Introduction and aim. The evaluation to determine the cause of hepatic encephalopathy consists primarily of laboratory testing to rule out infections and metabolic causes. Despite lack of evidence, it is a common practice amongst clinicians to obtain a head CT as part of their initial evaluation in a cirrhotic presenting with recurrent episodes of hepatic encephalopathy.
Material and methods. Medical records of all cirrhotic adults admitted to a tertiary care hospital from 2007 to 2010 with hepatic encephalopathy were reviewed.
Results. In 67 patients, there were 147 episodes of hepatic encephalopathy where a head CT was performed. Six CTs had intracranial findings explaining hepatic encephalopathy. Two patients had focal neurologic findings on physical exam with no history of trauma, one had a history of trauma with no focal neurologic deficits and two had both a history of trauma and focal neurologic findings. Only one case revealed an intracranial hemorrhage with neither a preceding history of trauma nor positive neurological signs. The overall prevalence of intracranial findings in hepatic encephalopathy was 4% (6/147) and 0.6% (1/142) in the absence of trauma or focal neurologic findings. Laboratory and clinical variables including mean levels of ammonia, sodium, creatinine, bilirubin, albumin, platelet count, INR, encephalopathy grade and MELD score did not have a statistically significant impact on head CT findings (P > .05).
Conclusion. In conclusion, the yield of a head CT in determining the cause of change in mental status is extremely low in patients with cirrhosis who present with recurrent hepatic encephalopathy.
Hepatic encephalopathy (HE) describes the spectrum of transient and potentially reversible neuropsychiatric abnormalities, seen in 50-70% of patients with chronic liver dysfunction.1 Patients present with a wide spectrum of symptoms, the most common being confusion or altered mental status. Before arriving at a diagnosis of HE, it is of utmost importance to exclude other etiologies of neuropsychiatric abnormalities in patients with chronic liver disease who present with change in mentation. These include intracranial space occupying lesions, cerebrovascular events, infections and metabolic derangements.2
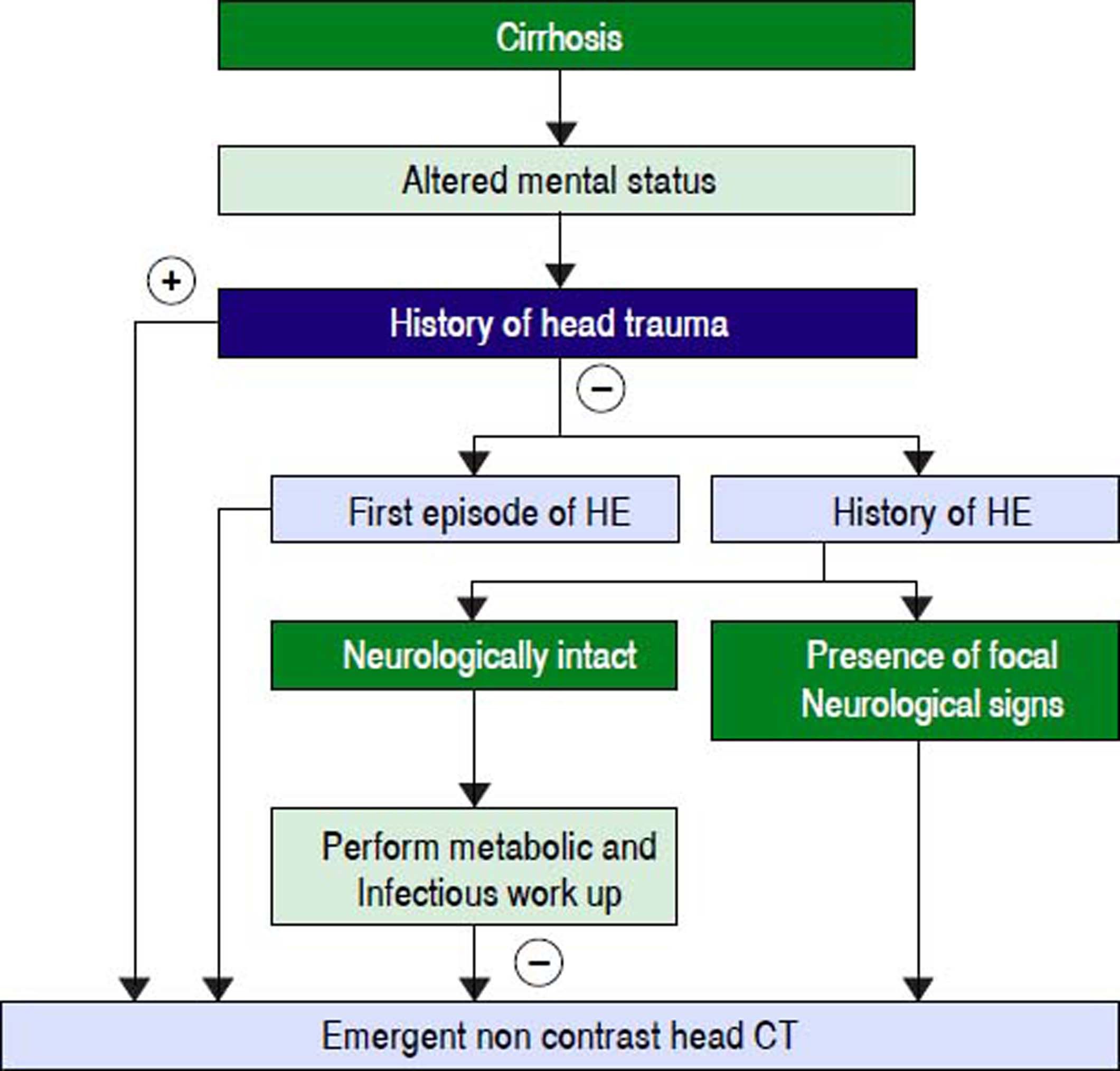
When a patient with cirrhosis presents for the first time with altered mental status a non-contrast computed tomographic (CT) scan of the head should be performed to exclude any structural abnormalities of the brain. However due to the nature of chronic liver disease, patients with cirrhosis often present with recurrent episodes of HE. Historically, it has been observed that clinicians commonly request imaging of the brain (head CT) on subsequent episodes of HE without any evidence supporting this clinical practice.
The yield of a head CT in determining the etiology of altered mental status in the general population is low in the absence of preceding history of trauma or when there is a lack of focal neurological signs on examination.3–5 However, the perceived notion of auto anticoagulation due to an elevated international normalized ratio (INR) and the presence of thrombocytopenia in patients with cirrhosis, commonly prompt the clinician to request brain imaging in order to rule out intracranial hemorrhage. It is important to revisit the usefulness of a head CT scan as the procedure is expensive, exposes the patient to radiation and delays the treatment of HE.
The aim of our study is to determine the prevalence of positive head CT findings in cirrhotic patients with an acute presentation of HE. On the basis of our findings we would like to identify scenarios in which the head CT scan would be a useful tool in assessment of cirrhotic patients with altered mental status. Lastly, we want to identify any biochemical and coagulation profiles that may correlate with abnormal brain imaging findings in this subset of patients.
Material and MethodsThis is a retrospective, observational, single-center study conducted at a tertiary care hospital (Hahnemann University Hospital, Philadelphia, Pennsylvania). Data over a three-year period (2007-2010) was analyzed, from inpatient medical records of patients with a known history of cirrhosis that presented to the emergency department with HE or had an episode of HE while an inpatient. All patients had a head CT performed as part of their initial evaluation for altered sensorium. The study protocol was approved by our institutional review board, which waived informed consent for this retrospective study.
Inclusion criteria were age older than 18 years and an established diagnosis of liver cirrhosis. Patients were excluded from the study if this was their first episode of HE, if they had a previous history of stroke, intracranial spaceoccupying lesion or had a known neurological illness such as dementia or parkinsonism.
The diagnosis of HE was made if the patient had altered mental status or compatible neuropsychological signs (i.e., somnolence, confusion, focal neurological deficit, asterixis or fetor hepaticus). CT scan of the entire head was performed at 4-mm intervals on a stat protocol using GE equipment. All CT scans were performed without contrast and sedation, and were reviewed by a radiologist.
Data for each patient were recorded for demographic characteristics, etiology of cirrhosis, history of trauma, antiplatelet/anticoagulation therapy, neurological examination findings, biochemical data (serum levels of sodium, creatinine, albumin, total bilirubin, ammonia, platelets and INR) and CT brain findings.
Data were recorded in an electronic database. Statistical analysis was performed using the SAS system, version 9.1. Categorical data was analyzed by χ2 test and Fisher’s exact test. A p value of < 0.05 was considered statistically significant.
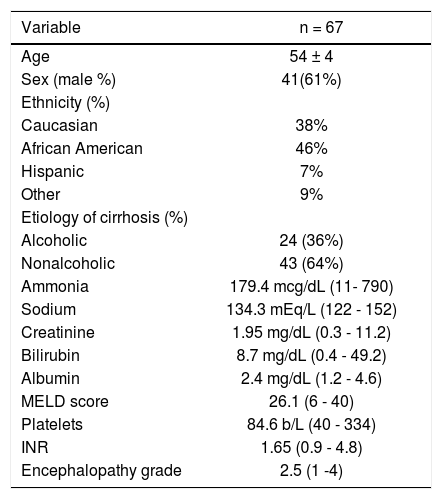
ResultsWe identified 147 episodes of HE in 67 patients who met the inclusion criteria. The baseline patient characteristics are displayed in table 1. The causes for encephalopathy included infection, gastrointestinal bleeding, medication noncompliance, dehydration, renal failure, constipation, medications, transjugular intrahepatic portosystemic shunt, and portal vein thrombosis.
Baseline patient characteristics.
| Variable | n = 67 |
|---|---|
| Age | 54 ± 4 |
| Sex (male %) | 41(61%) |
| Ethnicity (%) | |
| Caucasian | 38% |
| African American | 46% |
| Hispanic | 7% |
| Other | 9% |
| Etiology of cirrhosis (%) | |
| Alcoholic | 24 (36%) |
| Nonalcoholic | 43 (64%) |
| Ammonia | 179.4 mcg/dL (11- 790) |
| Sodium | 134.3 mEq/L (122 - 152) |
| Creatinine | 1.95 mg/dL (0.3 - 11.2) |
| Bilirubin | 8.7 mg/dL (0.4 - 49.2) |
| Albumin | 2.4 mg/dL (1.2 - 4.6) |
| MELD score | 26.1 (6 - 40) |
| Platelets | 84.6 b/L (40 - 334) |
| INR | 1.65 (0.9 - 4.8) |
| Encephalopathy grade | 2.5 (1 -4) |
The overall prevalence of intracranial findings on head CT in our patient population was 6 in 147 episodes (4%). Imaging of the brain was normal in the remaining 141 head CT performed. In the 147 episodes of HE, there were 10 episodes of HE where patients had focal neurological signs on clinical examination.
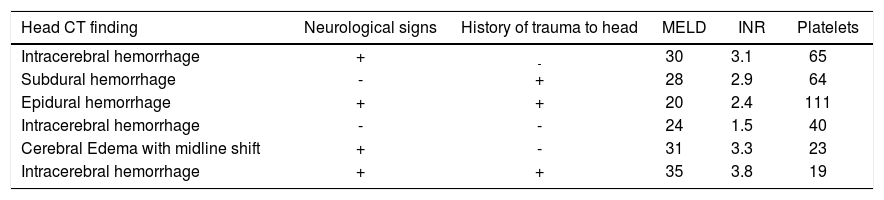
The six episodes of HE associated with positive head CT findings were the primary focus because analysis of their presentation could help triage patients who would require a more thorough workup (Table 2). Out of the six abnormal head CT scans, five patients had various forms of intracranial bleeding while one patient was reported as having diffuse cerebral edema with midline shift. Two out of the six patients presented with a recent history of trauma and had focal findings on neurological examination. Two other patients presented with focal neurological findings but no documented history of trauma. The fifth patient with an abnormal head CT scan had a subdural hemorrhage with a recent history of trauma but had a normal neurological exam. The sixth patient was diagnosed with intracranial hemorrhage but did not have a history of trauma nor presence of focal neurological findings on physical examination. Overall, 1 of 142 (0.7%) episodes of HE had acute intracranial findings on neuroimaging without the presence of trauma or a focal neurological finding on examination. None of these patients were on anti-platelet or anticoagulant agents.
Radiological and laboratory findings in patients with positive head CT.
| Head CT finding | Neurological signs | History of trauma to head | MELD | INR | Platelets |
|---|---|---|---|---|---|
| Intracerebral hemorrhage | + | - | 30 | 3.1 | 65 |
| Subdural hemorrhage | - | + | 28 | 2.9 | 64 |
| Epidural hemorrhage | + | + | 20 | 2.4 | 111 |
| Intracerebral hemorrhage | - | - | 24 | 1.5 | 40 |
| Cerebral Edema with midline shift | + | - | 31 | 3.3 | 23 |
| Intracerebral hemorrhage | + | + | 35 | 3.8 | 19 |
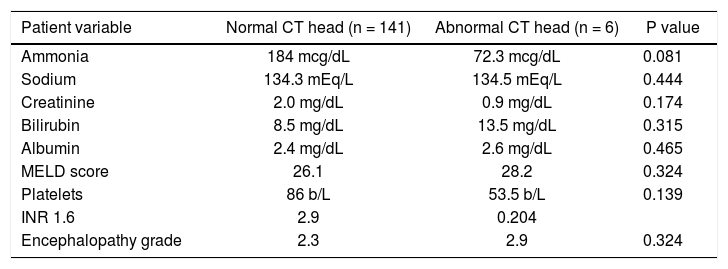
The mean levels of laboratory values from patients with HE found to have abnormal head CT, were compared to those with normal head CT to identify any clinical differences or trends in their laboratory workups (Table 3). None of these variables had a statistically significant impact on CT findings (p > 0.05).
Mean value of variables in patients with normal and abnormal CT head.
| Patient variable | Normal CT head (n = 141) | Abnormal CT head (n = 6) | P value |
|---|---|---|---|
| Ammonia | 184 mcg/dL | 72.3 mcg/dL | 0.081 |
| Sodium | 134.3 mEq/L | 134.5 mEq/L | 0.444 |
| Creatinine | 2.0 mg/dL | 0.9 mg/dL | 0.174 |
| Bilirubin | 8.5 mg/dL | 13.5 mg/dL | 0.315 |
| Albumin | 2.4 mg/dL | 2.6 mg/dL | 0.465 |
| MELD score | 26.1 | 28.2 | 0.324 |
| Platelets | 86 b/L | 53.5 b/L | 0.139 |
| INR 1.6 | 2.9 | 0.204 | |
| Encephalopathy grade | 2.3 | 2.9 | 0.324 |
The diagnosis of HE is primarily made clinically with the adjunct of laboratory and radiologic testing to exclude infectious and metabolic causes.1 Despite the scarcity of evidence, head CT scan is used frequently by clinicians to rule-out intracranial pathology in a cirrhotic patient presenting with altered mental status.
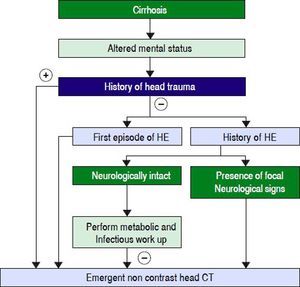
With the exception of frontal cortical atrophy and mild cerebral edema, head CT scan is often normal in patients with cirrhosis presenting with HE.6,7 These findings are usually “chronic” and have a limited value in the management of a patient during an episode of HE.8,9 We hypothesized that a head CT scan should not be part of the initial evaluation in a cirrhotic patient with a change in mental status unless there is a history of trauma or focal findings on a neurological examination. Of the 147 head CT scans studied, only 6 (4%) had positive intracranial findings. These scans were from six different patients. Five out of these six patients had either a history of preceding head trauma or had focal neurological findings on clinical examination. Imaging of the head was normal in the remaining 141 CTs performed. These findings indicate that neuroimaging of the brain has a very low yield in determining the cause of HE and should be reserved for patients who have either a history of trauma or a focal neurological deficit on clinical examination. In cases where no known precipitator is found after initial evaluation or there is a lack of clinical improvement after medical therapy, neuroimaging should be used for further evaluation (Figure 1).
Traditionally deranged hemostatic indices or extreme alteration in mental status have been used as a justification by clinicians to perform a head CT in a patient with chronic liver disease. However, we did not find any significant association between these hematological parameters, nor the grade of encephalopathy or MELD scores in patients who had positive finding on CT of the brain.
When a patient with cirrhosis presents with altered mental status and provides a history of preceding trauma, it is obligatory to obtain imaging of the head to rule out intracranial hemorrhage. The presentation of HE with focal neurological signs is well documented in the literature.10 Whether the presence of focal neurological signs is a strong enough indication to perform imaging of the head remains a matter of debate. Rahimi, et al. evaluated 223 patients with cirrhosis and altered mental status that underwent head CT scanning on admission to the hospital. HE was the cause of altered mental status in 47% of patients. They found that no patient with HE had focal neurologic findings nor a focal abnormality on head CT. Moreover, all of the patients who had abnormal brain imaging, also had coexistent focal neurologic findings on presentation.11 Contrarily, Cadranel, et al. observed 8 patients with HE who had a focal neurological deficit on clinical evaluation, but had normal head CT.12
The results of our study are reinforced by a recent study. Donovan, et al.13 demonstrated that in patients with cirrhosis (n = 462) presenting with altered mental status, those with a history of trauma, intracranial hemorrhage or positive focal neurological signs on clinical examination had a higher likelihood of intracranial hemorrhage on head CT. The yield of CT scan for altered mental status in the absence of the above factors was extremely low (0.3%). Our study was different, as we looked at patients with a known history of HE who presented with recurrent episodes of HE. Moreover our study focused not only on intracranial hemorrhage but a broader range of intracranial findings on head CT.
Our study is not without limitations. First, it was conducted on a preselected, nonrandomized cohort at a single center. Secondarily, one of the six patients with intracranial hemorrhage on neuroimaging did not have a history of trauma nor a focal neurological deficit on examination. Although this patient represents only 0.6% of the study population, missing his diagnosis would have been catastrophic. We therefore recommend a prospective, multicenter, randomized controlled study to assess the utility of neuroimaging to find correlating significant findings as a cause for HE.
In conclusion, the yield of a head CT scan in determining the etiology of change in mental status is extremely low in patients with liver cirrhosis who present with recurrent HE. The diagnostic evaluation to determine the precipitating cause of HE should include a thorough history, detailed neurological examination, and supportive laboratory test to evaluate for infections, gastrointestinal bleeding, metabolic disturbances and drug intoxication. We recommend that a head CT scan should be performed in the initial evaluation of patients presenting with recurrent HE, only when there is history of trauma or evidence of focal neurological findings on clinical exam. This approach would be cost-effective, time saving, and prevent unnecessary exposure to radiation.
Abbreviations- •
CT: computed tomography.
- •
HE: hepatic encephalopathy.
- •
INR: international normalized ratio.
- •
MELD: model for end stage liver disease.
None.
DisclosuresNone of the authors have any conflicts of interest to disclose