis and the most appropriate treatment for this patient population.
We aimed to achieve a consensus on the clinical and therapeutic management of peritoneal candidiasis (PC) based on the Epico strategy.37,64–66
MethodsA panel of 29 specialists from 14 hospitals in the Valencia and Murcia communities (Annex 1) with wide experience in the treatment of critically ill patients were asked to vote on and validate the recommendations previously established by the 6 coordinators (Annex 2) responsible for the research.
The criteria for inclusion were based on the participants’ experience with the clinical management of critically ill patients with a suspected or confirmed IAFI. The DELPHI technique was used to perform the study with the objective of optimizing the consultation process of the panel members. Specifically, the DELPHI methodology enables to consider group opinions, not merely individual opinions, from experts in the different medical items provided by the coordinators. A consensus of the experts greater than 70% (21–29) in Top 3 (score of 7 or more points) was required to finally consider each item as a recommendation. In those cases in which the majority of the responses to a given question were shared by 15–20 participants, the degree of consensus was established as medium, whereas in those cases in which consensus was only shared by 15 or fewer experts, the degree of consensus was defined as low.
The study was performed in three phases. Initially the coordinators responsible for the systematic search of the literature established 31 questions distributed in 6 categories: (1) epidemiology, 5 questions (developed by J.P. and D.N.); (2) microbiological diagnosis, 4 questions (developed by J.P. and D.N.); (3) clinical diagnosis, 6 questions (developed by R.Z. and J.C.V.); (4) antifungal treatment, 5 questions (developed by R.Z. and G.A.); (5) de-escalation therapy, 4 questions (developed by J.C.V. and M.S.); and (6) special situations, 7 questions (developed by M.S. and G.A.). In the cases in which no consensus was reached, the experts detailed the reasons for the divergent opinions. Afterwards, the panel of 29 experts voted anonymously the different questions in a face-to-face meeting held on October 17–18, 2014. All the participants validated the final list of recommendations.
ResultsEpidemiology1. Intra-abdominal yeasts are frequently isolated after gastro-duodenal and small intestine perforations, which is uncommon in biliary tract perforations and rare after colorectal and appendix perforations.RationaleThe isolation of Candida spp. in the peritoneal fluid varies depending on the anatomical location of the digestive tract rupture. Its incidence is higher (41%) in high gastrointestinal perforations (above the angle of Treitz) than in colorectal and appendicular perforations (18%).15,55 Yeast can be isolated with clinical significance from the abdominal specimens of patients with complicated gastrointestinal perforations that require multiple surgical procedures to be repaired.8,24
All the experts consulted confirmed that the isolation of Candida species in the peritoneal fluid varies with the anatomical location of the digestive tract breach. Specifically, and based on a 0–9 point scale, in which 9 represents the maximum level of agreement, 29 experts granted 7 or more points to this concept. The average score was established at 7.92 points, and the consensus level was 100%.
2. The risk factors more specifically related to Candida peritonitis (CP) are recurrent abdominal surgery (including laparoscopy), gastrointestinal perforation (especially recurrent, or perforations not treated within the first 24h) and leakages of gastrointestinal anastomosis (primarily in the upper digestive tract).RationaleAny type of surgery with gastrointestinal anatomical barrier disruption facilitates the seeding of the peritoneal cavity with yeasts from the digestive tract. Upper gastrointestinal perforations (and anastomotic leakages) cause a seeding of the peritoneal cavity with yeasts in 50% of patients. The development of a subsequent peritonitis increases the risk of CP up to 11 times.15,24
All the expert panel members highlighted that recurrent abdominal surgery, gastrointestinal perforation, and leakages of gastrointestinal anastomosis are risk factors specifically related to CP. Specifically, and based on a scale of 0–9 points, the 29 experts granted 7 or more points to these risk factors. The average score was 8.0 points. The degree of consensus reached by the experts was high (100%).
3. Less specifically, CP has also been associated with prior colonization by Candida, tertiary peritonitis, severe sepsis or septic shock, acute necrotizing pancreatitis, postoperative paralytic ileus, parenteral nutrition, nosocomial peritonitis, long stay in the ICU, proton pump inhibitor therapy, and prolonged antibacterial therapy (>5 days).RationaleColonization by Candida is one of the most verified predictors of the development of IC. Tertiary peritonitis with multiple surgeries (often associated with prolonged antibacterial treatments) and any peritonitis associated with severe sepsis or septic shock significantly increases the risk of CP. Acute necrotizing pancreatitis (with significant destruction of pancreatic tissue and adjacent structures) is also associated with high risk of CP, particularly if it is associated with prolonged antibiotic therapy (>5 days) and/or abdominal surgery. Postoperative paralytic ileus and total parenteral nutrition greatly increase the risk of colonization by Candida, mucosal atrophy, and CP development in critically ill patients. Furthermore, a prolonged stay in the ICU is a recognized risk factor for colonization and infection by Candida; this risk is increased by the multiple breaches of skin and mucous barriers that critically ill patients experience. Proton pump inhibitors and histamine-2 receptor antagonists also facilitate colonization of the gastrointestinal tract by Candida and, consequently, a predisposition toward Candida intra-abdominal infections after recent abdominal surgery.15,24,41
Approximately 87% of the experts consulted agreed that CP is less specifically associated with prior colonization by Candida spp., tertiary peritonitis, severe sepsis or septic shock, acute necrotizing pancreatitis, postoperative paralytic ileus, parenteral nutrition, nosocomial peritonitis, long stay in the ICU, proton pump inhibitor therapy, and prolonged antibacterial therapy (>5 days). Specifically, and using a 0–9 point scale, 29 experts granted 7 or more points to this statement. The average score was 7.29 points and the degree of consensus was high (>70%).
4. Isolation of Candida strains non-susceptible to fluconazole is usually associated with previous treatment with azole agents, age>65 years, hospital stay>30 days, and gastrointestinal surgery in the previous month.RationaleIn adult patients with neoplastic disease, risk factors for developing an IC by Candida isolates resistant (or least susceptible) to fluconazole include pretreatment with systemic triazoles, age>65 years, length of hospital stay>30 days, and gastrointestinal surgery in the 30 days before the previous IC episode.30,59
The majority of the specialists consulted (76.1%) agreed that the isolation of fluconazole-non susceptible Candida strains is associated with a previous treatment with azole agents, age>65 years, hospital stay>30 days and gastrointestinal surgery in the previous month. With 9 points as the highest score and 0 the lowest, 22 experts granted 7 or more points to the importance of identifying the risk factors associated with possible therapeutic failure. The average score was 6.92 points and the degree of consensus achieved was high (>70%).
5. The hospital acquisition of CP with Candida isolation in the peritoneal fluid, the presence of severe sepsis or septic shock, and the occurrence of a spontaneous perforation in an already hospitalized patient have been described as factors associated with increased mortality in patients with intra-abdominal candidiasis.RationaleThe isolation of intra-abdominal yeasts during surgery, severe ongoing disease, and any type of gastrointestinal perforation during hospital stay are associated with a significant increase in mortality of patients with CP. In addition, the isolation of yeasts in sterile liquids has been associated with ICU admission, increased dependence on mechanical ventilation, and need for central venous catheter (risk factors related to IC).41,42,55
The majority of the experts consulted (86%) highlighted the importance of intra-abdominal yeast isolation during surgery, the presence of severe sepsis or septic shock, and the occurrence of a spontaneous perforation in an already hospitalized patient as risk factors associated with poor outcome. Specifically, and based on a 0–9 scale, in which 9 represents the maximum level of importance, 25 experts granted 7 or more points to the importance of identifying these risk factors. The degree of consensus reached was high (>70%) and the average score was established at 7.04 points.
Microbiological diagnosis1. If CP is suspected, the most suitable clinical samples for direct microscopical examination and mycological culture are necrotic or purulent specimens collected during surgery or by percutaneous aspiration (alternatively, samples obtained by drainage can also be valid, but only those taken in the first 24h post-implant). Blood cultures are rarely positive for CP.RationaleThe meaning of Candida isolation in the abdominal cavity is controversial, particularly in the context of polymicrobial infections. In fact, there is no gold standard for CP diagnosis. There are not even consistent criteria to discriminate between colonization and infection. A diagnosis of CP is commonly based on the observation of structures compatible with or on the isolation of Candida spp. from the samples stated above in high-risk patients. Therefore, when CP is suspected, samples of peritoneal fluid should be collected in the operating room for culture along with 1 or 2 sets of blood cultures. Samples obtained through drainage tubes after the first 24h post-implantation are neither representative nor valuable for CP diagnosis (they are only useful for studies of colonization).7,18,40,60
The vast majority of the experts consulted (96.1%) agreed that necrotic or purulent specimens collected during surgery or by percutaneous aspiration are the most suitable samples for microbiological diagnosis of CP. Specifically, and based on a 0–9 scale, in which 9 represents the maximum level of importance, 28 experts granted 7 or more points to these clinical samples as the most appropriate for CP microbiological diagnosis. The degree of consensus was high (>90%), and the average score was 7.92 points.
2. To facilitate the recovery of yeasts in culture, a minimum 1ml of abdominal fluid or 1g of necrotic tissue should be inoculated in the medium. The usual culture media for the isolation of yeasts are Sabouraud-chloramphenicol agar and blood culture bottles designed for this purpose (Mycosis-IC-F®, Bactec-Becton Dickinson), although the majority of the species involved grow easily in the blood culture bottles used for bacteria.RationaleThe diagnostic sensitivity of the mycological culture is directly related to the amount of sample inoculated in the media. Therefore, when a CP is suspected, whenever possible, a minimum amount must be collected and inoculated onto the culture media: at least 1ml of abdominal fluid or 1g of tissue. Due to the easy growth of yeasts in the current blood culture bottles (designed to recover bacteria), it is not essential to use bottles specifically designed for fungi recovery. To increase the diagnostic sensitivity of blood culture in disseminated candidiasis, the correct blood volume inoculated into each bottle (recommended by the manufacturer) is more important than the model or type of blood culture bottle used.5,24,52
All the experts consulted agreed that the diagnostic sensitivity of the mycological culture is directly related to the amount of sample inoculated in the media. Specifically, based on a 0–9 scale, in which 9 is of utmost importance, 29 experts granted 7 or more points to this fact. The average score was 8.29 points and a high degree of consensus was achieved (100%).
3. All the yeasts isolated in the peritoneal fluid must be identified to the species level; afterwards, an antifungal susceptibility study should be performed.RationaleThe species isolated from all organic liquids must always be identified, and an antifungal susceptibility study is advisable in all the isolates in these samples. However, thanks to recent epidemiological studies performed in our country, the antifungal susceptibility of most isolated species is predictable; consequently, it is always necessary to identify the isolated species.13,24
All the experts consulted confirmed the need to identify all the yeasts isolated in peritoneal fluid to the species level and the need to perform antifungal susceptibility tests on all these isolates. Specifically, and using a 0–9 point scale, the 29 experts granted 7 or more points to this approach. The average score was 8.6 points and the degree of consensus achieved was high (100%).
4. The quantification of beta-d-glucan in serum can be useful in the diagnosis of CP. Molecular techniques are more sensitive than direct microscopic examination and culture for the detection of Candida in peritoneal fluid, but their diagnostic value has not been sufficiently evaluated. These techniques, along with the detection of mannan antigen, anti-mannan antibody, and C. albicans germ tube antibody (CAGTA), are useful to rule out CP by its high negative predictive value.RationaleIn a recent study, Tissot et al. observed that levels of beta-d-glucan>82.6pg/ml in serum were significantly associated with CP (p=0.002).61 Detection of nucleic acids by molecular techniques, although more sensitive than direct microscopic examination and mycological culture, cannot today replace conventional diagnosis of IC. It is necessary to define the positive predictive value of fungal DNA detection in peritoneal fluid in the absence of Candida spp. in culture. The detection of mannan antigen, anti-mannan antibodies, and CAGTA are useful to rule out CP by their high negative predictive value.7,11,40,54
The vast majority of the specialists consulted (89.6%) agreed on the usefulness of beta-d-glucan quantification in serum in the diagnosis of CP and the utility of mannan antigen, anti-mannan antibody, and CAGTA detection to rule out CP due to their high negative predictive value. The degree of consensus achieved was high (>75%), and the average score was 7.5 points.
Clinical diagnosis1. CP should be ruled out in every patient after intra-abdominal surgery due to a gastrointestinal perforation.RationaleAlthough its correlation with the presence of infection is uncertain, the presence of yeasts in the intra-abdominal fluid is common after a gastrointestinal perforation.41,55
Eighty-nine percent of the experts consulted agreed there is an increased risk of CP after intra-abdominal surgery to repair a gastrointestinal perforation. Specifically, and using a 0–9 point scale, the 26 experts granted seven or more points to this approach. The average score was 6.8 points, and a high degree of consensus was achieved (>75%).
2. The presence of multifocal Candida colonization is useful for CP diagnosis.RationaleIt is accepted in the literature that multifocal colonization by Candida predicts both IC and CP, whereas in the pathophysiology of CP, the presence of multifocal Candida colonization might be not related to its development and other determining factors could be involved.7,40
A majority of the experts (79%) consulted agreed that the multifocal isolation of Candida in critically ill patients predicts both IC and CP. Specifically, three experts did not consider multifocal colonization in any case, whereas three confirmed that they could consider this risk factor only in certain specific cases.
3. The Dupont Score should be used to predict a CP episode.RationaleThe Dupont Score is a predictive score that considers four independent risk factors (with the same weight) to predict the isolation of yeasts in the peritoneal fluid of critically ill surgical patients: female sex, peritonitis secondary to perforation of the upper digestive tract, hemodynamic instability during surgery, and prior antibiotic treatment in the last 48h. The presence of at least 3 of these factors is associated with a high rate of yeast detection, with a sensitivity of 84%, a specificity of 50%, and positive and negative predictive values of 67% and 72%, respectively.7,18
None of the experts consulted considered the Dupont Score useful to predict an episode of CP in critically ill patients. Specifically, and based on a 0–9 scale, in which 9 represents the maximum level of importance, the 29 experts granted 4 or fewer points to this clinical score as a prediction rule of CP. The average score was 3.22 points, with a high degree of consensus (100%).
4. The Ostrosky rule must be used to predict a CP episode.RationaleThe Ostrosky score is a clinical prediction rule designed and validated to identify patients in clinical trials at risk for IC; however, the rule only applies to less than 10% of patients in ICUs. It is a score with low sensitivity (34%) and positive predictive value (10%), and high specificity (90%). The rule was created to detect patients at high risk for IC in the intensive care setting, although very few patients with CP were included for its validation.7,45
Only 62% of the panel members considered the Ostrosky rule useful to predict a CP in critically ill patients. Specifically, on a scale of 1–9 points, in which 9 represents the maximum level of agreement, 18 experts granted 7 or 8 points in favor. The average score was established at 5.9 points, and a low degree of consensus was achieved (<70%).
5. The Candida score must be used to predict a CP episode.RationaleAfter abdominal surgery, critically ill patients with a Candida score ≥3 are correlated with high incidence of IC (up to 33%). However, as occurred with the Ostrosky rule, few patients (less than 30%) with CP were included in the validation study.32,33
Only 3 of the total 29 panel specialists consulted (10.3%) did not consider the Candida score useful to predict CP in critically ill patients after abdominal surgery. Specifically, and using a scale of 0–9 points, in which 9 represents the greatest level of importance, 89.7% of the experts granted 7 or more points to the statement. An average of 7.44 points was established, achieving a high consensus (>70%).
6. The colonization corrected index must be used to predict a CP episode.RationalePrevious isolation of Candida from several body sites appears to be one of the best predictors of IC in high-risk surgical ICU patients.19 Pittet et al. showed that the intensity of colonization by Candida spp. was significantly related to the risk of proven candidiasis.49 The colonization corrected index (CCI) (ratio of highly positive samples/total number of samples analyzed) was described in surgical patients, and demonstrated that a CCI>0.4 has a high positive predictive value (100%) for the development of IC. Furthermore, early fluconazole pre-emptive treatment in patients with a CCI>0.4 decreased the incidence of candidemia, although this study included a small number of patients with CP.48,66
Ninety percent of the experts consulted agreed that using the CCI to predict a CP episode was useful. Specifically, and using a scale of 0–9 points, in which 9 represents the greatest level of importance, 89.6% specialists granted 7 or more points to the statement. An average of 7.29 points was established, with a high degree of consensus (>70%).
Treatment1. Due to the poor prognosis of CP, the adequate control of the infectious source, together with an early and appropriate antifungal treatment, is recommended.RationaleThe mortality rate associated with CP is very high, ranging from 20% to 70%. There is some debate regarding the meaning of positive peritoneal fluid cultures for Candida and whether antifungal therapy reduces mortality rates. Various studies on patients with IC have revealed that early and appropriate antifungal therapy in patients with adequate control of the focus reduces mortality.29,65
The majority of the experts (82.7%) agreed that the control of the infectious focus, together with an early and appropriate antifungal treatment, are determining factors in a favorable outcome of CP. Specifically, 24 of the 29 specialists stated that they “fully or broadly agreed” with the statement, and a high level of consensus was achieved (>80%).
2. Starting an empirical antifungal treatment is recommended in patients with perforation of the upper digestive tract (a) having community-acquired CP with risk factors for colonization by Candida and shock or severe sepsis; or (b) in cases of secondary nosocomial peritonitis with shock, severe sepsis, or tertiary peritonitis.Rationale(a) There is no evidence in the literature that clearly supports the use of an empirical antifungal therapy in patients with perforation of the upper digestive tract and community-acquired CP. (b) The literature lacks sufficient evidence recommending the routine use of empirical antifungal treatment, even in high-risk patients and in those with secondary peritonitis acquired in the community. However, there is some evidence suggesting that patients with nosocomial CP or tertiary peritonitis have increased mortality rates in comparison with patients with community-acquired CP. Therefore, the starting of empirical therapy in patients with secondary nosocomial peritonitis or tertiary peritonitis should be considered, given that any Candida isolation worsens the prognosis.7,41,65
With respect to question 2a, the majority (79.3%) of the experts consulted considered starting an empirical antifungal treatment very important in patients with perforation of the upper digestive tract with community-acquired CP and with risk factors for Candida colonization, shock, or severe sepsis. Specifically, based on a scale of 0–9 points, in which 9 represents the highest level of importance, 23 experts granted 7 or more points to this statement.
Regarding question 2b, all the panel members considered prescribing empirical therapy in patients with upper digestive tract perforation and community-acquired CP (a risk factor for Candida colonization), and shock or severe sepsis. Specifically, and using a scale of 0–9 points, in which 9 represents the greatest level of importance, all the specialists granted 7 or more points to this statement, achieving an average of 8.33 points. A high level of consensus was reached (>70%).
3. Starting an early antifungal treatment in patients with positive non-culture-based microbiological techniques is recommended (BDG, CAGTA, mannan-antimannan, or DNA detection).RationaleThe combination of traditional diagnostic methods with non-culture-based microbiological tools could improve the diagnosis of IC in critically ill patients. To date, the published results on the detection of beta-d-glucan, galactomannan, mannan, and antimannan, C. albicans germ tube antibodies or DNA are promising and could be useful for determining an early antifungal treatment. In general, screening once or twice a week in surgical critically ill patients after 5–7 days of hospitalization is recommended.7,11,47,50
All the experts consulted agreed that non-culture-based methods were not useful to determine the prescription of an early antifungal treatment. Specifically, based on a scoring scale of importance from 0 to 9 points, the 29 experts granted 5 or fewer points to the need for this microbiological diagnosis. The average score was 2.07 points. A high degree of consensus was reached (Bottom 4>70%).
4. In patients with a CP episode, an echinocandin is recommended when the patient is unstable, has previously received azole therapy, or when a fluconazole-resistant Candida is isolated in the peritoneal fluid obtained by surgical procedures.RationaleThere is evidence in the literature that demonstrates that echinocandins can reduce mortality compared with other antifungal agents (27% vs. 36%).4,34 Consequently, echinocandins should be considered the first choice treatment of CP due to their demonstrated efficacy in clinical trials, their broad spectrum of activity, their fungicidal activity, and low toxicity, as recommended by the ESCMID and IDSA guidelines.10,46 There are no studies in the literature that demonstrate a superior response to that of echinocandins in the treatment of patients with CP.7,65 However, low-to-moderate penetration of micafungin into the peritoneal fluid after the first dose has been observed in the only pharmacokinetic study of echinocandins in critically ill patients with proven or suspected CP.21
The panel experts reached full consensus regarding the selection of echinocandins as empirical treatment for a CP episode if the patient is unstable, has previously received azoles, or when a fluconazole-resistant Candida is isolated in the peritoneal fluid obtained by a surgical procedure. Based on a scale of 0–9 points, in which 9 represents the greatest level of importance, 100% of the specialists awarded 7 or more points to the empirical administration of echinocandins in this clinical scenario.
Spectrum reduction of the antifungal treatment1. In patients with CP treated empirically with any echinocandin, consider de-escalation of treatment if there is no diagnostic confirmation by the fifth day of antifungal therapy and the patient is clinically stable.RationaleSusceptibility patterns to antifungal agents vary depending on the Candida species. C. albicans, C. tropicalis, and C. parapsilosis are usually susceptible to fluconazole, whereas C. glabrata susceptibility is generally dose-dependent or resistant, and C. krusei is intrinsically resistant. Thus, identification of the species and determining its susceptibility to the antifungal agents are essential to optimize the antifungal treatment, including de-escalation to fluconazole. In candidemia there are several markers that allow us to decide on this matter, but not in intra-abdominal fungal infections. Antifungal treatment for CP is frequently prescribed based only on clinical suspicion or risk scores. Thus, it is reasonable to suspend any antifungal treatment if you rule out a CP diagnosis and the patient is clinically stable.7,10,40,46
The majority of the experts consulted (75.8%) agreed on starting a de-escalation treatment to fluconazole if there is no diagnostic confirmation by the fifth day of antifungal therapy and the patient is clinically stable. Specifically, 22 of the 29 specialists stated that they “fully or broadly agreed” with the statement, achieving a high level of consensus (Top 2, 80%).
2. In intra-abdominal fungal infection, biomarkers cannot help to establish a decision on the de-escalation of the treatment.RationaleAntifungal de-escalation should be guided by microbiological results. In candidemia there are certain microbiological studies (blood cultures) or even biological markers that can help to assess the response to the treatment. However, this situation cannot be applied to intra-abdominal fungal infections.7,40,61
The majority of the panel experts (75.8%) agreed that biomarkers cannot help to establish a decision on the de-escalation treatment of intra-abdominal fungal infections. Specifically, and using a scale of 0–9 points, in which 9 represents the greatest level of importance, 22 specialists granted 7 or more points to this statement, achieving an average of 7.09 points.
3. In patients with proven CP treatment, de-escalation to an azole after 5–7 days of treatment must be performed if the patient is clinically stable and the isolated Candida species is susceptible to azoles.RationaleTo achieve the maximum effectiveness in the use of antimicrobials, reducing the adverse effects and administering a cost-effective treatment, we must ensure that the prescribed antifungal therapy is the appropriate, but also de-escalate when possible in terms of antimycotic efficacy and thus reduce costs. In intra-abdominal infections by Candida, the same de-escalation criteria used in candidemia must be applied. Various guidelines and a recent consensus recommend this de-escalation decision in the conditions expressed.7,10,46,56
The vast majority of the experts consulted (89.6%) recommended considering de-escalating to fluconazole after 5–7 days in patients with proven CP if the patient is clinically stable and the isolated Candida species is susceptible to azoles. Specifically, based on a scale of 1–9 points, in which 9 represents the maximum level of agreement, 26 experts granted 7 or more points to this statement, achieving an average of 7.68 points.
4. The drugs of choice to de-escalate antifungal treatment in CP are intravenous azole agents, as long as the isolated species of Candida is susceptible and the patient is clinically stable.RationaleFor CP, the various recommendations for candidemia could be applied. In a patient treated initially with an echinocandin or liposomal amphotericin B, the de-escalation to an azole (fluconazole or voriconazole) should be the first choice. Given the special characteristics of the patient subjected to abdominal surgery, the antifungal should be administered intravenously.7,10,40,46
All the experts consulted (100%) considered intravenous azoles as the drugs of choice to de-escalate antifungal treatment in CP, if the isolated species of Candida is susceptible and the patient is clinically stable. A high degree of consensus was reached (Top 2, 90%).
Special situations1a. Acute necrotizing pancreatitis, with criteria of severity, is a special high-risk situation for developing fungal intra-abdominal infection.RationaleSevere necrotizing pancreatitis is included as a common risk factor for development of IC. Almost one-third of patients with recurrent gastrointestinal perforation, anastomotic leaks, or acute necrotizing pancreatitis developed intra-abdominal IC. The classic prospective study of Calandra et al. showed that the primary risk factors for intra-abdominal candidiasis are recurrent gastrointestinal perforations, anastomotic fistula, splenectomy, and acute pancreatitis. Other authors also recognized severe necrotizing pancreatitis among the risk factors for Candida peritonitis, including abdominal viscera perforation, intestinal suture dehiscence-associated peritonitis, or the presence of a peritoneal dialysis catheter.8,39,51
All the panel members agreed that acute necrotizing pancreatitis with criteria of severity is a special high-risk situation for developing fungal intra-abdominal infection. Specifically, and using a scale of 0–9 points, in which 9 represents the greatest level of importance, 26 specialists granted 8 or 9 points to this statement. The average score was established at 8.24 points, and the consensus level achieved was high (Top 2>90%).
1b. Risk of fungal infection, especially by the genus Candida, in the context of an acute necrotizing pancreatitis should be evaluated by scales/scores and/or biomarkers.RationaleThe incidence of intra-abdominal candidiasis in the context of an acute necrotizing pancreatitis is variable and ranges between 5% and 68%, according to various studies. The wide variation could be attributable to the disparities in the selection of patients, the methodology, and the diagnostic criteria applied in the various series. In a well-selected population of critically ill patients, the incidence of Candida peritonitis in patients with acute necrotizing pancreatitis is approximately 18–20%. Microbiological cultures of intra-abdominal samples directly obtained during surgery through punctures, computed tomography guided catheters, or during endoscopic resection of necrotic tissues play a relevant role in the Candida peritonitis diagnosis because Candida species are quickly cleared from blood; therefore, routine blood cultures are not always positive. Given the delay in implementing early antifungal empirical treatment is associated with increased morbidity and mortality, it is desirable to identify patients at increased risk of invasive fungal infection. As a result, several risk scores and biomarkers have been developed, but their utility in patients with acute necrotizing pancreatitis has not been established. In this scenario, the Candida colonization index score could be the most accurate and discriminative test to identify patients with severe acute pancreatitis at risk of developing Candida infection.23,39,62
The majority (93.1%) of the experts consulted agreed it is important to evaluate the risk of Candida infection in the context of an acute necrotizing pancreatitis by scales/scores and/or biomarkers. Specifically, based on a scale of 0–9 points, in which 9 represents the highest level of importance, 27 experts granted 7 or more points to this statement. The average score was 7.4 points, with a high level of consensus reached (>90%).
1c. Universal antifungal prophylaxis is not recommended for all cases of acute necrotizing pancreatitis, although it should be administered in those with severe pancreatitis with increased risk of IC.RationaleAlthough various authors have proposed antifungal prophylaxis during acute necrotizing pancreatitis, their prophylactic use in critical patients remains a subject of great controversy that is thus far unresolved. The IDSA's recent guidelines have recommended the use of fluconazole for the prevention of IC only in ICU surgical patients at high risk of intra-abdominal candidiasis. Therefore, the most appropriate conclusion on this issue is included in the recommendations of the European consensus on intra-abdominal IC: in patients with recurrent gastrointestinal surgery or anastomotic fistula leaking, fluconazole prophylaxis should be considered (recommendation grade B-I), but there is no explicit mention of acute necrotizing pancreatitis; candins could be considered if there is a high probability of azole resistance (C-II).7,46
A vast majority of the specialists consulted (86.2%) agreed that universal antifungal prophylaxis for all cases of acute necrotizing pancreatitis should not be recommended, although in patients with severe pancreatitis and a high risk of IC, antifungal prophylaxis should be administered. The degree of consensus achieved was high (>80%), and the average score was 7.21 points.
2a. In patients with intra-abdominal fungal abscesses, the control of the infectious focus to reduce the fungal inoculum must be achieved by percutaneous or surgical drainage.RationaleIntra-peritoneal abscesses are purulent collections surrounded by fibrous walls that can be produced by expansion of localized inflammatory processes (appendicitis, diverticulitis, cholecystitis, pancreatitis), abdominal trauma, or previous abdominal surgery complications. They are polymicrobial infections, including Gram-negative bacteria, Gram-positive bacteria, anaerobic bacteria, and yeasts. An association between the type of infectious focus control and the mortality of the patients infected by Candida has been observed. The conventional treatment of these abscesses has typically been surgical drainage. However, successful treatments have also been achieved with punctures and drainage by percutaneous catheters guided by radiological techniques (primarily ultrasound scanning and computed tomography scan), and they are the preferred option according to some therapeutic guidelines when compared with surgical drainage (category B-II).7,41,60
Full consensus was reached when percutaneous or surgical drainage were considered the adequate procedures for controlling the infectious focuses in patients with intra-abdominal fungal abscesses. Specifically, based on a scale of 0–9 points, in which 9 represents the highest level of importance, all the experts granted 8 or 9 points to this statement, and the average score was 8.9 points.
2b. Medical instrumentation or surgery should be the procedures for managing fungus balls in the nephro-urological tract when tract obstruction is present.RationaleObstruction due to fungus balls at any level of the urinary tract can be detected using imaging techniques, especially echography. Revealing the obstruction is essential, because antifungal treatment alone will rarely be effective if the obstruction is not resolved. Treatment of fungus balls in the urinary tract usually requires combined strategies: an aggressive surgical treatment with debridement, and the addition of intravenous systemic antifungal treatment (high doses of fluconazole or amphotericin B, the latter with or without flucytosine). Percutaneous nephrostomy allows irrigation with antifungals to achieve high local concentrations and fungal mass reduction.1,27 In the recently published IDSA guidelines, surgical intervention is strongly recommended for adults (strong recommendation; low-quality evidence). Furthermore, irrigation through nephrostomy tubes, if present, with amphotericin B deoxycholate (25–50mg in 200–500ml sterile water) is also recommended (strong recommendation; low-quality evidence).46
All the panel members agreed that the treatment for Candida urinary tract infection associated with fungus balls must be performed by means of medical instrumentation or surgery when obstruction of the nephro-urological tract is present. Specifically, and using a scale of 0–9 points, in which 9 represents the greatest level of importance, 26 specialists granted 8 or 9 points to the statement. The average score was established at 8.63 points, and the consensus level was high (Top 2, 100%).
3a. Chronic disseminated candidiasis (or hepatosplenic candidiasis) occurs almost exclusively in patients with hematological malignancies who have just recovered from an episode of postchemotherapy neutropenia.RationaleChronic disseminated candidiasis (CDC) is a special clinical presentation of IC observed almost exclusively in oncohematological patients who are recovering from neutropenia due to a postchemotherapy aplasia. CDC occurs in 7% of the patients with acute leukemia who receive chemotherapy; however, its incidence has decreased in recent years, possibly in relation to the antifungal prophylaxis (preferably with azoles) and empirical antifungal treatments (primarily with candins or amphotericin B) administered to these patients.14,38
All the experts consulted agreed that chronic disseminated candidiasis occurs almost exclusively in patients with hematological malignancies after recovering from a postchemotherapy neutropenia episode. Specifically, and using a 0–9 point scale, the 29 specialists granted 7 or more points to this statement. The average score was 8.19 points, and the degree of consensus achieved was high (100%).
3b. When CDC is suspected, imaging techniques (ultrasound scanning, contrast-enhanced computed tomography, or magnetic resonance imaging) must be performed to confirm the entity, and if there is no contraindication, to guide a puncture aspiration and/or a biopsy to obtain samples for microbiological cultures and pathological studies.RationaleThe diagnosis of CDC is a real challenge, especially when candidemia is not known or documented. Therefore, in the neutropenia recovery period, complementary studies must be performed using direct ophthalmoscopy (to observe possible fungal septic metastasis in the retina) and using imaging techniques that can evidence abscesses or microabscesses in the solid intra-abdominal viscera primarily affected, such as the liver and spleen. Imaging techniques have also been useful in monitoring the response to antifungal treatment because they can show the stability or reduction of the size and/or the number of lesions and whether there is recurrence after antifungal treatment interruption.14,38
All the panel members agreed that when CDC is suspected, abdominal ultrasound scanning, contrast-enhanced computed tomography, or magnetic resonance imaging must be performed to confirm the diagnosis and, if there is no contraindication, to guide a puncture aspiration and/or a biopsy to obtain samples for microbiological cultures and pathological studies. Specifically, and using a scale of 0–9 points, in which 9 represents the greatest level of importance, the 29 experts granted 7 or more points to this statement. The average score was established at 8.27 points, and the consensus level was high (Top 2>90%).
3c. In the treatment of CDC, in addition to antifungal drugs, corticosteroids might be necessary to control the inflammatory component of the associated immune reconstitution syndrome.RationaleCDC is currently considered an inflammatory immune reconstitution syndrome due to the two-way relationship established between fungus and host, which is common during neutropenia recovery (“reconstitution of polymorphonuclear leucocytes”); consequently, some authors and guidelines recommend the addition of corticosteroids to the antifungal treatment.31,63 However, no comparative studies, with or without adjuvant corticotherapy, have been published in regard to an improvement in morbidity or a survival advantage in this entity.
In the treatment of CDC, approximately 79.3% of the experts consulted considered the addition of corticosteroids to the antifungal drugs necessary to control the inflammatory component of associated immune reconstitution syndrome. Specifically, and using a 0–9 point scale, 23 experts granted 7 or more points to this recommendation. The average score was 7.2 points, with a high degree of consensus (>80%).
4. Proper management of fungal peritonitis in patients on peritoneal dialysis requires the removal of the peritoneal catheter.RationaleThe peritoneal catheter is a foreign body that facilitates the emergence of infections and serves as a reservoir for bacteria and fungi. Infection can occur at the exit site, in the subcutaneous route, or in the peritoneum (peritonitis). Peritonitis continues to be a complication of peritoneal dialysis, contributing to the failure of the technique, hospitalization, and even death. Fungal peritonitis is primarily produced by species of the genus Candida, particularly by C. albicans, although in recent years other species of the genus has become more prevalent than C. albicans. Compared with other microorganisms, fungal peritonitis has been associated with higher hospitalization rates, withdrawal of the catheter, hemodialysis transfer, and death. In all patients on peritoneal dialysis with peritonitis caused by Candida or other fungi, the dialysis catheter must be removed promptly, and appropriate antifungal therapy must be administered for at least 14 days.6,35
The panel experts reached full consensus regarding removal of the peritoneal catheter as key to fungal peritonitis treatment in patients on peritoneal dialysis. Based on a scale of 0–9 points, in which 9 represents the greatest level of importance, 100% of the specialists awarded 8 or more points to this statement. The average score was established at 8.83 points, and the consensus level was high (Top 1>80%).
5. In candidiasis of the biliary tract causing obstruction, antifungal treatment must be complemented with bile drainage, preferably by an endoscopic procedure.RationaleFungal infection of the biliary tract is observed in patients with prior antibiotic therapy, cancer, pancreatitis, in those who are immunosuppressed, in patients who undergo biliary surgery, reiterated instrumental manipulation, or solid organ transplant (SOT). C. albicans is the species more frequently isolated in fungal biliary tract infections, although other species of the genus have emerged in recent years. Fungal infections are a common cause of bile duct obstruction; therefore, treatment of candidiasis of the biliary tract must include draining, washing, and/or debridement of biliary tree, usually by endoscopic retrograde cholangiopancreatography (ERCP). In cases of ERCP failure, endoscopic ultrasound-guided biliary drainage is an innovative alternative to classical surgical drainage or percutaneous cholecystostomy.16,26
All the specialists consulted agreed that in biliary tract candidiasis causing obstruction, antifungal treatment must be complemented with bile drainage (preferably by endoscopic procedure). The degree of consensus achieved was high (Top 2>85%), and the average score was 8.1 points.
6a. Universal antifungal prophylaxis is not recommended in liver transplant (LT) recipients, and must be selected for those patients with certain risk factors for fungal infection.RationaleUnlike lung transplant, antifungal prophylaxis in other SOT recipients remains controversial and constitutes a real challenge. Strategies to prevent candidemia in SOT recipients in general, and intra-abdominal candidiasis in LT recipients in particular, should be based on epidemiological local trends and, when appropriate, should be limited to patients at high risk. Specific risk factors for IC in LT have been described: perioperative transfusion of >10 red blood cell units; ICU stay>5 days post-transplantation; preoperative blood creatinine>2mg/dl or need for dialysis; biliary-digestive anastomosis; hepatic artery thrombosis; retransplant; pretransplant fulminant liver failure; need for an immediate post-transplant reoperation; serious graft rejection; Candida colonization in the first 3 days post-transplant; and CMV infection.22,25,58
All the panel members agreed that universal antifungal prophylaxis is not recommended in LT recipients, but must be considered for those patients with risk factors for fungal infection. Based on a scale of 0–9 points, in which 9 represents the greatest level of importance, 100% of the specialists awarded 7 or more points to this statement. The average score was established at 8.42 points, and the consensus level was high (Top 2>90%).
6b. Empiric antifungal therapy with echinocandins should be prescribed in liver transplant recipients with risk factors for IC – especially in hemodynamically unstable patients, in those previously exposed to an azole, and in those at high risk of infection by azole-resistant Candida species (C. glabrata or C. krusei).RationaleSOT recipients have a substantial risk of IC, especially intra-abdominal SOT (liver, pancreas, or intestine) recipients. Candida infection therapy in patients with SOT does not differ from the recommended treatment guidelines for other patients, especially those with pathology or abdominal surgery, although there are some specific limitations to the use of certain antifungals in SOT recipients. Deoxycholate amphotericin B should not be used due to its nephrotoxicity, especially in patients receiving anticalcineurin agents as immunosuppressive treatment; all azoles interact with anticalcineurin drugs due to their cytochrome P450 metabolism, for which monitoring of the plasma concentration of both the immunosuppressive and azole agents is important. Nevertheless, echinocandins (caspofungin, anidulafungin, and micafungin) have typically few adverse effects and fewer drug interactions in SOT recipients; consequently, they are the antifungals of choice to start an empiric antifungal therapy in LT recipients with high suspicion of invasive candidiasis.43,53,65
All the specialists agreed that empiric antifungal therapy with echinocandins should be prescribed in LT recipients with risk factors for IC – especially in hemodynamically unstable patients, those previously exposed to an azole, or at high risk of infection by C. glabrata or C. krusei. Specifically, and based on a scale of 0–9, in which 9 represents the highest level, the average score obtained for this statement was 8.38 points. A high level of consensus was achieved (Top 2>90%).
6c. Due to the significant drug interactions between azoles and immunosuppressive drugs, such as anticalcineurins, the use of these antifungals is not recommended in LT recipients with IC; when there is no alternative, monitoring immunosuppressant plasma levels is requiredRationaleAzoles and amphotericin B formulations exhibit adverse effects that can be critical in the LT recipient. The use of triazole agents is frequently limited by their interactions with immunosuppressive calcineurin inhibitors (such as cyclosporine, sirolimus, or tacrolimus) and by the associated adverse effects, especially if graft dysfunction or impaired renal function is present. In most cases, IC occurs in the immediate post-transplant period in an ICU-admitted patient, who sometimes has renal failure or is being treated with hemodialysis. In this situation, selecting the correct dosage of anticalcineurins is difficult. The safety profile of candins is better than other antifungals for SOT recipients due to the absence of nephrotoxicity in their minor interactions on the cytochrome P450. Consequently, the three echinocandins are useful in the clinical management of IC in LT recipients, although small differences among them in metabolism and elimination have been observed.43,53,65
All the panel members agreed that the use of azoles is not recommended in LT recipients with IC; if there is no alternative, monitoring immunosuppressant plasma levels would be required. Specifically, and using a scale of 0–9 points, in which 9 represents the greatest level of importance, the 29 experts granted 7 or more points to this statement. The average score was established at 8.06 points, and the consensus level was high (Top 2>76%).
7a. In patients with IC and moderate liver dysfunction (Child–Pugh 7–9), echinocandins are recommended, and the use of azoles should be avoidedRationaleThe liver metabolizes caspofungin and micafungin, therefore altering plasma concentrations, although in a different manner in the case of hepatic dysfunction. Anidulafungin, due to its extrahepatic metabolism, does not require dose adjustment in any degree of hepatic insufficiency. In mild hepatic impairment (Child–Pugh<7), no dose adjustment of echinocandins is required. In moderate hepatic impairment (Child–Pugh 7–9), the levels of caspofungin are typically increased, whereas those of micafungin are reduced, and those of anidulafungin are not altered. In severe hepatic dysfunction (Child–Pugh>9), micafungin and caspofungin are not recommended because sufficient pharmacokinetic data do not exist. In this case, anidulafungin should be prescribed. Regarding the azoles, there is risk of hepatotoxicity and they might also require dose adjustment in moderate liver insufficiency.17,28
Full consensus of the specialists regarding the administration of echinocandins and avoiding the use of azoles in the treatment of IC in patients with moderate liver dysfunction (Child–Pugh 7–9) was reached. All the specialists awarded 7 or more points to the statement. The average score was established at 7.89 points, and the consensus level was high (Top 2>65%).
7b. Echinocandins are the antifungals of choice in patients with any degree of renal dysfunctionRationaleFluconazole is cleared by renal excretion, for which the dose must be adjusted to half when creatinine clearance drops below 60ml/min. Voriconazole does not require dosage adjustment, although an intravenous formulation should not be used with creatinine clearance below 30ml/min due to the accumulation and possible toxicity of the excipient (cyclodextrin); nevertheless, its use in patients with renal failure has been described in the literature. Posaconazole is subject to minimal urinary excretion; therefore, the standard dose of orally administered posaconazole for antifungal prophylaxis can be used in patients with varying degrees of renal impairment. Due to the low renal excretion of anidulafungin, caspofungin, and micafungin, no dosage adjustment is required in patients with renal dysfunction.12,44
The vast majority of the experts consulted (89.6%) considered echinocandins the antifungal of choice in patients with any degree of renal dysfunction. Specifically, and based on a scale of 0–9 points, in which 9 represents the greatest level of importance, 26 of the 29 specialists granted 7 or more points to this statement, establishing an average of 7.79 points.
7c. All the echinocandins can be considered similar in the treatment of patients needing renal replacement therapy (continuous or intermittent), and no dose adjustments are neededRationaleFluconazole is dialyzable, for which the postdialysis dosage must be adjusted; however, in the case of continuous venovenous hemofiltration, significant increases in dose are needed. Classically, drugs such as echinocandins, with high protein attachment and mostly non-renal elimination, were not cleared by renal replacement therapy, indicating that no dose adjustment is needed. However, adsorption of echinocandins to hemofilter membranes has been demonstrated (up to 20% in the case of anidulafungin), although they do not affect the minimum plasma levels required. Based on recently published pharmacokinetic data on patients undergoing continuous renal replacement therapy, echinocandins can be administered at usual doses. However, in the case of micafungin, if a C. parapsilosis infection is suspected, administration of a loading dose might be necessary to achieve therapeutic levels.2,20,36
All the experts consulted considered the three echinocandins comparable in the treatment of patients needing renal replacement therapy without a dose adjustment requirement. Specifically, the 29 specialists granted 7 or more points to this statement, establishing an average of 8.12 points, with a high level of consensus (Top 2>85%).
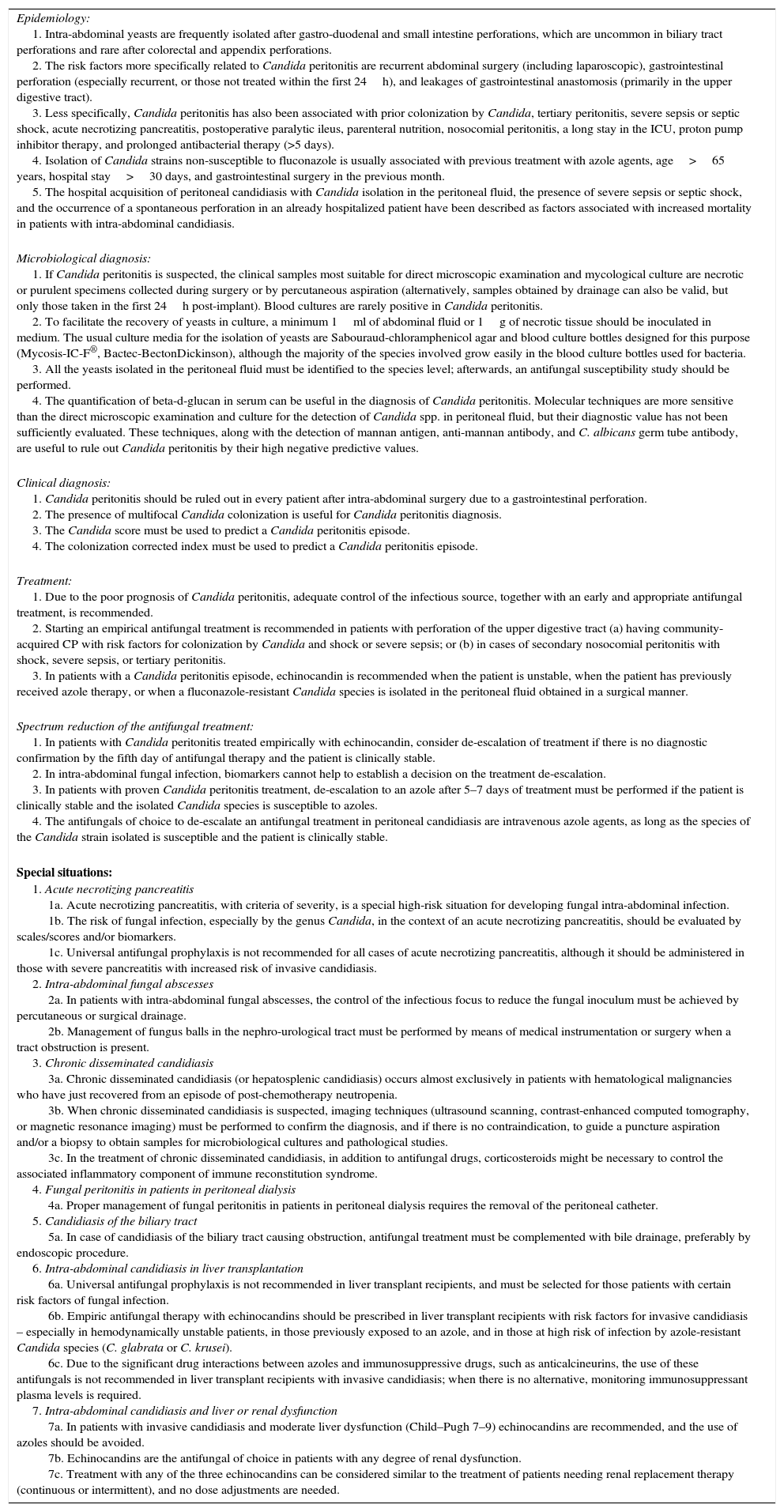
The final recommendations are summarized in Table 1.
Recommendations approved by the panel of experts.
| Epidemiology: 1. Intra-abdominal yeasts are frequently isolated after gastro-duodenal and small intestine perforations, which are uncommon in biliary tract perforations and rare after colorectal and appendix perforations. 2. The risk factors more specifically related to Candida peritonitis are recurrent abdominal surgery (including laparoscopic), gastrointestinal perforation (especially recurrent, or those not treated within the first 24h), and leakages of gastrointestinal anastomosis (primarily in the upper digestive tract). 3. Less specifically, Candida peritonitis has also been associated with prior colonization by Candida, tertiary peritonitis, severe sepsis or septic shock, acute necrotizing pancreatitis, postoperative paralytic ileus, parenteral nutrition, nosocomial peritonitis, a long stay in the ICU, proton pump inhibitor therapy, and prolonged antibacterial therapy (>5 days). 4. Isolation of Candida strains non-susceptible to fluconazole is usually associated with previous treatment with azole agents, age>65 years, hospital stay>30 days, and gastrointestinal surgery in the previous month. 5. The hospital acquisition of peritoneal candidiasis with Candida isolation in the peritoneal fluid, the presence of severe sepsis or septic shock, and the occurrence of a spontaneous perforation in an already hospitalized patient have been described as factors associated with increased mortality in patients with intra-abdominal candidiasis. |
| Microbiological diagnosis: 1. If Candida peritonitis is suspected, the clinical samples most suitable for direct microscopic examination and mycological culture are necrotic or purulent specimens collected during surgery or by percutaneous aspiration (alternatively, samples obtained by drainage can also be valid, but only those taken in the first 24h post-implant). Blood cultures are rarely positive in Candida peritonitis. 2. To facilitate the recovery of yeasts in culture, a minimum 1ml of abdominal fluid or 1g of necrotic tissue should be inoculated in medium. The usual culture media for the isolation of yeasts are Sabouraud-chloramphenicol agar and blood culture bottles designed for this purpose (Mycosis-IC-F®, Bactec-BectonDickinson), although the majority of the species involved grow easily in the blood culture bottles used for bacteria. 3. All the yeasts isolated in the peritoneal fluid must be identified to the species level; afterwards, an antifungal susceptibility study should be performed. 4. The quantification of beta-d-glucan in serum can be useful in the diagnosis of Candida peritonitis. Molecular techniques are more sensitive than the direct microscopic examination and culture for the detection of Candida spp. in peritoneal fluid, but their diagnostic value has not been sufficiently evaluated. These techniques, along with the detection of mannan antigen, anti-mannan antibody, and C. albicans germ tube antibody, are useful to rule out Candida peritonitis by their high negative predictive values. |
| Clinical diagnosis: 1. Candida peritonitis should be ruled out in every patient after intra-abdominal surgery due to a gastrointestinal perforation. 2. The presence of multifocal Candida colonization is useful for Candida peritonitis diagnosis. 3. The Candida score must be used to predict a Candida peritonitis episode. 4. The colonization corrected index must be used to predict a Candida peritonitis episode. |
| Treatment: 1. Due to the poor prognosis of Candida peritonitis, adequate control of the infectious source, together with an early and appropriate antifungal treatment, is recommended. 2. Starting an empirical antifungal treatment is recommended in patients with perforation of the upper digestive tract (a) having community-acquired CP with risk factors for colonization by Candida and shock or severe sepsis; or (b) in cases of secondary nosocomial peritonitis with shock, severe sepsis, or tertiary peritonitis. 3. In patients with a Candida peritonitis episode, echinocandin is recommended when the patient is unstable, when the patient has previously received azole therapy, or when a fluconazole-resistant Candida species is isolated in the peritoneal fluid obtained in a surgical manner. |
| Spectrum reduction of the antifungal treatment: 1. In patients with Candida peritonitis treated empirically with echinocandin, consider de-escalation of treatment if there is no diagnostic confirmation by the fifth day of antifungal therapy and the patient is clinically stable. 2. In intra-abdominal fungal infection, biomarkers cannot help to establish a decision on the treatment de-escalation. 3. In patients with proven Candida peritonitis treatment, de-escalation to an azole after 5–7 days of treatment must be performed if the patient is clinically stable and the isolated Candida species is susceptible to azoles. 4. The antifungals of choice to de-escalate an antifungal treatment in peritoneal candidiasis are intravenous azole agents, as long as the species of the Candida strain isolated is susceptible and the patient is clinically stable. |
| Special situations: 1. Acute necrotizing pancreatitis 1a. Acute necrotizing pancreatitis, with criteria of severity, is a special high-risk situation for developing fungal intra-abdominal infection. 1b. The risk of fungal infection, especially by the genus Candida, in the context of an acute necrotizing pancreatitis, should be evaluated by scales/scores and/or biomarkers. 1c. Universal antifungal prophylaxis is not recommended for all cases of acute necrotizing pancreatitis, although it should be administered in those with severe pancreatitis with increased risk of invasive candidiasis. 2. Intra-abdominal fungal abscesses 2a. In patients with intra-abdominal fungal abscesses, the control of the infectious focus to reduce the fungal inoculum must be achieved by percutaneous or surgical drainage. 2b. Management of fungus balls in the nephro-urological tract must be performed by means of medical instrumentation or surgery when a tract obstruction is present. 3. Chronic disseminated candidiasis 3a. Chronic disseminated candidiasis (or hepatosplenic candidiasis) occurs almost exclusively in patients with hematological malignancies who have just recovered from an episode of post-chemotherapy neutropenia. 3b. When chronic disseminated candidiasis is suspected, imaging techniques (ultrasound scanning, contrast-enhanced computed tomography, or magnetic resonance imaging) must be performed to confirm the diagnosis, and if there is no contraindication, to guide a puncture aspiration and/or a biopsy to obtain samples for microbiological cultures and pathological studies. 3c. In the treatment of chronic disseminated candidiasis, in addition to antifungal drugs, corticosteroids might be necessary to control the associated inflammatory component of immune reconstitution syndrome. 4. Fungal peritonitis in patients in peritoneal dialysis 4a. Proper management of fungal peritonitis in patients in peritoneal dialysis requires the removal of the peritoneal catheter. 5. Candidiasis of the biliary tract 5a. In case of candidiasis of the biliary tract causing obstruction, antifungal treatment must be complemented with bile drainage, preferably by endoscopic procedure. 6. Intra-abdominal candidiasis in liver transplantation 6a. Universal antifungal prophylaxis is not recommended in liver transplant recipients, and must be selected for those patients with certain risk factors of fungal infection. 6b. Empiric antifungal therapy with echinocandins should be prescribed in liver transplant recipients with risk factors for invasive candidiasis – especially in hemodynamically unstable patients, in those previously exposed to an azole, and in those at high risk of infection by azole-resistant Candida species (C. glabrata or C. krusei). 6c. Due to the significant drug interactions between azoles and immunosuppressive drugs, such as anticalcineurins, the use of these antifungals is not recommended in liver transplant recipients with invasive candidiasis; when there is no alternative, monitoring immunosuppressant plasma levels is required. 7. Intra-abdominal candidiasis and liver or renal dysfunction 7a. In patients with invasive candidiasis and moderate liver dysfunction (Child–Pugh 7–9) echinocandins are recommended, and the use of azoles should be avoided. 7b. Echinocandins are the antifungal of choice in patients with any degree of renal dysfunction. 7c. Treatment with any of the three echinocandins can be considered similar to the treatment of patients needing renal replacement therapy (continuous or intermittent), and no dose adjustments are needed. |
None to declare.
Vicente Abril
Consorcio Hospital General Universitario, Valencia
Manuel Alós
Hospital Clínico Universitario, Valencia
José Luis Antón Pascual
Hospital Universitario San Juan, Alicante
Rocío Armero
Hospital Universitario Dr. Peset, Valencia
Miguel Angel Arribas
Hospital Arnau de Vilanova, Valencia
Juan José Camarena
Hospital Universitario Dr. Peset, Valencia
José Antonio Carbonell
Hospital Clínico Universitario, Valencia
Edurne Carbonell
Hospital Clínico Universitario, Valencia
Andrés Carrillo Alcaraz
Hospital Universitario Morales Meseguer, Murcia
Mónica Climente
Hospital Universitario Dr. Peset, Valencia
Raquel Durá
Consorcio Hospital General Universitario, Valencia
Carlos García-Palenciano
Hospital Virgen de la Arrixaca, Murcia
Concepción Gimeno
Consorcio Hospital General Universitario, Valencia
Ricardo Gimeno
Hospital Universitario y Politécnico La Fe, Valencia
Bárbara Gomila
Hospital General, Castellón
Javier Guasch Pomés
Hospital de la Plana, Villareal
Esperanza Merino de Lucas
Hospital General Universitario, Alicante
Ignacio Moreno
Hospital Universitario y Politécnico La Fe, Valencia
Rosa Oltra
Hospital Clínico Universitario, Valencia
Pilar Ortega
Consorcio Hospital General Universitario, Valencia
Juan Carlos Pardo Talavera
Hospital Reina Sofía, Murcia
Ana Pérez Carbonell
Hospital Universitario, Elche
Francesc Puchades
Hospital Padre Jofre, Valencia
Roberto Reig
Hospital General, Castellón
María Teresa Rodríguez
Hospital General, Castellón
Eva Romá
Hospital Universitario y Politécnico La Fe, Valencia
Silverio Salvador
Hospital General Universitario, Alicante
Ricardo Serrano
Hospital General Universitario, Alicante
Inmaculada Vidal
Hospital General Universitario, Alicante
Gerardo Aguilar (G.A.)
Hospital Clínico Universitario, Valencia
David Navarro (D.N.)
Hospital Clínico Universitario, Valencia
Javier Pemán (J.P.)
Hospital Universitario y Politécnico La Fe, Valencia
Miguel Salavert (M.S.)
Hospital Universitario y Politécnico La Fe, Valencia
Juan Carlos Valía (J.C.V.)
Consorcio Hospital General Universitario, Valencia
Rafael Zaragoza (R.Z.)
Hospital Universitario Dr. Peset, Valencia