Metabolic syndrome (MetS) is a combination of various cardiovascular risk factors with a major impact on morbidity and premature mortality. However, the impact of MetS on self-reported health-related quality of life (HRQoL) is unknown.
This study evaluated the HRQoL in a Spanish adult population aged 55 years and older with MetS.
MethodA cross-sectional analysis was performed with baseline data from the PREDIMED-Plus multicentre randomized trial. The participants were 6430 men and women aged 55–75 years with overweight/obesity (body mass index ≥27 and ≤40kg/m2) and MetS. The SF-36 questionnaire was used as a tool to measure HRQoL. Scores were calculated on each scale of the SF-36 by gender and age.
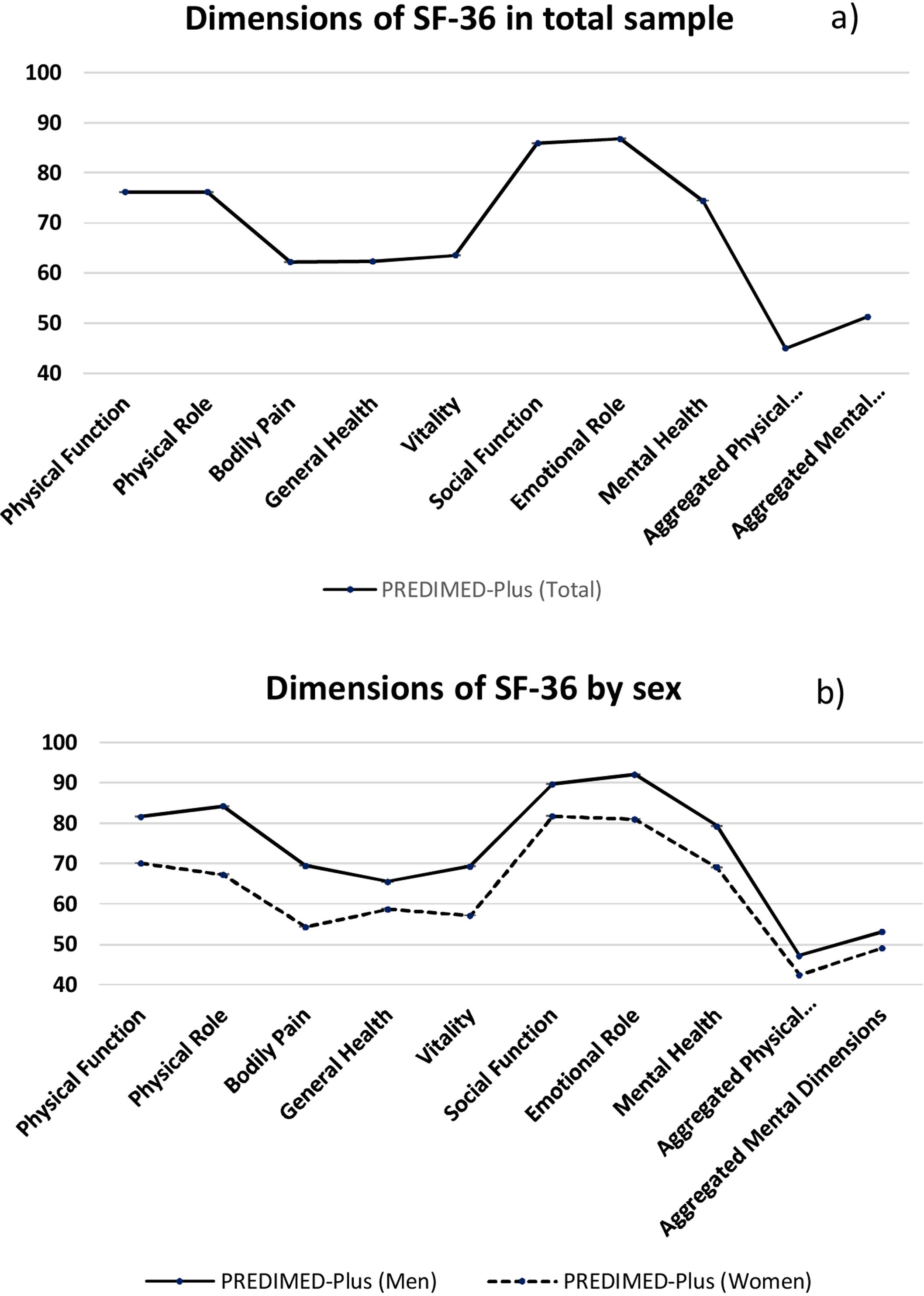
ResultsParticipants showed higher scores in the social function (mean 85.9, 95% CI; 85.4–86.4) and emotional role scales (mean 86.8, 95% CI; 86.0–87.5). By contrast, the worst scores were obtained in the aggregated physical dimensions. In addition, men obtained higher scores than women on all scales. Among men, the worst score was obtained in general health (mean 65.6, 95% CI; 65.0–66.2), and among women, in body pain (mean 54.3, 95%CI; 53.4–55.2). A significant decrease was found in the aggregated physical dimensions score among participants 70–75 years old, but an increased one in the aggregated mental dimensions, compared to younger participants.
ConclusionsOur results reflect that the MetS may negatively affect HRQoL in the aggregated physical dimensions, body pain in women, and general health in men. However, this adverse association was absent for the psychological dimensions of HRQoL, which were less affected.
El síndrome metabólico (SM) es la combinación de diversos factores de riesgo cardiovascular que pueden derivar en un mayor impacto en la morbimortalidad prematura. Sin embargo, el impacto del SM en la calidad de vida relacionada con la salud (CVRS) es desconocido. El objetivo de este estudio es evaluar la CVRS en la población adulta española de 55 años o más con SM.
MétodosSe realizó un análisis transversal con los datos del ensayo PREDIMED-Plus. Seis mil cuatrocientos treinta varones y mujeres entre 55-75 años con sobrepeso/obesidad y SM. El instrumento de medida de la CVRS fue el cuestionario SF-36. Cada escala del SF-36 fue descrita y estratificada por sexo.
ResultadosLos participantes mostraron valores más altos en las escalas función social (media: 85,9; IC 95%: 85,4-86,4) y rol emocional (media: 86,8; IC 95%: 86,0-87,5). En los varones, la peor puntuación fue en la dimensión salud general (media: 65,6; IC 95%: 65,0-66,2) y en las mujeres el dolor corporal (media: 54,3; IC 95%: 53,4-55,2). Además, los varones obtuvieron puntuaciones más altas en todas las escalas. En la escala función física en varones se encontró una disminución significativa de la CVRS en los participantes entre 70 y 75 años en comparación con los más jóvenes. Las peores puntuaciones se obtuvieron en las dimensiones físicas agregadas.
ConclusionesEl SM afecta de manera negativa a la CVRS en las dimensiones agregadas físicas, haciendo especial hincapié en la esfera dolor corporal en mujeres y salud general en varones. Sin embargo, las esferas psicológicas se encuentran menos afectadas por el SM.
Metabolic syndrome (MetS) is a cluster of various cardiovascular risk factors such as abdominal obesity, high blood pressure, insulin resistance, and impaired serum lipid profiles that, when combined, can lead to cardiovascular disease (CVD)1 and increase the risk of mortality.2
The prevalence of MetS in the adult population, using standardized measurements in a representative sample of the Spanish population3 was 22.7% (26.0% women vs. 19.4% men). This prevalence increases with age and is higher in women aged 65 years or older.
It is important to highlight that MetS may lead to alterations in self-perceived well-being, which, for many people, may be more important than the comorbidities associated with MetS.4 MetS and an increased body-mass index (BMI)>27kg/m2, have been linked to a decrease in health-related quality of life (HRQoL).5,6
In turn, weight loss and an increase in physical activity may enhance HRQoL.6
Self-perceived HRQoL is relevant because it could be a strong predictor of chronic disease and long-term mortality.7,8 One of the most widely used tools to measure the HRQoL is the short-form SF-36 questionnaire, which has been used by over 400 articles up to date.9 It has been shown to be useful for the general population, specific subgroups, and in studies comparing the burden of different illness.10 In the content review, metric properties and development of the Spanish version of SF-36 done by Vilagut et al.,11 the authors concluded that the SF-36 questionnaire is a particularly well-suited tool to use in investigations and clinical practice with high validity and reproducibility. The primary aim of our study was to assess the HRQoL for the adult Spanish population aged 60 years or older with MetS. This result is of great interest, since it would allow us to assess if being overweight/obese and having MetS may be associated to a poorer quality of life. Moreover, it would permit the design of global strategies in nursing care in order to be able to increase the quality of life in this vulnerable population.
MethodsStudy design and participantsWe carried out a cross-sectional evaluation of baseline data within the framework of the PREDIMED-Plus trial, which design has been extensively described elsewhere12,13 and which study protocol can be found on the PREDIMED-Plus website (https://www.predimedplus.com/).14 Briefly, PREDIMED-Plus study is an ongoing, 6-year, multi-center, parallel group, randomized clinical trial conducted in 23 Spanish recruitment centers to assess the effectiveness of an intensive weight-loss intervention program based on an intensive weight-loss intervention program (based on an energy restricted Mediterranean diet, physical activity promotion and behavioral support) on severe cardiovascular events in comparison with a control group receiving normal care.
The trial was approved by the Institutional Review Board of all recruitment centers where the study was conducted.12 The trial was registered in 2014 at the International Standard Randomized Controlled Trial (ISRCTN89898870).
Eligible participants were community-dwelling men (aged 55–75 years) and women (aged 60–75 years) with overweight or obesity (BMI ≥27kg/m2 and<40kg/m2), meeting at least 3 criteria of the MetS definition,15 and CVD free. Detailed inclusion and exclusion criteria have been extensively described elsewhere12,13 and are available at http://predimedplus.com/.14 We recruited 6874 participants from October 2013 to December 2016 who were randomly assigned in a 1:1 ratio to the intensive diet and lifestyle intervention group or to the usual care group. All participants provided written informed consent.
For the current analysis, we excluded 338 participants who did not complete half of the items that make up the scale and 106 participants with missing information on the baseline HRQoL questionnaire (SF-36-items). From the remaining 6430 participants, 5078 had completed the 36-items at baseline and 1352 participants answered more than half of the items that make up the scale. To preserve the sample size, the imputation of the mean was used to replace missing data. A total of 6430 participants were included for evaluation in the current study. The data were analyzed using the available, complete PREDIMED-Plus database, dated 10/08/2017.
Health-related quality of life assessmentHRQoL was measured using a Spanish version of SF-36, the questionnaire that was validated for the Spanish population, and is widely used as a precise way to measure self-perceived HRQoL.11,16
SF-36 has 36 items that assess eight dimensions or scales: physical functioning, physical role functioning, bodily pain, general health, vitality, social role functioning, emotional role functioning, and mental health. These dimensions are grouped into two components: the physical component of health (physical functioning, physical role functioning, bodily pain and general health) and the mental component or psychosocial aspects (vitality, social role functioning, emotional role functioning, and mental health). The reliability of the scale, measured with Cronbach's α from the SF-36 questionnaire, used to determine the values of the Spanish population of ≥ 60 years was higher than the proposed standard of 0.7.17
Each item was scored with a numeric value, then all values corresponding to the same domain were added up and adjusted to a scale from 0 to 100. A higher punctuation means better health. The HQRoL was completed during the baseline visit.
Other covariatesSocio-demographic variables such as sex, age, birthplace, level of education, and current job were collected using a general questionnaire at baseline.
Statistical analysisMeasures of central tendency and spread were calculated with their 95% confidence intervals for the scores in each of the dimensions of the SF-36. The distribution of participants by sociodemographic characteristics was presented with proportions. We used the stratified values for quinquennials of age (men: 55–59, 60–64, 65–69 and 70–74 years; women: 60–64, 65–69 and 70–74 years) and sex. All analyses were performed with the statistical package StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP.
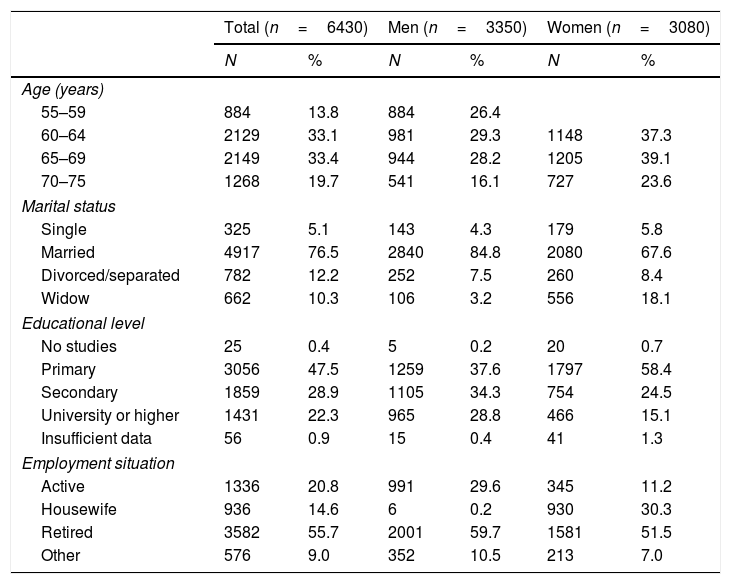
ResultsTable 1 shows the descriptive characteristics of the sample at baseline. A total of 6430 participants, 52.1% of whom were men and 47.9% women, were included. The average age was 64.9 (4.9) years. Most of them were married (76.5%) and had only elementary studies (47.5%). The proportion of participants who were retired was 55.7%.
Descriptive characteristics at baseline of the studied sample.
| Total (n=6430) | Men (n=3350) | Women (n=3080) | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Age (years) | ||||||
| 55–59 | 884 | 13.8 | 884 | 26.4 | ||
| 60–64 | 2129 | 33.1 | 981 | 29.3 | 1148 | 37.3 |
| 65–69 | 2149 | 33.4 | 944 | 28.2 | 1205 | 39.1 |
| 70–75 | 1268 | 19.7 | 541 | 16.1 | 727 | 23.6 |
| Marital status | ||||||
| Single | 325 | 5.1 | 143 | 4.3 | 179 | 5.8 |
| Married | 4917 | 76.5 | 2840 | 84.8 | 2080 | 67.6 |
| Divorced/separated | 782 | 12.2 | 252 | 7.5 | 260 | 8.4 |
| Widow | 662 | 10.3 | 106 | 3.2 | 556 | 18.1 |
| Educational level | ||||||
| No studies | 25 | 0.4 | 5 | 0.2 | 20 | 0.7 |
| Primary | 3056 | 47.5 | 1259 | 37.6 | 1797 | 58.4 |
| Secondary | 1859 | 28.9 | 1105 | 34.3 | 754 | 24.5 |
| University or higher | 1431 | 22.3 | 965 | 28.8 | 466 | 15.1 |
| Insufficient data | 56 | 0.9 | 15 | 0.4 | 41 | 1.3 |
| Employment situation | ||||||
| Active | 1336 | 20.8 | 991 | 29.6 | 345 | 11.2 |
| Housewife | 936 | 14.6 | 6 | 0.2 | 930 | 30.3 |
| Retired | 3582 | 55.7 | 2001 | 59.7 | 1581 | 51.5 |
| Other | 576 | 9.0 | 352 | 10.5 | 213 | 7.0 |
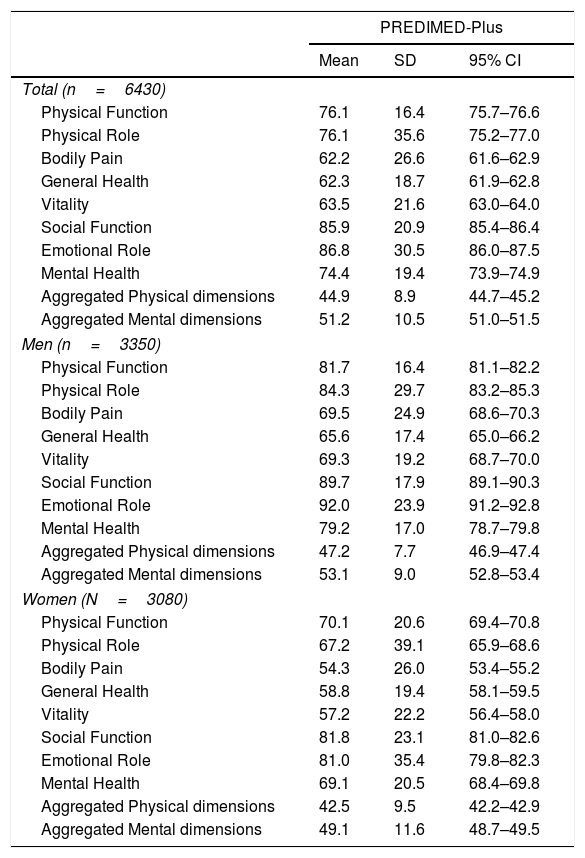
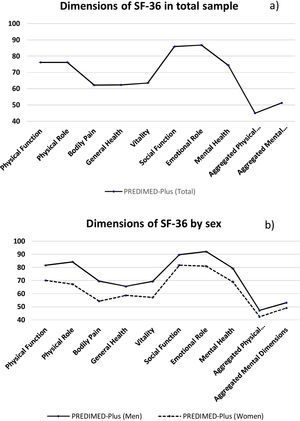
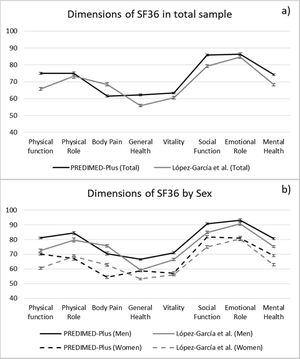
Table 2 shows the SF-36 scale scores, applied both to the general form and stratified by sex in the PREDIMED-Plus study. Participants showed higher values in social function and emotional role scales in total sample and both sexes. In men, the worst score was the dimension of general health and the women was the bodily pain scale. In addition, men obtained higher scores on all scales than women (Fig. 1).
Average scores of the scales evaluated in the SF-36 in the full sample and by sex.
| PREDIMED-Plus | |||
|---|---|---|---|
| Mean | SD | 95% CI | |
| Total (n=6430) | |||
| Physical Function | 76.1 | 16.4 | 75.7–76.6 |
| Physical Role | 76.1 | 35.6 | 75.2–77.0 |
| Bodily Pain | 62.2 | 26.6 | 61.6–62.9 |
| General Health | 62.3 | 18.7 | 61.9–62.8 |
| Vitality | 63.5 | 21.6 | 63.0–64.0 |
| Social Function | 85.9 | 20.9 | 85.4–86.4 |
| Emotional Role | 86.8 | 30.5 | 86.0–87.5 |
| Mental Health | 74.4 | 19.4 | 73.9–74.9 |
| Aggregated Physical dimensions | 44.9 | 8.9 | 44.7–45.2 |
| Aggregated Mental dimensions | 51.2 | 10.5 | 51.0–51.5 |
| Men (n=3350) | |||
| Physical Function | 81.7 | 16.4 | 81.1–82.2 |
| Physical Role | 84.3 | 29.7 | 83.2–85.3 |
| Bodily Pain | 69.5 | 24.9 | 68.6–70.3 |
| General Health | 65.6 | 17.4 | 65.0–66.2 |
| Vitality | 69.3 | 19.2 | 68.7–70.0 |
| Social Function | 89.7 | 17.9 | 89.1–90.3 |
| Emotional Role | 92.0 | 23.9 | 91.2–92.8 |
| Mental Health | 79.2 | 17.0 | 78.7–79.8 |
| Aggregated Physical dimensions | 47.2 | 7.7 | 46.9–47.4 |
| Aggregated Mental dimensions | 53.1 | 9.0 | 52.8–53.4 |
| Women (N=3080) | |||
| Physical Function | 70.1 | 20.6 | 69.4–70.8 |
| Physical Role | 67.2 | 39.1 | 65.9–68.6 |
| Bodily Pain | 54.3 | 26.0 | 53.4–55.2 |
| General Health | 58.8 | 19.4 | 58.1–59.5 |
| Vitality | 57.2 | 22.2 | 56.4–58.0 |
| Social Function | 81.8 | 23.1 | 81.0–82.6 |
| Emotional Role | 81.0 | 35.4 | 79.8–82.3 |
| Mental Health | 69.1 | 20.5 | 68.4–69.8 |
| Aggregated Physical dimensions | 42.5 | 9.5 | 42.2–42.9 |
| Aggregated Mental dimensions | 49.1 | 11.6 | 48.7–49.5 |
CI: Confidence Interval; SD: Standard deviation.
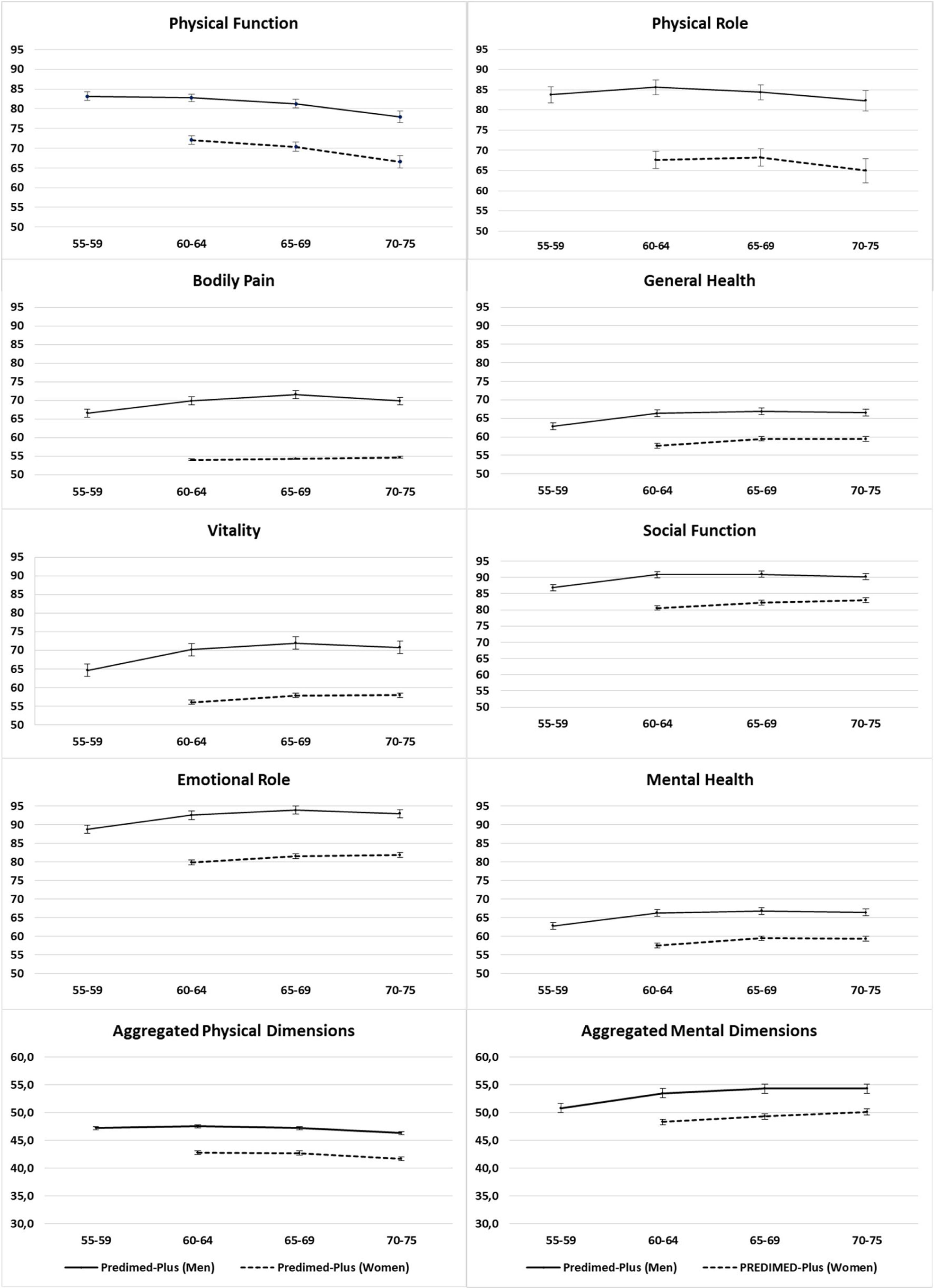
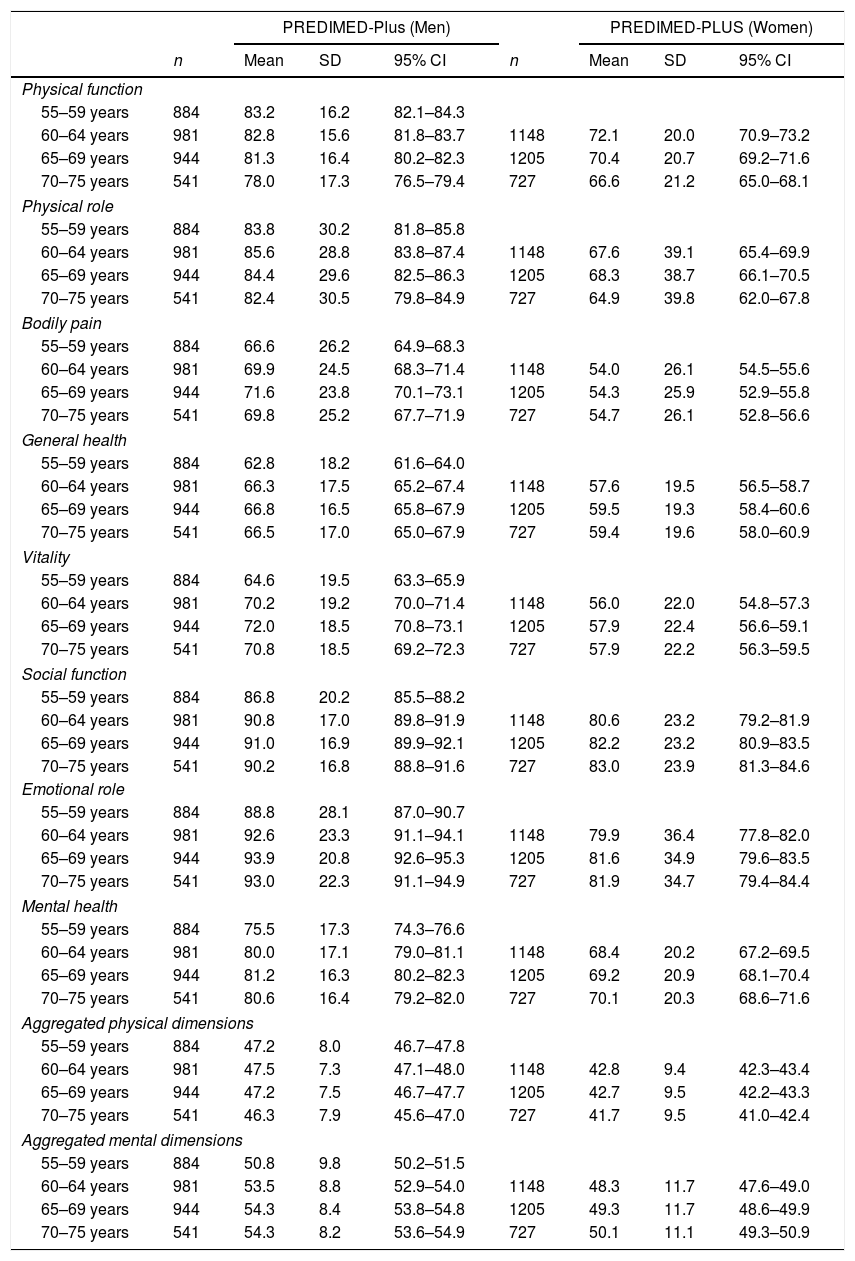
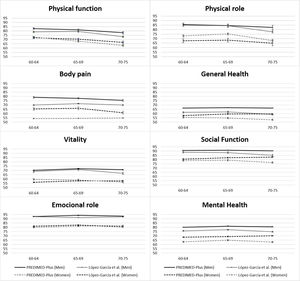
Table 3 shows the scores obtained in SF-36 in men and women stratified for quinquennials of age groups (55–59 years/60–64 years/65–69 years/70–75 years). In men, it can be seen that as age increases, HRQoL decreases significantly on the physical function scale. Participants aged 70–75 have a worse HRQoL than those aged 55–59 to 60–65. There is also a nonsignificant decrease in HRQoL on the physical role scale in older participants. In all other dimensions the score is similar in all three age ranges. In the case of women, we also found significant differences in the scales of physical function and physical role between the different age ranges, with a decrease in HRQoL in people between 70 and 75 years old compared to those between 60 and 65 years old. In the rest of the scales there is a slight increase, without significant differences, in the mean scores as age advances (Fig. 2).
Average scores of SF-36's dimensions in PREDIMED-Plus by sex and age.
| PREDIMED-Plus (Men) | PREDIMED-PLUS (Women) | |||||||
|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | 95% CI | n | Mean | SD | 95% CI | |
| Physical function | ||||||||
| 55–59 years | 884 | 83.2 | 16.2 | 82.1–84.3 | ||||
| 60–64 years | 981 | 82.8 | 15.6 | 81.8–83.7 | 1148 | 72.1 | 20.0 | 70.9–73.2 |
| 65–69 years | 944 | 81.3 | 16.4 | 80.2–82.3 | 1205 | 70.4 | 20.7 | 69.2–71.6 |
| 70–75 years | 541 | 78.0 | 17.3 | 76.5–79.4 | 727 | 66.6 | 21.2 | 65.0–68.1 |
| Physical role | ||||||||
| 55–59 years | 884 | 83.8 | 30.2 | 81.8–85.8 | ||||
| 60–64 years | 981 | 85.6 | 28.8 | 83.8–87.4 | 1148 | 67.6 | 39.1 | 65.4–69.9 |
| 65–69 years | 944 | 84.4 | 29.6 | 82.5–86.3 | 1205 | 68.3 | 38.7 | 66.1–70.5 |
| 70–75 years | 541 | 82.4 | 30.5 | 79.8–84.9 | 727 | 64.9 | 39.8 | 62.0–67.8 |
| Bodily pain | ||||||||
| 55–59 years | 884 | 66.6 | 26.2 | 64.9–68.3 | ||||
| 60–64 years | 981 | 69.9 | 24.5 | 68.3–71.4 | 1148 | 54.0 | 26.1 | 54.5–55.6 |
| 65–69 years | 944 | 71.6 | 23.8 | 70.1–73.1 | 1205 | 54.3 | 25.9 | 52.9–55.8 |
| 70–75 years | 541 | 69.8 | 25.2 | 67.7–71.9 | 727 | 54.7 | 26.1 | 52.8–56.6 |
| General health | ||||||||
| 55–59 years | 884 | 62.8 | 18.2 | 61.6–64.0 | ||||
| 60–64 years | 981 | 66.3 | 17.5 | 65.2–67.4 | 1148 | 57.6 | 19.5 | 56.5–58.7 |
| 65–69 years | 944 | 66.8 | 16.5 | 65.8–67.9 | 1205 | 59.5 | 19.3 | 58.4–60.6 |
| 70–75 years | 541 | 66.5 | 17.0 | 65.0–67.9 | 727 | 59.4 | 19.6 | 58.0–60.9 |
| Vitality | ||||||||
| 55–59 years | 884 | 64.6 | 19.5 | 63.3–65.9 | ||||
| 60–64 years | 981 | 70.2 | 19.2 | 70.0–71.4 | 1148 | 56.0 | 22.0 | 54.8–57.3 |
| 65–69 years | 944 | 72.0 | 18.5 | 70.8–73.1 | 1205 | 57.9 | 22.4 | 56.6–59.1 |
| 70–75 years | 541 | 70.8 | 18.5 | 69.2–72.3 | 727 | 57.9 | 22.2 | 56.3–59.5 |
| Social function | ||||||||
| 55–59 years | 884 | 86.8 | 20.2 | 85.5–88.2 | ||||
| 60–64 years | 981 | 90.8 | 17.0 | 89.8–91.9 | 1148 | 80.6 | 23.2 | 79.2–81.9 |
| 65–69 years | 944 | 91.0 | 16.9 | 89.9–92.1 | 1205 | 82.2 | 23.2 | 80.9–83.5 |
| 70–75 years | 541 | 90.2 | 16.8 | 88.8–91.6 | 727 | 83.0 | 23.9 | 81.3–84.6 |
| Emotional role | ||||||||
| 55–59 years | 884 | 88.8 | 28.1 | 87.0–90.7 | ||||
| 60–64 years | 981 | 92.6 | 23.3 | 91.1–94.1 | 1148 | 79.9 | 36.4 | 77.8–82.0 |
| 65–69 years | 944 | 93.9 | 20.8 | 92.6–95.3 | 1205 | 81.6 | 34.9 | 79.6–83.5 |
| 70–75 years | 541 | 93.0 | 22.3 | 91.1–94.9 | 727 | 81.9 | 34.7 | 79.4–84.4 |
| Mental health | ||||||||
| 55–59 years | 884 | 75.5 | 17.3 | 74.3–76.6 | ||||
| 60–64 years | 981 | 80.0 | 17.1 | 79.0–81.1 | 1148 | 68.4 | 20.2 | 67.2–69.5 |
| 65–69 years | 944 | 81.2 | 16.3 | 80.2–82.3 | 1205 | 69.2 | 20.9 | 68.1–70.4 |
| 70–75 years | 541 | 80.6 | 16.4 | 79.2–82.0 | 727 | 70.1 | 20.3 | 68.6–71.6 |
| Aggregated physical dimensions | ||||||||
| 55–59 years | 884 | 47.2 | 8.0 | 46.7–47.8 | ||||
| 60–64 years | 981 | 47.5 | 7.3 | 47.1–48.0 | 1148 | 42.8 | 9.4 | 42.3–43.4 |
| 65–69 years | 944 | 47.2 | 7.5 | 46.7–47.7 | 1205 | 42.7 | 9.5 | 42.2–43.3 |
| 70–75 years | 541 | 46.3 | 7.9 | 45.6–47.0 | 727 | 41.7 | 9.5 | 41.0–42.4 |
| Aggregated mental dimensions | ||||||||
| 55–59 years | 884 | 50.8 | 9.8 | 50.2–51.5 | ||||
| 60–64 years | 981 | 53.5 | 8.8 | 52.9–54.0 | 1148 | 48.3 | 11.7 | 47.6–49.0 |
| 65–69 years | 944 | 54.3 | 8.4 | 53.8–54.8 | 1205 | 49.3 | 11.7 | 48.6–49.9 |
| 70–75 years | 541 | 54.3 | 8.2 | 53.6–54.9 | 727 | 50.1 | 11.1 | 49.3–50.9 |
CI: Confidence Interval; SD: Standard deviation.
Both in the overall sample and in the sample stratified by age and sex, we can verify that the worst scores were obtained in the aggregated physical dimensions.
DiscussionThe main findings of the present cross-sectional study conducted in individuals with MetS suggest that better average scores were obtained in the emotional role functioning and social functioning scales. The lower values in our study for the areas of bodily pain, general health and vitality, were probably due to the participants’ MetS which may have led to a negative impact on their HRQoL.
In all our sample, the minimum scores documented for men were for general health, bodily pain and vitality scales, while for women the minimum scores were also in the physical role scale, like other studies.5,18–21 This could be due to all participants in our study being overweight/obese and at least three criteria of MetS, as well as an age between 55 and 75 years. Obesity is a problem that has been on the rise as is the normalization of overweight in the elderly,22,23 so its impact on HRQoL can be expected to be more pronounced in the physical dimension and more moderate in the psychosocial dimension. The dimensions of the SF-36 questionnaire that measure the physical burden are the perception of general health, physical functioning, vitality and bodily pain.21 Obesity means an excessive body fat storage, in addition, participants are aged between 55 and 75 years and at this age there is a decrease in muscle mass and abdominal and perivisceral body fat redistribution. This is associated with increased abdominal circumference, which means increased difficulties in mobility, daily activities and bodily pain. There is also decreased functional ability and an increased disability rate, which occurs during aging and are exacerbated by obesity.24,25
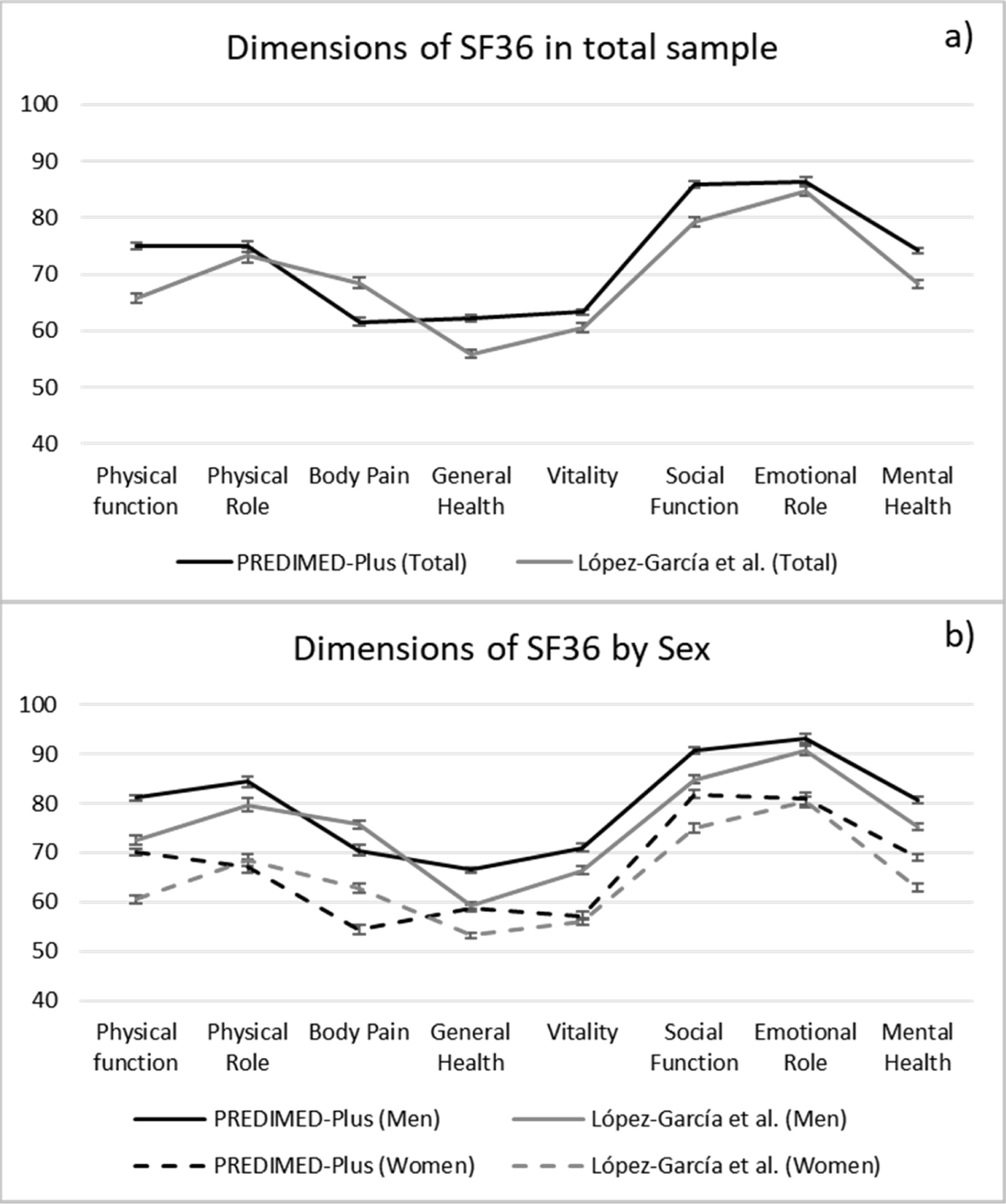
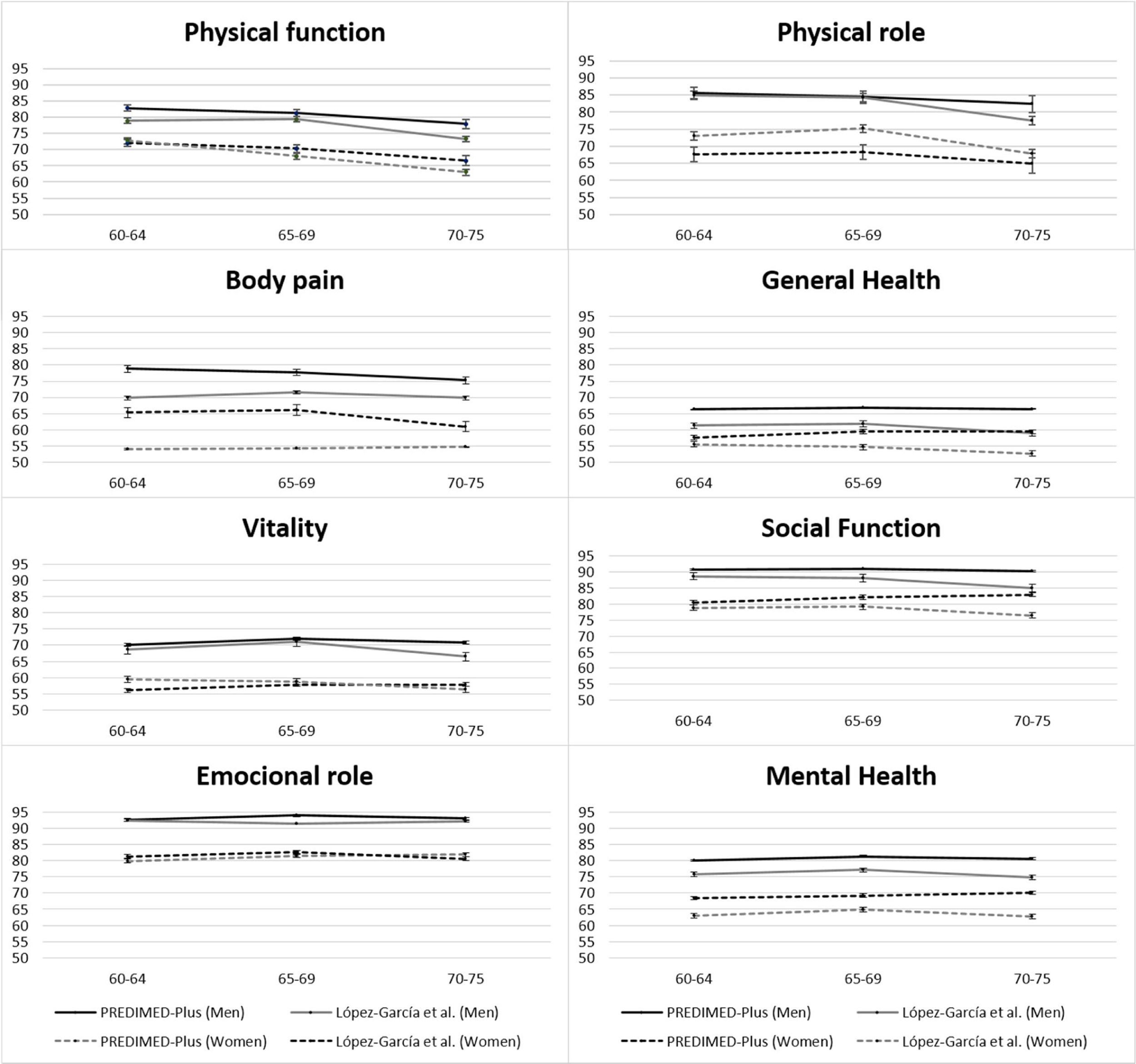
A comparison with the reference values of HRQoL in the Spanish population ≥60 years published by López-García et al.,17 in 2003 (Figs. 1S and 2S, supplementary data) shows that the data follow the same distribution as in our study, the scales with the highest mean scores in both males and females are emotional role and social function, while the lowest scores can be found in the dimensions general health and vitality. In addition, we also found a decrease in HRQoL in the physical dimensions. Similarly, the scores obtained in women are lower than in men. We obtained results similar to previous studies.26–29 However, if we compare each of the scales, we observe that the scores in the PREDIMED-Plus study are higher than the reference values for the Spanish population ≥60 years on all scales except bodily pain. A possible explanation to the observed differences could be explained due to the 15 years that have elapsed between the studies. Because the HRQoL is a reflection of the knowledge, experiences and values of individuals and collectivities, which are conditioned by a particular moment, quality of life criteria have evolved through the years.30 PREDIMED-Plus is a primary cardiovascular prevention trial. Consequently, although participants have MetS, they have not yet had a cardiovascular event and therefore consider themselves healthy people, while the participants in the study by López-García et al.17 were selected from a sample of the general population where participants with and without pathologies and several chronic conditions were also included. Therefore, it is expected that the HRQoL in our study might be higher.31
In the Karlsson et al. study32 the results were the other way around, meaning people with obesity scored lower in their mood compared to healthy reference people. However, in our study an association with better mental health was similar to the Barcones-Molero et al. study.21
There, they checked the obesity and weight gain influence over quality of life, according to SF-36 for the dynamic cohort Seguimiento Universidad de Navarra (SUN) and the average values for mental health increased with BMI and became statistically significant in unadjusted models.
Men showed higher scores than women in all scales, which is the same in other studies in abdominal obesity and type 2 diabetes, in the population over 65 years old and in the general population, both in national studies and in international studies.19,29,32,33
In physical components (physical functioning and physical role functioning), scales can be also observed that when the age increases the quality of life is decreased. Perhaps due to aging a loss of functional capacity is involved and is consistent with the rates of the Spanish population between 70 and 75 years old with disabilities or limitations, which represents 21.8% of total.25
This study has some limitations. First, it is an observational cross-sectional descriptive study, so it does not imply causality. Also, the participants in our study are not representative of the general population as they all have MetS. However, the high number of participants and that after 15 years the scores obtained in the HRQoL questionnaire follow the same concordance as the reference values for the Spanish population ≥60 years is a strength, as well as the correct validity and reproducibility to measure the quality of life related to the health of the SF-36 questionnaire.
In conclusion, we can say that our results may reflect that the MetS might have a negative influence dimensions of HRQoL, general health, bodily pain and vitality the same cannot be said about psychological dimensions, which are less affected. Furthermore, we observed that HRQoL in women was poorer than in men for several dimensions, particularly, in the bodily pain dimension and the physical role and vitality dimensions. Therefore, the approach from Primary Care consultations on the impact generated by the MetS on HRQoL together with their potential causes is fundamental, paying special attention to the differences between men and women in this associationsexes.
Registration of clinical trialsThe trial was registered in 2014 at the International Standard Randomized Controlled Trial (ISRCTN89898870).
Funding sourcesThe PREDIMED-Plus trial was supported by the Spanish government's official funding agency for biomedical research, ISCIII, through the Fondo de Investigación para la Salud (FIS), which is co-funded by the European Regional Development Fund (three coordinated FIS projects led by Jordi Salas-Salvadó and Josep Vidal, including the following projects: PI13/00673, PI13/00492, PI13/00272, PI13/01123, PI13/00462, PI13/00233, PI13/02184, PI13/00728, PI13/01090, PI13/01056, PI14/01722, PI14/00636, PI14/00618, PI14/00696, PI14/01206, PI14/01919, PI14/00853, PI14/01374, PI16/00473, PI16/00662, PI16/01873, PI16/01094, PI16/00501, PI16/00533, PI16/00381, PI16/00366, PI16/01522, PI16/01120, PI17/00764, PI17/01183, PI17/00855, PI17/01347, PI17/00525, PI17/01827, PI17/00532, PI17/00215, PI17/01441, PI17/00508, PI17/01732, PI17/00926), the Special Action Project entitled: Implementación y evaluación de una intervención intensiva sobre la actividad física Cohorte PREDIMED-PLUS grant to Jordi Salas-Salvadó, the European Research Council (Advanced Research Grant 2013–2018; 340918) grant to Miguel Ángel Martínez-Gonzalez, the Recercaixa grant to Jordi Salas-Salvadó (2013ACUP00194), grants from the Consejería de Salud de la Junta de Andalucía (PI0458/2013; PS0358/2016; PI0137/2018), the PROMETEO/2017/017 grant from the Generalitat Valenciana, the SEMERGEN grant and FEDER funds (CB06/03), Olga Castaner is funded by the JR17/00022 grant, ISCIII. Christopher Papandreou is supported by a postdoctoral fellowship granted by the Autonomous Government of Catalonia (PERIS 2016–2020 Incorporació de Científics i Tecnòlegs, SLT002/0016/00428). Cristina Bouzas received a Fernando Tarongí Bauzà Grant. José C. Fernández-García is supported by a research contract from Servicio Andaluz de Salud (SAS) (B-0003-2017).
Conflict of interestThe authors have declared that there are no competing interests.
Steering Committee:
J. Salas-Salvadó (Coordinator), M.A. Martínez-González, M. Fitó. E. Ros, FJ. Tinahones, D. Corella and R. Estruch.
Executive Committee:
J. Salas-Salvadó, M.A. Martínez-González, D. Corella, M. Fitó, J. Vioque, D. Romaguera, J.A Martínez, J. Wärnberg, J. Lopez-Miranda, R. Estruch, A. Bueno-Cavanillas, Á.M. Alonso-Gómez, J.A. Tur, FJ. Tinahones, L. Serra-Majem, V. Martin, J. Lapetra, C. Vázquez, X. Pinto, J. Vidal, L. Daimiel, M. Delgado-Rodríguez, M.A. Rubio and E. Ros.
Dietary and Lifestyle Intervention Committee:
J. Salas-Salvadó (chair), M.A. Martínez-González, M. Fitó and R. Estruch;
Dietary Intervention: J. Salas-Salvadó (chair), N. Babio, E. Ros, A. Sánchez-Tainta;
Physical Exercise: M. Fitó (chair), H. Schröder, A. Marcos, D. Corella, J. Warnberg;
Behavioral support: R. Estruch (chair), F. Fernández-Aranda, C. Botella and J. Salas-Salvadó.
Clinical Event Ascertainment Committee:
F. Arós (Chair), M. Aldamiz, A. Alonso-Gómez, L. Forga, A. García-Layana, J. Portu, J. Timiraos, A. González-Pinto, I. Zorrilla, M. Martínez-Kareaga, P. Seoane.
Chair: Dr. Fernando Arós
Cardiology: Dr. Angel Alonso-Gómez; Dr. Fernando Arós
Neurology: Dr. Juan Timiraos
Internal Medicine: Dr. Mikel Aldamiz; Dr. Joseba Portu
Endocrinology: Dr. Lluis Forga
Ophthalmology: Dr. Alfredo García-Layana
Psychiatry: Dr. Ana González Pinto; Dr. Iñaki Zorrilla
Oncology: Dr. Mireia Martínez; Dr. Patricia Seoane
Independent Data and Safety Monitoring Board:
M.J. Stampfer (Harvard School of Public Health), J. Sabate (Loma Linda University), A. Astrup (Copenhagen University), F. Fernandez-Aviles (Universidad Complutense of Madrid), X. Pi-Sunyer (Columbia University).
Support groups:
C. Botella, F. Fernandez-Aranda, R. Lamuela, A. Marcos, M. del Puy Portillo, E. Ros, G. Sáez, F. Arós, E. Gómez-Gracia
Rovira i Virgili University, Department of Biochemistry and Biotechnology, Human Nutrition Unit, University Hospital of Sant Joan de Reus, Pere Virgili Institute for Health Research, Reus, Spain: R. Pedret Llaberia, R. Gonzalez, R. Sagarra Álamo, F. París Palleja, J. Balsells, J.M. Roca, T. Basora Gallisa, J. Vizcaino, P. Llobet Alpizarte, C. Anguera Perpiñá, M. Llauradó Vernet, C. Caballero, M. Garcia Barco, M.D. Morán Martínez, J. García Rosselló, A. Del Pozo, C. Poblet Calaf, P. Arcelin Zabal, X. Floresví, M. Ciutat Benet, A. Palau Galindo, J.J. Cabré Vila, F. Dolz Andrés, M. Soler, M. Gracia Vidal, J. Vilalta J. Boj Casajuana, M. Ricard, F. Saiz, A. Isach, M. Sanchez Marin Martinez, E. Granado Font, C, Lucena Luque, C. Mestres Sola, N. Becerra-Tomás, G. Mestres, G. Mena-Sánchez, L. Barrubés Piñol, M. Gil Segura, C. Papandreou, N. Rosique-Esteban, S. Chig, I. Abellán Cano, A. Palau Galindo, V. Ruiz García, A. Salas-Huetos, I. Paz-Graniel, L. Sánchez Niembro, P. Hernandez-Alonso, S. Canudas, L. Camacho-Barcia, J. García-Gavilán, A. Díaz-López.
Department of Preventive Medicine and Public Health, University of Navarra-Navarra Institute for Health Research (IdiSNA), Pamplona, Spain: M. Ruiz-Canela, P. Buil-Cosiales, C. Razquin, M. Bes-Rastrollo, A. Sanchez Tainta, B. SanJulian Aranguren, E. Goñi, Z. Vázquez, I. Barrientos, M. Canales, A. Rico, J. Basterra Gortari, A. Garcia Arellano, J. Diez-Espino, O. Lecea-Juarez, J. Carlos Cenoz-Osinaga, J. Bartolome-Resano, A. Sola-Larraza, B. Cano-Valles, S. Eguaras, E. Pascual Roquet-Jalmar, H. Lancova, R. Ramallal, M.L. Garcia-Perez, V. Estremera-Urabayen, M.J. Ariz-Arnedo, C. Hijos-Larraz, C. Fernandez Alfaro, B. Iñigo-Martinez, R. Villanueva Moreno, S. Martin-Almendros, L. Barandiaran-Bengoetxea, C. Fuertes-Goñi, A. Lezaun-Indurain, M.J. Guruchaga-Arcelus, O. Olmedo-Cruz, B. Iñigo-Martínez, L. Escriche-Erviti, R. Ansorena-Ros, R. Sanmatin-Zabaleta, J. Apalategi-Lasa, J. Villanueva-Telleria, M.M. Hernández-Espinosa, I. Arroyo-Bergera, L. Herrera-Valdez, L. Dorronsoro-Dorronsoro.
Department of Preventive Medicine, University of Valencia, University Jaume I, Conselleria de Sanitat de la Generalitat Valenciana, Valencia, Spain: González JI, Portolés O, Ortega-Azorín C, Barragán R, Carrasco P, Asensio EM, Fernández-Carrión R, Coltell O, Sáiz C, Férriz E, González-Monje I, Giménez-Fernández F, Quiles L, Fernández-Lacruz R, Giménez-Alba I, Carratalá-Calvo A, Valero-Barceló C, Osma R, Antón F, Mir C, Sánchez-Navarro S, Navas J, González-Gallego I, Bort-Llorca L, Pérez-Ollero L, Giner-Valero M, Monfort-Sáez R, Nadal-Sayol J, Pascual-Fuster V, Martínez-Pérez M, Riera C, Belda MV, Medina A, Miralles E, Ramírez-Esplugues MJ, Rojo-Furió M, San Onofre N, Mattingley G, Delgado MA, Pages MA, Riofrío Y, Abuomar L, Blasco-Lafarga N, Valcarce AM, Medina MD, de Valcárcel S, Tormo N, Felipe-Román O, Lafuente S, Navío EI, Aldana G, Crespo JV, Llosa JL, González-García L, Raga-Marí R.
Cardiovascular Risk and Nutrition Research Group, Servicio de Endocrinología, IMIM (Hospital del Mar Medical Research Institute), Barcelona. Departament de Medicina, Universitat Autònoma de Barcelona, Barcelona, Spain: O. Castañer, M.A. Muñoz, A. Hernaéz, L. Torres, M. Quifer, R. Llimona, G Freixer, A. Pérez, M. Farràs, R. Elosua, J. Marrugat, J. Vila, I. Subirana, S. Pérez, A. Goday, J.J. Chillaron Jordan, J.A. Flores Lerroux, D. Benaiges Boix, Llauradó G, M. Farré, E. Menoyo, D. Muñoz-Aguayo, S. Gaixas, G. Blanchart, A. Sanllorente, M. Soria, J. Valussi, A. Cuenca, L. Forcano, A. Pastor, A. Boronat, S. Tello, M. Cabañero, L. Franco, H. Schröder, R. De la Torre, C. Medrano, J. Bayó, M.T. García, V. Robledo, P. Babi, E. Canals, N. Soldevila, L. Carrés, C. Roca, M.S. Comas, G. Gasulla, X. Herraiz, A. Martínez, E. Vinyoles, J.M. Verdú, M. Masague Aguade, E. Baltasar Massip, M. Lopez Grau, M. Mengual, V. Moldon, M. Vila Vergaz, R. Cabanes Gómez, Ciurana, M. Gili Riu, A. Palomeras Vidal, F. Peñas F., A. Raya, M.A. Sebastian, M. Valls.
Nutritional Epidemiology Unit, Miguel Hernandez University, ISABIAL-FISABIO, Alicante, Spain: M. Garcia de la Hera. M, S. Gonzalez-Palacios, L. Torres Collado, D. Valera Gran, L. Compañ Gabucio, L Notario-Barandiaran, A. Oncina Canovas, D. Orozco Beltran, S. Pertusa Martínez, A Asensio, Juan Manuel Zazo, C Gisbert Sellés, J Román Maciá, C Sánchez Botella, R Lloret Macián M.V Hernándis Marsán, B. Cloquell Rodrigo, M.C. Altozano Rodado N. Iranzo García, I. Candela García, R. Valls Enguix, E.P. Cases Pérez, C.M. López García, C. Tercero Maciá, A Pastor Morell, E. Alonso Bartolomé, JJ Ballester Baixauli, M.T. Cano Sánchez, B.E. Ayús Rojo, E. Pedro Cases Pérez, C. Tercero Maciá, L.A. Mira Castelló, I.A. García García, M. Jordá Ballesta, C. Pastor Polo, E. Puig Agulló
Hospital Son Espases (HUSE) and Institute for Health Research Illes Balears (IdISBa), Palma de Mallorca, Spain: A. Colom, J. Konieczna, M. Morey, R. Zamanillo, A.M. Galmés, V. Pereira, M.A. Martín, A. Yáñez, J. Llobera, J. Ripoll, R. Prieto, F. Grases, A. Costa, C. Fernández-Palomeque, E. Fortuny, M. Noris, S. Munuera, F. Tomás, F. Fiol, A. Jover, J.M. Janer, C. Vallespir, I. Mattei, N. Feuerbach, M. del Mar Sureda, S. Vega, L. Quintana, A. Fiol, M. Amador, S. González, J. Coll, A. Moyá.
Department of Nutrition, Food Sciences, and Physiology, Center for Nutrition Research, University of Navarra, Pamplona, Spain: I. Abete, I. Cantero, C. Cristobo, I. Ibero-Baraibar, M. Zulet, J. Ágreda Martínez, M.D. Lezáun Burgui, R. Bartolomé Resano, E. Cano Cáceres, T. Elcarte López, E. Echarte Osacain, B. Pérez Sanz, I. Blanco Platero, S.A. Andueza Azcárate, A. Gimeno Aznar, E. Ursúa Sesma, B. Ojeda Bilbao, J. Martinez Jarauta, L. Ugalde Sarasa, B. Rípodas Echarte, M.V. Güeto Rubio.
University of Málaga and Institute of Biomedical Research in Malaga (IBIMA), Málaga, Spain: F.J. Barón-López, J.C. Fernández García, N. Moreno-Morales, M. del C. Rodríguez-Martínez, J. Pérez-López, J.C. Benavente-Marín, E. Crespo Oliva, E. Contreras Fernández, F.J. Carmona González, R. Carabaño Moral, S. Torres Moreno, M.V. Martín Ruíz, M. Alcalá Cornide, V. Fuentes Gómez.
Lipids and Atherosclerosis Unit, Department of Internal Medicine, Maimonides Biomedical Research Institute of Cordoba (IMIBIC), Reina Sofia University Hospital, University of Cordoba, Cordoba, Spain: A. Garcia-Rios, J. Criado García, A.I. Jiménez Morales, N. Delgado Casado, A. Ortiz Morales, J.D. Torres Peña, F.J. Gómez Delgado, F. Rodríguez Cantalejo, J. Caballero Villaraso, J.F. Alcalá, P.J. Peña Orihuela, G. Quintana Navarro.
Department of Internal Medicine, Institut d’Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Hospital Clínic, University of Barcelona, Barcelona, Spain: R. Casas, M. Domenech, C. Viñas, S. Castro-Barquero, A.M. Ruiz-León, L. Tarés, A.I. Jordan, R. Soriano, M. Camafort, C. Sierra, E. Sacanella, A. Sala-Vila, J. M. Cots, I. Sarroca, M. García, N. Bermúdez, A. Pérez, I. Duaso, A. de la Arada, R. Hernández, C. Simón, M.A. de la Poza, I. Gil, M. Vila, C. Iglesias, N. Assens, M. Amatller, LL. Rams, T. Benet, G. Fernández, J. Teruel, A. Azorin, M. Cubells, D. López, J.M. Llovet, M.L. Gómez, P. Climente, L. de Paula, J. Soto, C. Carbonell, C. Llor, X. Abat, A. Cama, M. Fortuny, C. Domingo, A. I. Liberal, T. Martínez, E. Yañez, M. J. Nieto, A. Pérez, E. Lloret, C. Carrazoni, A. M. Belles, C. Olmos, M. Ramentol, M. J. Capell, R. Casas, I. Giner, A. Muñoz, R. Martín, E. Moron, A. Bonillo, G. Sánchez, C. Calbó, J. Pous, M. Massip, Y. García, M.C. Massagué, R. Ibañez, J. Llaona, T. Vidal, N. Vizcay, E. Segura, C. Galindo, M. Moreno, M. Caubet, J. Altirriba, G. Fluxà, P. Toribio, E. Torrent, J. J. Anton, A. Viaplana, G. Vieytes, N. Duch, A. Pereira, M. A. Moreno, A. Pérez, E. Sant, J. Gené, H. Calvillo, F. Pont, M. Puig, M. Casasayas, A. Garrich, E. Senar, A. Martínez, I. Boix, E. Sequeira, V. Aragunde, S. Riera, M. Salgado, M. Fuentes, E. Martín, A. Ubieto, F. Pallarés, C. Sala, A. Abilla, S. Moreno, E. Mayor, T. Colom, A. Gaspar, A. Gómez, L. Palacios, R. Garrigosa.
Department of Preventive Medicine and Public Health, University of Granada, Granada, Spain: L. García Molina, B. Riquelme Gallego, A. Maldonado Calvo, A. López Maldonado, E.M. Garrido, A. Baena Dominguez, F. García Jiménez, E. Thomas Carazo, A. Jesús Turnes González, F. González Jiménez, F. Padilla Ruiz, J. Machado Santiago, M.D. Martínez Bellón, A. Pueyos Sánchez, L. Arribas Mir, R. Rodríguez Tapioles, F. Dorador Atienza, L. Baena Camus, C. Osorio Martos, D. Rueda Lozano, M. López Alcázar, F. Ramos Díaz, M. Cruz Rosales Sierra, P. Alguacil Cubero, A. López Rodriguez, F. Guerrero García, J. Tormo Molina, F. Ruiz Rodríguez.
OSI ARABA, University Hospital Araba, Vitoria, Spain: J. Rekondo, I. Salaverria, A. Alonso-Gómez, M.C. Belló, A. Loma-Osorio, L. Tojal, P. Bruyel, A. Casi Casanellas, M.L. Arnal Otero, J. Ortueta Martínez De Arbulo, J. Vinagre Morgado, J. Romeo Ollora, J. Urraca, M.I. Sarriegui Carrera, F.J. Toribio, E. Magán, A. Rodríguez, S. Castro Madrid, M.T. Gómez Merino, M. Rodríguez Jiménez, M. Gutiérrez Jodra, B. López Alonso, J. Iturralde Iriso, C. Pascual Romero, A. Izquierdo De La Guerra.
Research Group on Community Nutrition & Oxidative Stress, University of Balearic Islands & IDISBA, Palma de Mallorca, Spain: M. Abbate, E. Angullo, E. Argelich, M.M. Bibiloni, X. Capó, S. Carreres, L. Gallardo, J.M. Gámez, B. García, C. García, S. García, A. Julibert, C. Gómez, I. Llompart, A. Martorell, C.M. Mascaró, D. Mateos, M, Monserrat, S. Montemayor, A. Pons, M. Quetglas, J. Ramos, T. Ripoll, T. Rodríguez, A. Sureda, S. Tejada, L. Ugarriza.
Virgen de la Victoria Hospital, University of Málaga, Málaga, Spain: M.R. Bernal López, M. Macías González, J. Ruiz Nava, J.C. Fernández García, A. Vilches Pérez, A. González Banderas, A.V. Alarcon-Matin, J. Alcaide Torres, A. Vargas Candela, M. García Ruiz de Mier, M. León Fernández, R. Hernández Robles, S. Santamaría Fernández, J.M. Marín, J.C. Villalobos, A. Ortiz.
University of Las Palmas de Gran Canaria, Las Palmas, Spain: J. Álvarez-Pérez, E.M. Díaz Benítez, F. Díaz-Collado, J. Pérez-Cabrera, L.T. Casañas-Quintana, R.B. García-Guerra, I. Bautista-Castaño, C. Ruano-Rodríguez, F. Sarmiento de la Fe, J.A. García-Pastor, B. Macías-Gutiérrez, I. Falcón-Sanabria, C. Simón-García, A.J. Santana-Santana, J.B. Álvarez-Álvarez, B.V. Díaz-González, J.M. Castillo Anzalas, R.E. Sosa-Also, J. Medina-Ponce.
Biomedicine Institute (IBIOMED); University of León, and Primary Health Care Management of León (Sacyl), León, Spain: S. Abajo Olea, A. Adlbi Sibai, M. Ajenjo, L. Álvarez, E. Carriedo Ule, N. Cubelos, V. Dávila-Batista, M. Escobar Fernández, P. Farias Cardoso, J.I. Ferradal García, J.P. Fernández Vázquez, F. González Rivero, C. Onrrubia Baticón, M. Lavinia Popescu, J.I. López Gil, J. López de la Iglesia, A.J. Molina, M. Piró, S. Reguero Celada, M. Rodríguez Bul, M. Rubín-García, A.A. Torres Serna, F. Vitelli-Storelli.
Department of Family Medicine, Distrito Sanitario Atención Primaria Sevilla, Sevilla, Spain: L. Miró-Moriano, C. Domínguez-Espinaco, S. Vaquero-Díaz, F.J. García-Corte, A. Santos-Calonge, C. Toro-Cortés, N. Pelegrina-López, V. Urbano-Fernández, M. Ortega-Calvo, J. Lozano-Rodríguez, I. Rivera-Benítez, M. Caballero-Valderrama, P. Iglesias-Bonilla, P. Román-Torres, Y. Corchado-Albalat, L. Mellado-Martín.
Department of Endocrinology, Foundation Jiménez-Díaz, Madrid, Spain: A.I. de Cos, S. Gutierrez, S. Artola, A. Galdon, I. Gonzalo.
Lipids and Vascular Risk Unit, Internal Medicine, University Hospital of Bellvitge, Hospitalet de Llobregat, Barcelona, Spain: M. Gimenez-Gracia, R. Figueras, M. Poch, R. Freixedas, F. Trias, I. Sarasa, M. Fanlo, H. Lafuente, M. Liceran, V. Esteve, A. Rodriguez-Sanchez, E. Gomez-Sanchez, C. Pallarols, J. Monedero, X. Corbella, E. Corbella.
Department of Endocrinology, IDIBAPS, Hospital Clinic, University of Barcelona, Barcelona, Spain: A. Altés, I. Vinagre, C. Mestre, J. Viaplana, M. Serra, J. Vera, T. Freitas, E. Ortega, I. Pla.
Nutritional Genomics and Epigenomics Group, Institute IMDEA-Food, CEI UAM+CSIC, Madrid, Spain: J.M. Ordovás, V. Micó, L. Berninches, J. Tapia, M.J. Concejo, J. Muñoz, M. Adrián, Y. de la Fuente, C. Albertos, E. Villahoz, M.L. Cornejo, C. Cuesta, A.Montero, M.C. Valdés.
Division of Preventive Medicine, University of Jaén, Jaén, Spain: J.J. Gaforio, S. Moraleda, N. Liétor, J.I. Peis, T. Ureña, M. Rueda, M.I. Ballesta.
Department of Endocrinology and Nutrition, Institute for Health Research Hospital Clínico San Carlos (IdISSC), Madrid, Spain: C. Moreno Lopera, C. Aragoneses Isabel, M.A. Sirur Flores, M. Ceballos de Diego, T. Bescos Cáceres, Y. Peña Cereceda, M. Martínez Abad, R. Cabrera Vélez, M. González Cerrajero, M.A. Rubio Herrera, M. Torrego Ellacuría, A. Barabash Bustelo, M. Ortiz Ramos, A. Larrad Sainz.
Department of Basic and Clinical Psychology and Psychobiology, University Jaume I, Castellón de la Plana, Spain: R. Baños, A. García-Palacios.
Oxidative Pathology Unit. Department of Biochemistry and Molecular Biology, School of Medicine-INCLIVA, Service of Clinical Analyses, University Hospital Doctor Peset, Valencia, Spain. University of Valencia, Valencia Spain: G. Sáez Tormo (Sáez GT), N. Estañ-Capell, A. Iradi Casal, L. Monzó Beltrán, M. Fandos Sánchez, E. Alonso Iglesias, D. Acevedo León, A. Hernando Espinilla, A. Mora Herranz, C. Cerdá Micó.
Department of Preventive Medicine, University of Malaga, Malaga, Spain: J. Fernández-Crehuet Navajas, M. Gutiérrez Bedmar, A. García Rodriguez, A. Mariscal Larrubia, M. Carnero Varo, C. Muñoz Bravo.
Department of Psychiatry, University Hospital of Bellvitge, Barcelona, Spain:
F. Fernández-Aranda, S. Jiménez-Murcia, N. Mallorqui-Bagué, R. Granero, Z. Agüera, M. Lozano-Madrid.