Ischemic hepatitis is an infrequent entity, usually associated with low cardiac out put. We present a case of a 57 year-old man with chronic renal failure and cardiac tamponade who developed elevation of serum alanine transferase level of 5,054 U/L, aspartate transferase level of 8,747 U/L and lactate dehydrogenasa level of 15,220 U/L. The patient developed hepatic encephalopathy and hypoglycemia. Liver Doppler ultrasound was normal. He was seronegative for HBV and HCV, drugs list was scrutinized for the names of known hepatotoxins. Ischemic hepatitis was diagnosed. The hypoglycemia and encephalopathy were solved and the patient was discharged with normal transaminase levels. Ischemic hepatitis is typically preceded by hypotension, hypoxemia, or both. As one would expect, the most common cause of sustained systemic hypotension is cardiovascular disease. Liver biopsy is usually not necessary. The best treatment is support measures and correct the underlying condition.
Ischemic hepatitis is an infrequent entity, usually associated with low cardiac out put. It is associated with high risk of death, nevertheless, it presents a favorable evolution once corrected the flow blood. The abnormalities in the levels of the liver enzymes traduce liver damage of necrosis and cholestasis.
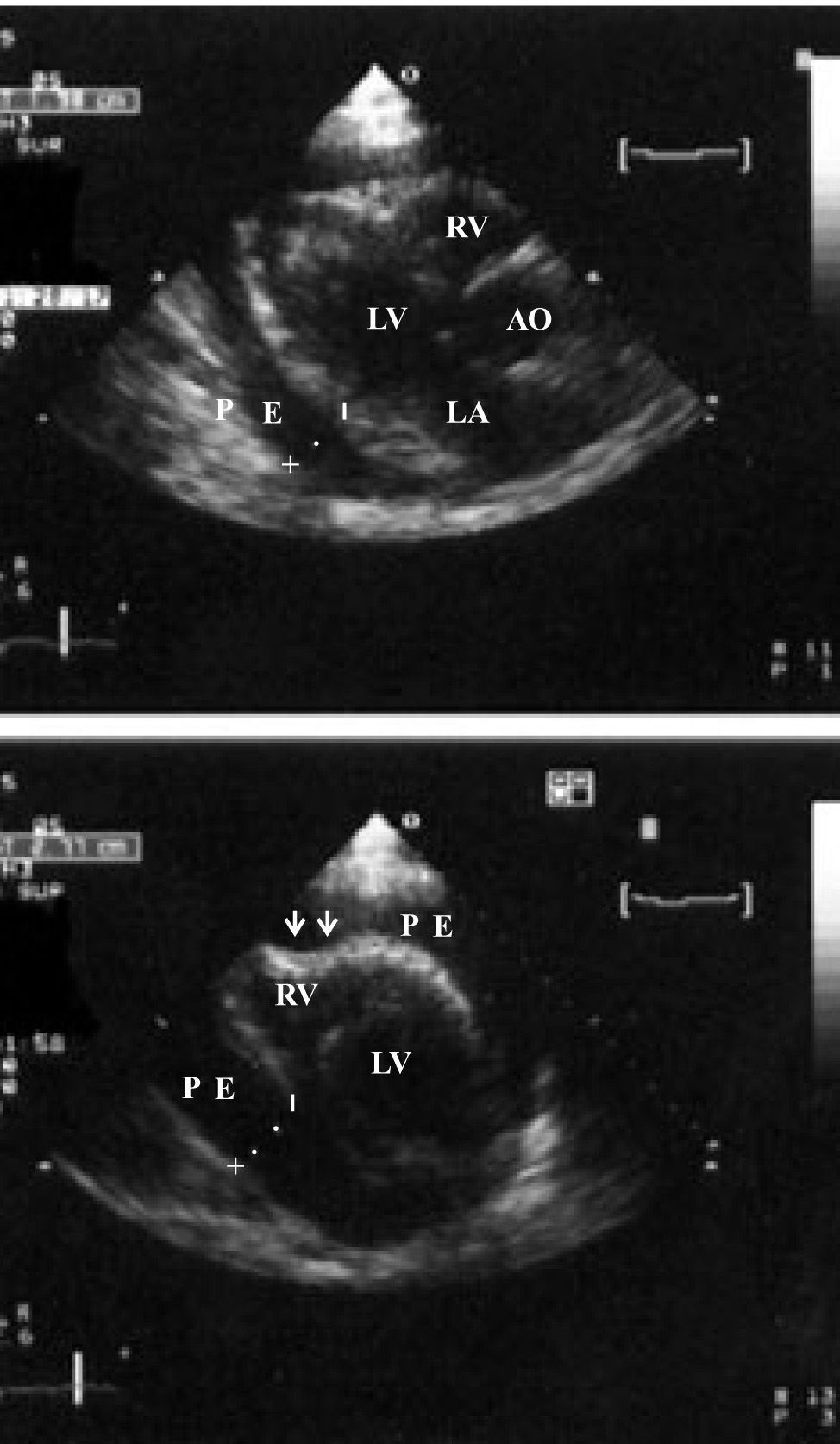
Clinical manifestationsA 57 year-old man presented at the emergency room for evaluation of dyspnea. He had type II diabetes mellitus from 15 years ago, and developed chronic renal failure as a complication. The patient had initiated hemodialysis one month before this clinical presentation. His medical record reported fatigue, exercise intolerance and dyspnea from two months. In the last 24 h the dyspnea increased. He got to the hospital with hemodynamic unstable condition, tachycardia, systolic blood pressure was 60 mmHg, the heart sounds were distant, there was moderated peripheral edema in lower limbs, he was conscious and oriented. A chest X ray (Figure 1) showed a wide heart silhouette, paradoxus pulse was documented. The ECG revealed tachycardia with low voltage (Figure 2). The echocardiography confirmed the diagnosis of pericardial effusion of 600 mL and right atrial-ventricular diastolic collapse (Figure 3). The serum creatinine was 8.2 mg/dL and the blood urea nitrogen was 59.7 mg/dL. The diagnosis of cardiac tamponade was established.
EvolutionHe required inotropic support with norepinefrine and aggressive administration of IV saline to maintain adequate ventricular filling. An urgent pericardiocentesis was performed under echocardiography guidance and blood fluid was drained. After the pericardiocentesis the patient improved, the inotropic support was no more necessary, the hemodialysis session was performed without complications but the rutinary exams at the next day showed high necroinflammatory activity of the liver with alanine transferase levels of 5,054 U/L, aspartate transferase levels 8,747 U/L, lactate dehydrogenasa levels 15,220 U/L, prothrombin time 16 seconds, INR 2.4, total bilirrubin 1.44 mg/dL, alkaline phosphatasa 188 U/L. Liver Doppler ultrasound was normal. He was seronegative for HBV and HCV, drugs list was scrutinized for the names of known hepatotoxins. At this time the patient developed hepatic encephalopathy with asterixis, aggressive behavior, arterial ammonium levels reported 98 μg/dL. (normal range 19-69). Antiammonium measures were initiated with parenteral L-ornitine and L-aspartate. Because hemorrhagic pericardial fluid was drained and the prothrombin time was prolonged, fresh frozen plasma was indicated. In the next 24 h transaminase levels decreased 50%: ALT 5,757 U/L, AST 4,423 U/L, DHL 7,906 U/L. INR 1.7. Hypoglycemia (50 mg/dL) was corrected with glucose infusion. The hypoglycemia and encephalopathy were solved, the ammonium levels decreased to 57 μg/dL. Liver biopsy was not performed and ischemic hepatitis was diagnosed. The patient was discharged with normal transaminase levels. A second echocardiography showed no pericardial effusion.
DiscussionIschemic hepatitis is typically preceded by hypotension, hypoxemia, or both. As one would expect, the most common cause of sustained systemic hypotension is cardiovascular disease, as in the present case, a patient with cardiac tamponade. Johnson and cols.1 showed in 23,125 admissions that 56 patients developed serum AST concentrations greater than 3,000 U/L, an occurrence rate of approximately two per 1,000 admissions. Acute hypotension (ischemic or hypoxic hepatitis) accounted for the majority (29/56) of the cases; which means that extreme elevations of AST are most often attributable to hypoxic hepatitis. Hypotension is most frequently caused by acute myocardial infarction or cardiac surgery and sepsis is the next leading cause. Other studies have shown that ischemic hepatitis can be detected biochemical in 0.3% to 2.6% of all patients admitted to a hospital for cardiac events.
In another recently series Bruguera2 investigate the frequency of distinct causes of elevated transaminase levels in the range of acute viral hepatitis in patients attended in a hospital. The major cause in 84 patients was hepatic ischemia in 24 (28%). In transplant recipients, the most frequent causes were ischemia/reperfusion injury, while in non-transplanted patients the most frequent causes were ischemic hepatitis and acute episodes of chronic viral hepatitis. The AST/ALT ratio did not contribute to etiologic diagnosis.
The diagnosis of ischemic hepatitis is typically first recognized by the laboratory finding of extraordinarily high aminotransferase values on a screening panel. Most often, the patient is in the hospital for problems not primarily associated with the liver. Findings of physical examination are not revealing, although altered mental status has been described in a few patients. The lactate dehydrogenase level is profoundly elevated. The ratio of alanine aminotransferase to lactate dehydrogenase is much higher in acute viral hepatitis than it is in ischemic hepatitis. The prothrombin time may be prolonged by 2 or 3 seconds. Hypoglycemia has been report in 30%.3 In many cases, a secure diagnosis cannot be made until the characteristic normalization of liver function test results occurs within a few days. Liver biopsy, which is usually not necessary, reveals bland, centrizonal necrosis with preservation of hepatic architecture. The mechanism is massive necrosis of hepatic cells in central lobulillar area by the hypoxemia caused by the low cardiac output. Damage of the 3 zone by ischemic or toxic, result in a predominant increase of the AST because the high concentration in liver acinos.
In the most severely affected patients, ischemic hepatitis is one manifestation of multiorgan failure and has a poor prognosis. Likewise, in the few patients whose liver injury is so severe that the syndrome of fulminant hepatic failure develops, ischemic hepatitis may be lethal. Fortunately, most cases are transient and subclinical. The pathophysiology of ischemic hepatitis, otherwise known as “shock liver,” is poorly understood, although it is believed to be the result of a reduction in systemic blood flow as typically occurs in shock. Systemic hypotension or shock alone did not lead to ischemic hepatitis. The vast majority of patients with ischemic hepatitis had severe underlying cardiac disease that had often led to passive congestion of the liver as showed by Seeto and cols.4 He identified a cohort of 31 patients (case group) who met the most commonly accepted definition of ischemic hepatitis (an acute reversible elevation in either the serum alanine or aspartate aminotransferase level of at least 20 times the upper limit of normal, excluding known causes of acute hepatitis or hepatocellular injury, in an appropriate clinical setting) and also evaluated the clinical features and serum aminotransferase levels in a cohort (the control group) of 31 previously healthy patients who sustained major non-hepatic trauma. Despite the marked reduction in blood pressure, no patient in the control group developed ischemic hepatitis. All 31 patients with ischemic hepatitis had evidence of underlying organic heart disease, 29 (94%) of whom had right-sided heart failure. So the vast majority of patients with ischemic hepatitis had severe underlying cardiac disease that had often led to passive congestion of the liver. These data suggest that right-sided heart failure, with resultant hepatic venous congestion, may predispose the liver to hepatic injury induced by a hypotensive event. In the other side, there are some reports of ischemic hepatitis associate with severe arterial hypoxemia in obese patients5-7 and some authors propose change the term for hepatitis hypoxic.8 The best treatment is support measures and correct the underlying condition. There is no prognosis model but the development of fulminant failure is associate with high mortality.