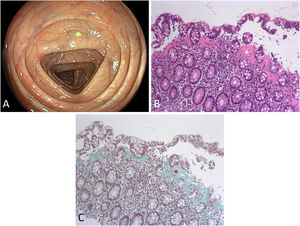
A 71-year-old female presented for diarrhea for >3 months passing up to 10 watery stools daily. Microbial stool analysis proved negative with fecal calprotectin slightly elevated (64μg/g; normal<50). Celiac serology and duodenal histology were unremarkable, while gastric biopsies revealed chronic H. pylori-negative gastritis. Ileocolonoscopy yielded normal endoscopic findings with preserved vascular pattern as exemplified in transverse colon. (A) Endoscopic biopsies were taken from ascending and sigmoid colon. Conventional histopathology indicated surface damage of detached superficial epithelium with preserved crypt architecture and insignificant intraepithelial lymphocytosis. (B, H&E, ×50) Of note, there was marked subepithelial collagenous band thickening>10μM additionally highlighted by ancillary stainings, warranting a diagnosis of collagenous colitis. (C, Masson's trichrome, ×50) Medication review indicated 8mg candesartan with angiotensin II receptor blockers rarely linked to microscopic colitis (MC)-like enteropathies. However, empirical switching to angiotensin converting enzyme inhibition yielded no clinical benefit within two weeks. Therefore, the patient was successfully treated with 9mg budesonide as the single licensed medication (Fig. 1).
With watery diarrhea as the lead symptom, collagenous colitis locates within the spectrum of MCs attributable to dysregulated immune reaction to luminal antigens. Mostly affecting elderly female patients, endoscopic findings are near- or completely normal, thus an adequate endoscopic biopsy protocol and pathology assessment is key to early diagnosis.
Conflict of interestNothing to declare.