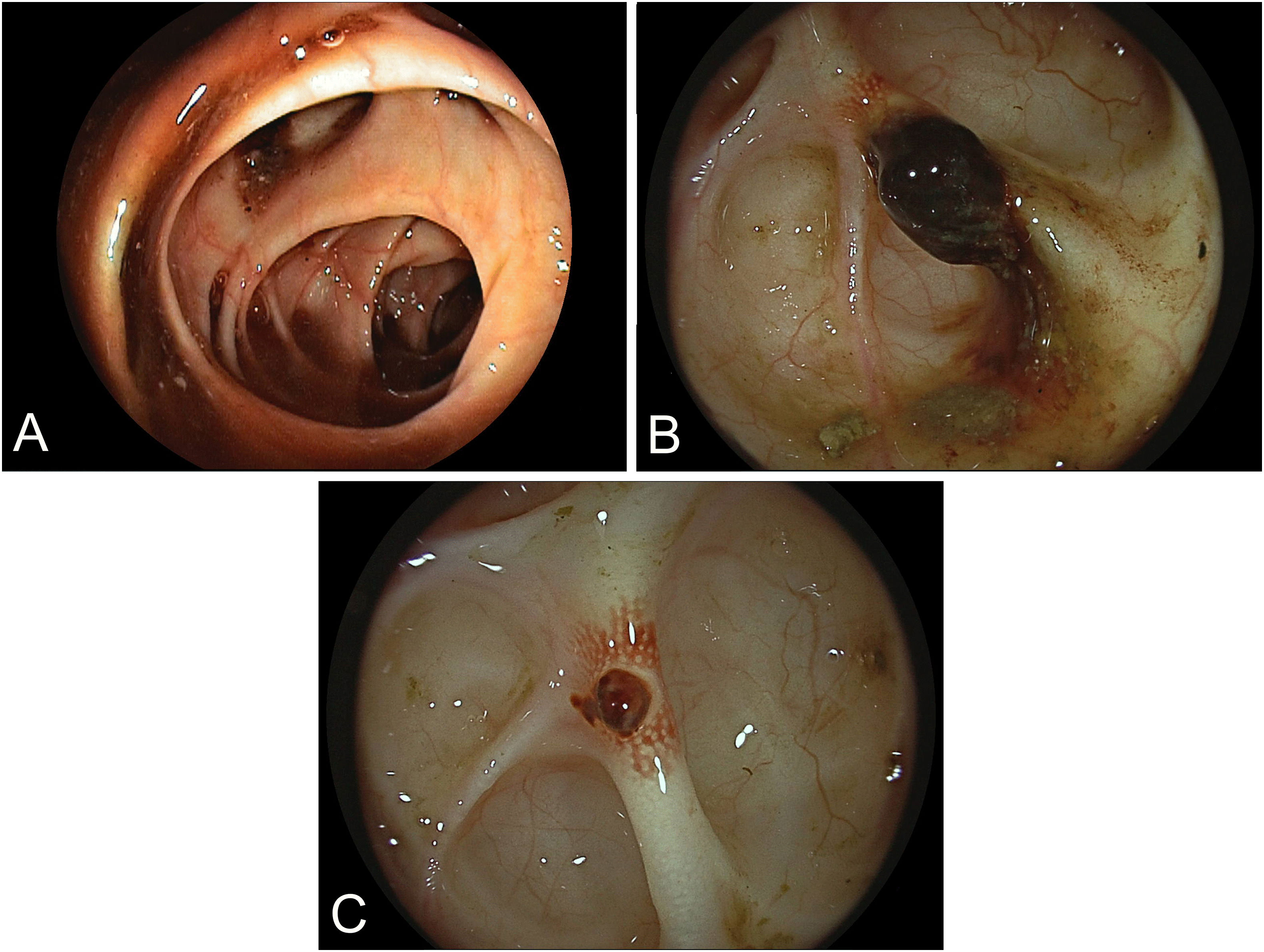
An 89-year-old male patient presented with signs of incipient shock and lower gastrointestinal bleeding (hemoglobin drop to as low as 5.6 g/dL). After stabilization and rapid bowel cleansing in the intensive care unit, the patient underwent early bedside colonoscopy, revealing multiple diverticulae throughout the colon with stigmata of subacute hemorrhage. (Fig. 1A) However, while a clinical diagnosis of colonic diverticular bleeding was firmly established, the distinct bleeding source was not pinpointed. Despite apparent spontaneous resolution in the short-term, the patient underwent repeat colonoscopy the following day after intensification of bowel cleansing. Beginning from the lower sigmoid, multiple individual larger diverticulae were gently intubated with the tip of the endoscope. In the mid-sigmoid, a large intra-divertiular adherent clot was detected in a voluminous diverticulum. (Fig. 1B) After intensive washing using a water jet system, the clot detached revealing a large-caliber vessel underneath, analogous to a Forrest IIa situation in ulcer bleeding. (Fig. 1C) The lesion was provided with two hemo-clips for vessel-directed endoscopic hemostasis. The further clinical course was unremarkable, and the patient was discharged three days later.
Depending on patients age, colonic diverticular bleeding overall ranks amongst the most common causes of lower gastrointestinal bleeding with a high propensity for spontaneous cessation. Notwithstanding, early endoscopic diagnosis is warranted and instrumental in excluding alternative sources of bleeding. Since the distinct bleeding diverticulum may not be readily identifiable, endoscopic treatment is only occasionally achievable with different techniques appropriate relative to the given anatomy, e.g. clipping of visible vessels or band ligation of small-necked diverticulae with visible bleeding.