Lung involvement in rheumatologic disease in children has been described with low frequency.
ObjectiveTo describe the lung function test and the radiological findings in a group of paediatric patients with rheumatologic diseases.
MethodsDescriptive study. Pulmonary function was evaluated with spirometry, carbon monoxide diffusing capacity, blood arterial gas at rest and post exercise in addition to chest radiography and high resolution computed tomography were performed in children with rheumatologic disease.
ResultsOf the fourteen patients studied: 11 were diagnosed with juvenile idiopathic arthritis (JIA), two with systemic lupus erythematosus (SLE), and one with juvenile dermatomyositis (JDM). Mean age: 13 years (range 7–18 years). Nine females, duration of disease 4±2.8 years (range 1–11 years). Four patients had any grade of abnormalities in one or more lung function tests and/or radiological test.
ConclusionWe recommend routine checks of pulmonary function in all patients with rheumatologic diseases even in the absence of respiratory symptoms.
Lung function tests have been used for the diagnosis, monitoring and treatment evaluation of a number of chronic lung diseases in children, such as asthma, cystic fibrosis, and interstitial pneumonitis. For each of these methods, there are standard procedures and reference values adjusted to normal population by age, sex, and height.1–3 Rheumatic diseases are a group of immunologically mediated inflammatory disorders associated with a large variety of affected organs.3
There are few descriptions of lung injuries in children with rheumatic disease, which incidentally may be affecting all its components such as airways, vessels, parenchyma, pleura, and respiratory muscles.4–9 Juvenile idiopathic arthritis, systemic lupus erythematosus, juvenile dermatomyositis, and systemic sclerosis are the most frequent rheumatic illnesses associated with lung compromise.1,2,4,5
This impairment can be related to the illness itself, drugs used in treatment, or secondary to infections between others.7,8
In adults, rheumatoid arthritis has been associated with mild restrictive defects, diffuse interstitial lung diseases, pulmonary vasculitis, and bronchiolitis obliterans. These alterations have also been observed in juvenile idiopathic arthritis.10,11
In childhood, lung impairment can be found in active diseases even in the absence of abnormalities in chest radiographs or in lung function tests such as diffusing capacity, lung volumes, low forced ventilatory flows and saturation in exercise.9
ObjectiveTo describe the lung function test and radiological findings in children in treatment for at least one year from diagnosis of some rheumatic disease stable in the preceding six months.
MethodsStudy populationFourteen patients attending the Immunology Department of Exequiel Gonzalez Cortes Children's Hospital (Santiago, Chile) were enrolled: 11 diagnosed with juvenile idiopathic arthritis (JIA) of different clinical form (three systemic, two oligoarticular, two polyarticular, and four enthesitis-related arthritis) according to the International League Association for Rheumatology classification12; two diagnosed with systemic lupus erythematosus (SLE) according to American Rheumatology Academic criteria updated by Hochberg13; and one diagnosed with juvenile dermatomyositis (JDM) according to Pearson criteria modified by Bohan and Peter.3 Age of onset and history of treatment were recorded. None had history of chronic lung disease before the onset of the rheumatic disease.
Lung functionIn all patients spirometry was obtained using a Med Graphics Breeze V 3.7 spirometer, and the best values of at least three technically well-performed flow-volume curves were used. Reference values of Gutierrez for Chilean populations of healthy children 4–18 years were applied14 and range 80–120% for reference values were considered normal.
Carbon monoxide diffusing capacity of lung (DLCO) and DLCO/alveolar volume (VA) were determined using a standardised single-breath technique (Master Screen Body V 4.3 Jaeger). Reference values from Zapletal for populations of healthy children aged 4–18 years were used15 and range 80–120% for reference values were considered normal
Blood arterial gases at rest and exercise were performed in the subjects before and after a run on a treadmill for three minutes after reaching submaximal heart rate. Reference values of Graef were used.16
In two cases with signs of hypoventilation, strength of respiratory muscles was assessed by measuring maximum static respiratory mouth pressures with a tube mouthpiece attached to pressure gauge. The absolute peak pressure for inspiratory effort (Pi max) was recorded and compared with reference values of Szeinberg.17 This test is used in our country as part of the evaluation of lung involvement in children with neuromuscular diseases.
Radiology testChest radiography and chest high resolution computed tomography (HRCT) were interpreted by two blinded radiologists.
The protocol was approved by the local Ethics Committee and written consent for participation in the study was obtained from their parents.
Statistical analysesAll variables were presented as means±SD. The results from the lung function test were expressed as a percentage of reference values.
Epi Info 6.0 and Stata 10.0 were used for data analysis. Percentages and Fisher exact test were used for qualitative nominal variables such as gender differences. T student test was applied for gauge variation with mean and standard deviation and average comparison.
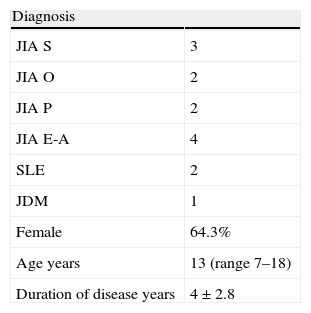
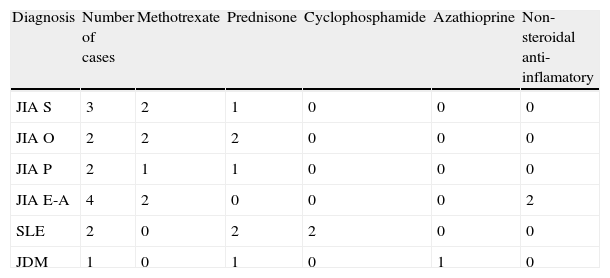
ResultsFourteen children were included (Table 1). Mean age was 13 years (range 7–18 years), nine females. Duration of disease was 4±2.8 years (range 1–11 years). Among these 14 children: nine had normal results in all lung function and radiologic tests (diagnoses JIA 8, JDM 1). Table 2 details the treatment being received at time of study. Seven JIA patients were receiving methotrexate, as well as low doses of prednisone in four; two lupus patients were treated with cyclophosphamide pulses plus prednisone during pulmonary evaluations.
Characteristics of the study population.
| Diagnosis | |
| JIA S | 3 |
| JIA O | 2 |
| JIA P | 2 |
| JIA E-A | 4 |
| SLE | 2 |
| JDM | 1 |
| Female | 64.3% |
| Age years | 13 (range 7–18) |
| Duration of disease years | 4±2.8 |
JIA=juvenile idiopathic arthritis; S=systemic; O=oligoarticular; P=polyarticular; E-A=enthesitis-related; SLE=systemic lupus erythematosus; JDM=juvenile dermatomyositis.
Current pharmacological treatment.
| Diagnosis | Number of cases | Methotrexate | Prednisone | Cyclophosphamide | Azathioprine | Non-steroidal anti-inflamatory |
| JIA S | 3 | 2 | 1 | 0 | 0 | 0 |
| JIA O | 2 | 2 | 2 | 0 | 0 | 0 |
| JIA P | 2 | 1 | 1 | 0 | 0 | 0 |
| JIA E-A | 4 | 2 | 0 | 0 | 0 | 2 |
| SLE | 2 | 0 | 2 | 2 | 0 | 0 |
| JDM | 1 | 0 | 1 | 0 | 1 | 0 |
JIA=juvenile idiopathic arthritis; S=systemic; O=oligoarticular; P=polyarticular; E-A=enthesitis-related; SLE=systemic lupus erythematosus; JDM=juvenile dermatomyositis.
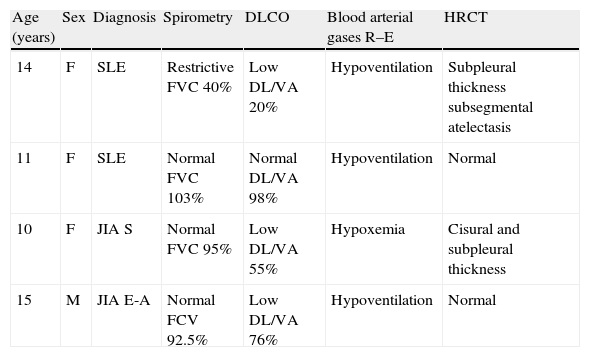
In four cases (28.6%, SLE 2, JIA 2) we found abnormal test (Table 3). One patient with SLE showed forced vital capacity (FVC) and forced expiratory volume in 1s (FEV1) lower than reference values compatible with restrictive defects; in this case, the other lung function test and radiology test were abnormal too. She had reduction in DLCO and evidence of hypoventilation in blood arterial gases at rest and exercise, and the value of maximal inspiratory pressure (Pi max) was lower than the reference values. In the other SLE patient we found signs of hypoventilation in the blood arterial gases at rest and exercise. In this case the other lung function test was normal and the Pi max could not be performed by the child. One JIA with enthesitis-related clinical form (E-A) patient had reduction in DLCO and hypoventilation signs in blood arterial gas at rest and post exercise. In this case the maximal inspiratory pressure (Pi max) values were lower than the reference. One AIJ with systemic clinical form patient had hypoxemia in blood arterial gases at rest and low DLCO.
Results of abnormal lung function tests and radiologic test.
| Age (years) | Sex | Diagnosis | Spirometry | DLCO | Blood arterial gases R–E | HRCT |
| 14 | F | SLE | Restrictive FVC 40% | Low DL/VA 20% | Hypoventilation | Subpleural thickness subsegmental atelectasis |
| 11 | F | SLE | Normal FVC 103% | Normal DL/VA 98% | Hypoventilation | Normal |
| 10 | F | JIA S | Normal FVC 95% | Low DL/VA 55% | Hypoxemia | Cisural and subpleural thickness |
| 15 | M | JIA E-A | Normal FCV 92.5% | Low DL/VA 76% | Hypoventilation | Normal |
JIA=juvenile idiopathic arthritis; S=systemic; E-A=enthesitis-related; SLE=systemic lupus erythematosus; FVC=forced vital capacity; DL=diffusion lung; VA=ventilation alveolar; DLCO=diffusion lung carbon monoxide; R–E=rest–exercise; HRCT=high resolution computed tomography.
In two patients chest radiography and chest HRCT abnormalities were demonstrated: two SLE patients had pleural compromise. One of them was associated with sub-segmental atelectasis. One JIA case had an asymptomatic sub-pleural nodule but this observation was considered a normal finding because the other functional respiratory tests were also normal.
We found no statistically significant risk factors for pulmonary injuries, probably due to the small number of cases.
DiscussionIn our study, one third (4/14) of the patients had any grade of abnormalities in the lung function test and/or radiologist test even when they did not show clinical respiratory symptoms in the last six months. It is also remarkable that there were no respiratory clinical symptoms shown in four patients.
In SLE patients, alterations compatible with early interstitial lung disease in DLCO were found without anomalies on HRCT at this stage. The hypoventilation found in two SLE patients is described in adult patients as a compromise of inspiratory muscles function associated with diaphragmatic dysfunction on the basis of the demonstration of decreased inspiratory muscles strength in eleven SLE patients for Wilcox.18 On the other hand, Laroche et al.19 failed to demonstrate diaphragm weakness. In children this alteration has also been described, but the origin is not yet clear.2,3,20–25 We cannot rule out the possible side effects of corticosteroids used over long periods in the respiratory muscles weakness, even though we find no evidence for this statement. On the other hand the assessment of inspiratory muscles in children receiving steroid treatment for long periods has been not studied, so probably if this test was done routinely information could be gathered about this possibility.
Lung compromise in children is infrequent in different following trials reporting 14–31% of pulmonary illness. The most common alteration is pleural compromise with pleural effusion in 12%; the interstitial pneumonitis had been considered a less common alteration with reports of between 1% and 14%.26,27
Lilleby et al.21 in a study including 46 SLE patients found abnormal DLCO in 26% as the most frequently abnormal lung function test and in one case this was associated to restrictive ventilatory pattern.
The low frequency of HRCT abnormalities in relation to the DLCO test's alteration was also reported by Lilleby.
The alterations in two JIA cases were compatible with early interstitial lung diseases, the most common features observed in adults with rheumatic disorders. However Knook at al.22 found no alteration in DLCO in 31 patients with juvenile idiopathic arthritis.
Due to the small number of children studied, we were unable to assess the potential impact of drugs on lung function describes for methotrexate, non-steroidal anti-inflammatory drugs or corticosteroids, especially in adults.2,5,28 In this series, one JIA with systemic form had been in treatment for the last two years with methotrexate and methylprednisolone and the other JIA with E-A form received non-steroidal anti-inflammatory intermittent treatment during 20 months and methotrexate for 17 months.
Although some bias could be attributable to small size and the heterogeneous population studied, the consecutive inclusion and prospective detailed pulmonary investigations with blinded review of test seem sufficient strength to us to guarantee the main conclusions.
We suggest the routine evaluation of pulmonary function in all patients with rheumatic diseases at least once a year, even in the absence of respiratory symptoms, in order to detect early alteration, optimise the treatment and prevent possible related complications.
Conflict of interestThe authors declare no potential conflicts of interest.