We aimed to identify factors associated with recurrent wheezing (RW) in infants in the first year of life living in the Southern region of São Paulo city and participating in the “Estudio Internacional de Sibilancias en Lactantes (EISL)” – phase 3 (P3).
Methods1335 parents of infants who were attended in primary care health units in the Southern region of São Paulo city from 2009 to 2010 answered the EISL-P3 written questionnaire. The wheezing group was stratified in accordance to the frequency of wheezing episodes as occasional wheezing (OW, less than three episodes), or RW (three or more episodes). Wheezing-associated factors were evaluated using multivariate analysis and were expressed as odds ratio (OR) and 95% confidence interval (95%CI).
ResultsThe most relevant factors related to OW were pneumonia (OR=3.10, 95%CI=1.68–5.73), hospitalisation due to pneumonia (OR=2.88, 95%CI=1.26–6.56) and recurrent upper respiratory infection (URI, OR=1.87, 95%CI=1.25–2.81). Regarding RW, recurrent URI (OR=5.34, 95%CI=3.83–7.45), pneumonia (OR=4.06, 95%CI=2.87–5.74) and asthmatic siblings (OR=3.02, 95%CI=1.67–5.45) were the most significantly associated factors.
ConclusionsIn the present study, we found that recurrent URI, positive history of pneumonia and familiar history of asthma were the most relevant factors associated with RW. The precocious knowledge of these factors can enable the identification of the probable asthmatic infants and can improve both prevention strategies and treatment of these patients.
Wheezing disorders are the main reasons for visits to the emergency room and hospitalisation during the first years of life in developed and in developing countries, thus having a considerable economic impact.1
Children with recurrent wheezing (RW), characterised by presenting three or more episodes, have been identified as high risk for developing asthma.2,3
Consequently, the development of tools that allow the recognition of potential wheezing-associated factors, especially in the recurrent form, and the identification of these patients is essential.4
The Estudio Internacional de Sibilancias en Lactantes (EISL) or International Study of Wheezing in Infants was designed to study the impact of RW in infants and to identify its prevalence and associated factors. EISL is a multicentre, cross-sectional, international study that was carried out using a standardised and validated written questionnaire (WQ) in all of the participating centres. EISL phase 1 (EISL-P1) WQ is composed by 45 questions regarding demographic characteristics, respiratory symptoms, use of medication and possible factors associated with wheezing.5
EISL phase 3 (EISL-P3) was designed to occur 5 years after EISL-P1 to evaluate time trends in the prevalence of wheezing and to identify new factors associated in the same demographic region. EISL-P3 WQ is similar to that applied in P1 with five new questions added regarding the use of paracetamol and antibiotics.
EISL-P1 included 30,093 infants. The prevalence of at least one episode of wheezing and of RW was 45.2% and 20.3%, respectively. Notably, wheezing was more prevalent and more severe in Latin American countries than in European countries.6 In Brazil, many centres had participated in EISL-P1. In the city of São Paulo, the study was conducted in the Southern region between 2005 and 2006.7,8 Few studies have evaluated the factors associated with wheezing in this age group in Brazil and Latin America, mainly using a standardised protocol able to compare results.
The present study was tailored to identify factors associated with RW in infants living in the Southern region of São Paulo city from 2009 to 2010 (EISL-P3).
Materials and methodsParents or caregivers of infants from 12 to 15 months old, living in the Southern region of São Paulo city, answered the standardised EISL-P3 WQ through interviews. The children were randomly selected during routine childcare visits or vaccination, from June 2009 to December 2010. 1543 parents were invited to participate to this study and 208 refused. 1135 agreed to participate and signed a written consent form. The parents participating in the study were interviewed by five paediatricians specialised in Allergy and Clinical Immunology.
Children whose parents informed of chronic diseases that could influence the respiratory system were not included in the study.
During the EISL-P1, nine primary care health units, among 60, were randomly selected from the chosen region to have the questionnaires answered.7 In the present study, the same units were selected.
It was established by the study coordinators that the sample should include no less than 1000 infants. The sample size was based on the International Study of Asthma and Allergies in Childhood (ISAAC), considering the prevalence of wheezing by 30% and 25% in two different centres, with study effect of 95% and significance level of 1% for this sample in order to ensure adequate power for comparisons between centres and countries, even for questions with low prevalence of positive responses.5,9
Data from the EISL-P3 WQ were standard codified and transferred to a Microsoft Excel 2007 database. Infants were initially allocated in two groups: wheezing (presented at least one episode of wheezing) and “no wheezing”. Wheezing was stratified by the frequency of wheezing episodes in: occasional wheezing (OW, less than three episodes) or recurrent wheezing (RW, had three or more episodes).
Statistical analysis was performed using the Statistical Package for the Social Science (SPSS) for Windows – version 17.0. as follows: absolute and relative frequencies for categorical variables; for numeric variables, summary statistics, such as mean and standard deviation, were shown. In order to verify the association between the categorical factors and wheezing, the Chi-square test and Fisher's exact test were used.
To identify factors associated with wheezing, logistic regression was performed. Wheezing was considered a dependent variable and other predictor variables were considered for modelling. Subsequently, these variables were excluded by the order of significance (backward method). The goodness of fit test was performed using the Hosmer–Lemeshow's test. For all of the statistical analysis, the significance level of 5% was adopted.
The Research Ethics Committee at the Federal University of São Paulo-EPM/UNIFESP approved this study.
ResultsIn EISL-P3, 1335 questionnaires were considered valid. Of these, 596 (44.6%) had at least one episode of wheezing. The prevalence of OW and RW in the first year of life was 23.0% and 21.6%, respectively.
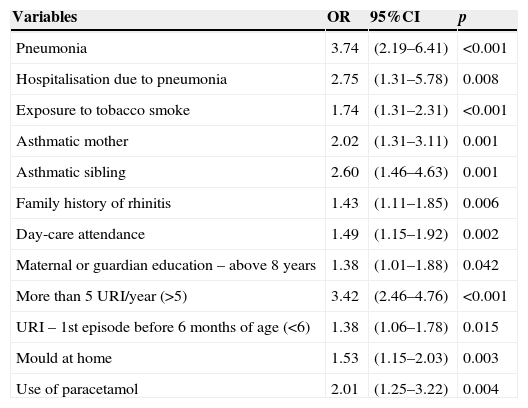
The factors associated with wheezing as a whole are detailed in Table 1. The gender of the infant, the presence of phone or carpet at home, consumption of processed foods, or presence of dog, cat or other animal did not show relevance in the final model of logistic regression. Antibiotic treatment was used during the wheezing episodes in 84% of this group. 20% of the infants were hospitalised due to pneumonia and 32% due to wheezing disorder. Additionally, 91 infants had a positive medical history of both types of hospitalisation.
Risk factors significantly associated with wheezing in infants from the Southern region of São Paulo city – International Study of Wheezing in Infants (EISL) – phase 3.
| Variables | OR | 95%CI | p |
|---|---|---|---|
| Pneumonia | 3.74 | (2.19–6.41) | <0.001 |
| Hospitalisation due to pneumonia | 2.75 | (1.31–5.78) | 0.008 |
| Exposure to tobacco smoke | 1.74 | (1.31–2.31) | <0.001 |
| Asthmatic mother | 2.02 | (1.31–3.11) | 0.001 |
| Asthmatic sibling | 2.60 | (1.46–4.63) | 0.001 |
| Family history of rhinitis | 1.43 | (1.11–1.85) | 0.006 |
| Day-care attendance | 1.49 | (1.15–1.92) | 0.002 |
| Maternal or guardian education – above 8 years | 1.38 | (1.01–1.88) | 0.042 |
| More than 5 URI/year (>5) | 3.42 | (2.46–4.76) | <0.001 |
| URI – 1st episode before 6 months of age (<6) | 1.38 | (1.06–1.78) | 0.015 |
| Mould at home | 1.53 | (1.15–2.03) | 0.003 |
| Use of paracetamol | 2.01 | (1.25–3.22) | 0.004 |
URI – upper respiratory infection, OR – odds ratio, 95%CI – 95% confidence interval.
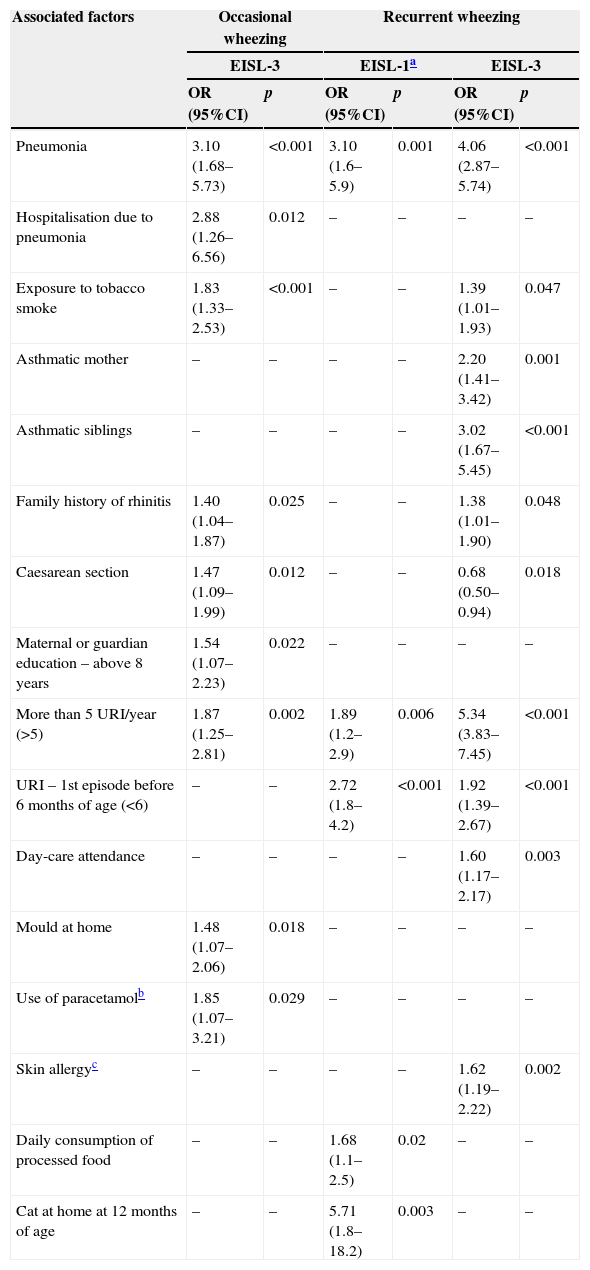
Table 2 describes factors associated to OW and to RW identified in the present study after multivariate analysis. In addition to the variables described in the table, the child's gender, the presence of air conditioning at home, the presence of carpet and exclusive breastfeeding for more than 6 months showed no relevance in the final model of logistic regression in this sampling.
Risk factors significantly associated with occasional or recurrent wheezing from the Southern region of Sao Paulo city infants during the first year of age – comparison with phases 1 and 3 of the International Study of Wheezing in Infants (EISL).
| Associated factors | Occasional wheezing | Recurrent wheezing | ||||
|---|---|---|---|---|---|---|
| EISL-3 | EISL-1a | EISL-3 | ||||
| OR (95%CI) | p | OR (95%CI) | p | OR (95%CI) | p | |
| Pneumonia | 3.10 (1.68–5.73) | <0.001 | 3.10 (1.6–5.9) | 0.001 | 4.06 (2.87–5.74) | <0.001 |
| Hospitalisation due to pneumonia | 2.88 (1.26–6.56) | 0.012 | – | – | – | – |
| Exposure to tobacco smoke | 1.83 (1.33–2.53) | <0.001 | – | – | 1.39 (1.01–1.93) | 0.047 |
| Asthmatic mother | – | – | – | – | 2.20 (1.41–3.42) | 0.001 |
| Asthmatic siblings | – | – | – | – | 3.02 (1.67–5.45) | <0.001 |
| Family history of rhinitis | 1.40 (1.04–1.87) | 0.025 | – | – | 1.38 (1.01–1.90) | 0.048 |
| Caesarean section | 1.47 (1.09–1.99) | 0.012 | – | – | 0.68 (0.50–0.94) | 0.018 |
| Maternal or guardian education – above 8 years | 1.54 (1.07–2.23) | 0.022 | – | – | – | – |
| More than 5 URI/year (>5) | 1.87 (1.25–2.81) | 0.002 | 1.89 (1.2–2.9) | 0.006 | 5.34 (3.83–7.45) | <0.001 |
| URI – 1st episode before 6 months of age (<6) | – | – | 2.72 (1.8–4.2) | <0.001 | 1.92 (1.39–2.67) | <0.001 |
| Day-care attendance | – | – | – | – | 1.60 (1.17–2.17) | 0.003 |
| Mould at home | 1.48 (1.07–2.06) | 0.018 | – | – | – | – |
| Use of paracetamolb | 1.85 (1.07–3.21) | 0.029 | – | – | – | – |
| Skin allergyc | – | – | – | – | 1.62 (1.19–2.22) | 0.002 |
| Daily consumption of processed food | – | – | 1.68 (1.1–2.5) | 0.02 | – | – |
| Cat at home at 12 months of age | – | – | 5.71 (1.8–18.2) | 0.003 | – | – |
URI – upper respiratory infection, OR – odds ratio, 95%CI – 95% confidence interval.
Positive medical history of pneumonia, hospitalisation due to pneumonia and frequent upper respiratory infection (URI) were the most significant factors associated with OW. Regarding RW, pneumonia and a positive medical history of asthmatic siblings were the most expressive factors (Table 2).
When the factors associated with OW and RW were compared, the positive family history of asthma (mother and siblings), more than five episodes of URI in the first year of life, day-care attendance and skin allergy were associated only to RW (Table 2). It should be highlighted that birth by caesarean section (C-section) showed distinct behaviour, i.e., associated risk for OW and protective effect for RW.
Still concerning RW, 92% of this group used antibiotics during wheezing episodes.
DiscussionIn our study, positive medical history of pneumonia, more than five episodes of URI, exposure to tobacco smoking and family history of rhinitis are significant factors associated to both OW and RW, albeit with distinct intensities (Table 2). These factors alone are not sufficient to distinguish RW from OW in these infants.
Previous history of pneumonia has been identified as a factor associated with wheezing by other centres participating in EISL,10–12 even in the presence of hospitalisation due to pneumonia.11 It is broadly recognised that some symptoms are shared in wheezing disorders and respiratory infections in children, especially infants, making it difficult to correctly diagnose and treat. In fact, the large number of hospitalisations due to pneumonia and wheezing observed in the present study seem to corroborate this notion. Nevertheless, there is evidence that recurrent episodes of wheezing can be a predisposition to childhood pneumonia.13,14
Conversely, frequent URI was also identified as a factor associated with wheezing in other Brazilian centres.11,12,15,16 Respiratory infections are common in childhood, particularly during the first year of life, which is related to the immaturity of innate and adaptive immunity.17–21 The sooner the respiratory system is attacked by infectious agents, the greater the structural and inflammatory involvement will be. Depending on the infectious agent, the immune response may favour the release of pro-inflammatory cytokines and proliferation of T helper type 2 cells, thus facilitating the development of asthma.19
Although a great number of children wheeze during respiratory infections, the persistence of wheezing and its progression to asthma results from a complex interaction between genetic inheritance and environmental exposure.
Additionally, it has already been described that the social contact with other infants may favour the precipitate exposure to infectious agents such as virus. Thus, day-care attendance or having an older sibling may favour infections and facilitate wheezing. To this date, unfortunately there is no consistent evidence for progression to asthma.22
With regard to being born by C-section, there is evidence suggesting a possible association with childhood asthma. Our results showed that delivery by C-section is an associated factor for OW, while being a protective factor for RW. These results are intriguing and invite further investigation.23
Passive exposure to tobacco smoking is a risk factor for wheezing and asthma. A recent meta-analysis observed that exposure to tobacco smoking induces a 20% fold increase in the incidence of wheezing disorders and asthma in children and young people.24 In relation with this data, some evidence has also demonstrated that exposure to mould is a risk factor associated with wheezing and asthma development.1
As previously mentioned, questions regarding the use of paracetamol and antibiotics were included in the EISL-P3 WQ. We verified that the use of paracetamol was considered a risk factor associated with wheezing. Epidemiological studies have shown that development of asthma is associated with regular use of antibiotics and paracetamol during childhood. Paracetamol can induce a decrease of glutathione levels, an enzyme that helps to repair oxidative damage in the airways and can lead to inflammation when presented in a lower concentration.25 Nevertheless, the association between asthma and early use of paracetamol may be inaccurate, a finding that warrants additional investigation.26
The association between wheezing/asthma and use of antibiotics is also controversial. While the distinction between wheezing episodes caused by bacterial or viral infection are still demanding, antibiotics have been frequently prescribed even without strict indication. Hence, it can be argued whether the use of antibiotics during childhood may be necessarily associated with subsequent asthma development and future investigations are needed to clarify this issue.27 Here, the use of antibiotics did not integrate with the final model analysis for RW because it could not be included as a predictor variable (in which a factor would be a cause, not a consequence of wheezing) due to the large number of infants with RW treated with antibiotics during the wheezing episodes.
Comparing factors associated with OW and RW, it can be verified that a positive family history of asthma (mother or siblings), skin allergy, URI before 6 months of age and attending day-care are exclusively associated with RW. In other words, these factors can identify among infants who wheeze in the first year of life, those with a higher risk of developing asthma.
The asthma predictive index was developed from the prospective Tucson Children's Respiratory Study2 to predict future asthma among infants with RW. The parental history of asthma and the presence of atopic eczema are major criteria for this index.28
We acknowledge the limitations of our study, including the fact that, as previously mentioned, cross-sectional studies may lead to a bias of reverse causality. Prospective studies should be performed for a better understanding concerning the risk factors that are associated with wheezing.
The use of a WQ that was vulnerable to the memory of parents and/or caregivers may produce information bias. However, some studies have already demonstrated that parents are able to accurately recall information regarding the diseases of their children.29 Epidemiological studies that employ questionnaires are valuable tools that have a low cost for generating information that can lead to improvement in public policies. They constitute an instrument of great value particularly in developing countries. Notably, the fact that the EISL-P3 WQ was constituted by questions concerning the first year of age, and was applied to parents whose infants were at the age of 12–15 months, may have minimised the possible memory bias.
The parents and/or caregivers may have confused wheezing with other respiratory sounds, consequently leading to an overestimation of the prevalence of wheezing. On the other hand, a shortened version of the EISL WQ has identified good agreement between the perception of parents and the medical diagnosis after auscultation, which was necessary for the constructive validation of the EISL.30
Comparing our results to those previously obtained from EISL-P1 in São Paulo, it could be noticed that infections were detected as risk factors in both phases. The significant association between infections and RW is evident. Together with atopy, it may constitute the bases of the progression from wheezing in infants to adulthood asthma.3
Several authors and studies have pointed out RW as a pre-asthma condition,3,28 suggesting that the precocious detection of RW is crucial. In this study, factors significantly associated with RW were frequent URI, positive medical history of pneumonia and family history of asthma. The knowledge of these risk factors is tailored to identify the possible asthmatic among infants, improving the prevention and treatment strategies for these patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Funding sourceNone.
Conflict of interestNone.