Drug-induced liver injury (DILI) is rare; however, it is one of the important causes of acute liver failure which results in significant morbidity or mortality.
Material and MethodsPatients with suspected DILI were enrolled based on predefined criteria and followed up for at least 6 months or until normalization of liver tests. Causality assessment was done by applying the Roussel Uclaf Causality Assessment Method model.
ResultsWe collected data from 82 individuals diagnosed with DILI at our hospital from 2014 through 2015 (41 men; median age, 38 years). The most commonly implicated drugs were antitubercular therapy (ATT) (49%), antiepileptic drugs (12%), complementary and alternative medicine (CAM) in 10%, antiretroviral drugs (9%) and non-steroidal anti-inflammatory drugs (6%). 8 out of 13 deaths were liver related. Also, liver related mortality was significantly higher for ATT DILI (17.5%) vs. those without (2.4%) (P = 0.02). There was no significant difference in overall as well as liver related mortality in hepatocellular, cholestatic or mixed pattern of injury. Laboratory parameters at one week after discontinuation of drug predicted mortality better than those at the time of DILI recognition. On multivariate logistic regression analysis, jaundice, encephalopathy, MELD (Model for end stage liver disease) score and alkaline phosphatase at one week, independently predicted mortality.
ConclusionDILI results in significant overall mortality (15.85%). ATT, anti-epileptic drugs, CAM and antiretroviral drugs are leading causes of DILI in India. Presence of jaundice, encephalopathy, MELD score and alkaline phosphatase at one week are independent predictors of mortality.
Drug-induced liver injury (DILI) is an uncommon cause of liver disease in the general population.1 DILI in most cases is detected with mild to moderate elevations of liver tests. However, in rare cases it may lead to liver failure and mortality.2 Also, hepatotoxicity is one of the important causes of termination of clinical trials and withdrawal of drug after marketing.3 The real incidence of DILI remains unknown due to difficulty in establishing diagnosis and the subclinical nature of injury in many cases. Its annual incidence in general population ranges from 14 to 19 per 100,000 inhabitants, with approximately 30% exhibiting jaundice.1,4 Overall mortality from 10 to 17.3% has been observed in several series.2,5-7
The major etiologic agents for DILI include antibiotics, anti-epileptics, complementary and alternative medicine (CAM) and non-steroidal anti-inflammatory drugs (NSAIDS).2,5 However, there is limited data from developing countries including Indian subcontinent, on etiology and outcome of DILI. As tuberculosis remains a very common infectious disease in these regions, most commonly implicated drugs for DILI are anti-tuberculous therapy (ATT).5
The spectrum of clinical presentation of DILI is wide, from asymptomatic liver test abnormalities to symptomatic acute liver disease or liver failure. This study was conducted to evaluate various causes, clinical features and outcomes of DILI in India. Also, the clinical and laboratory parameters associated with mortality were studied.
Material and MethodsThe study was designed as a single centre prospective observational cohort study. It was conducted in the Department of Gastroenterology in a large tertiary care hospital of a metropolitan city in western India. Patients were enrolled during the study period of two years from January 2014 to December 2015. Inpatients as well as outpatients presenting by themselves and satisfying the study criteria were included. Informed consent was taken from all the patients. The criteria for DILI were those established by the Indian Network for DILI (INDILI) in 2012. DILI was defined as (a) aspartate aminotransferase (AST) or alanine aminotransferase (ALT) levels greater than 5 times the upper limit of normal (ULN), regardless of symptoms or (b) total bilirubin greater than 2 mg/dL and rise in AST or ALT or alkaline phosphatase (ALP) levels greater than 2 times the ULN or (c) AST or ALT greater than 3 times ULN, if symptomatic with nausea, vomiting, abdominal pain, anorexia, skin rash, etc. Exclusion of other competing causes such as viral hepatitis, bile duct obstruction or congestive heart failure was done with serological tests and imaging.
Clinical and laboratory details of the patients were recorded as per the INDILI proforma. Clinical variables included age, gender, symptoms, duration of hospitaliza-tion and drug intake, concomitant drugs and illness, and cause of death. Laboratory tests included liver function tests, serum creatinine, complete hemogram, international normalized ratio, and viral serology to exclude viral hepatitis (IgM anti-hepatitis A virus, IgM anti-hepatitis E virus, hepatitis B surface antigen, IgM anti-hepatitis B core antigen, anti-hepatitis C virus antibody, Human Immunodeficiency Virus ELISA). If clinically indicated, studies were undertaken to exclude malaria, enteric fever, leptospirosis, dengue, and Wilson's disease. Tests for autoimmune hepatitis like anti-nuclear antibodies and smooth muscle antibodies or anti-LKM1 antibody were done if indicated. Acute kidney injury was defined as per the Kidney Disease Improving Global Outcomes (KDIGO) criteria.9 Abdominal ultrasound was done to rule out biliary obstruction. All patients were followed up for at least 6 months or until normalization of liver biochemistry. Injury was considered as chronic if serum biochemistry values or imaging remained abnormal at 6 months.2 Patients with pre-existing chronic liver injury were not excluded if they were considered to have developed superimposed DILI. If their basal liver tests were abnormal the DILI-induced increase was based on that basal value and the ULN was calculated from that value.1 MELD score was calculated by the formula: 9.6 x loge (creatinine mg/dL) + 3.8 x loge (bilirubin mg/dL) + 11.2 x loge (international normalized ratio) + 6.4.
Causality assessmentThe levels of liver tests immediately on admission or outpatient visit were used for analysis. Causality assessment will be done by applying the Roussel Uclaf Causality Assessment Method (RUCAM) model.10,11 According to these criteria, the liver injury was classified into hepato-cellular, cholestatic, or mixed pattern and the causal relationship was classified as highly probable, probable, possible, unlikely, or excluded. Only cases of confirmed DILI (i.e., highly probable, probable, or possible) were included in this report.
Assessment of clinical patterns of liver injuryAssessing the pattern of liver injury as hepatocellular, cholestatic, or mixed is based on calculating the “R” ratio, defined by the ratio of serum ALT to ALP, both expressed as multiples of the ULN. The R ratio applied to each case was calculated based on the initial liver tests at presentation. The cases were classified as hepatocellular if the R ratio was greater than 5, as cholestatic if the ratio was less than 2, and as mixed if the ratio was 2-5.10,11
Severity assessmentClinical severity of DILI was classified using DILI severity index adopted by the consensus criteria in 2011.12DILI severity was classified as mild, moderate, severe and fatal accordingly.
Statistical analysisFor processing the data, Microsoft Office Excel 2010 (Microsoft, Redmond, WA) and IBM SPSS Statistics Version 22.0 (IBM, Armonk, NY) were used. Data is summarized as means and standard deviation (SD) for continuous variables and frequencies and percentages for categorical variables. Categorical variables were analyzed using the χ2 test or Fisher's exact test when a cell's expected number was fewer than five. Continuous variables were analyzed using Mann-Whitney test for non-parametric data and unpaired t test for parametric data. Analysis of variance (ANOVA) was used for comparisons of groups. Multivariate analysis by logistic regression was performed to identify independent predictors of mortality, using all variables found to be clinically significant on univariate analysis. All reported P values are 2-tailed. The level of significance was set at 0.05.
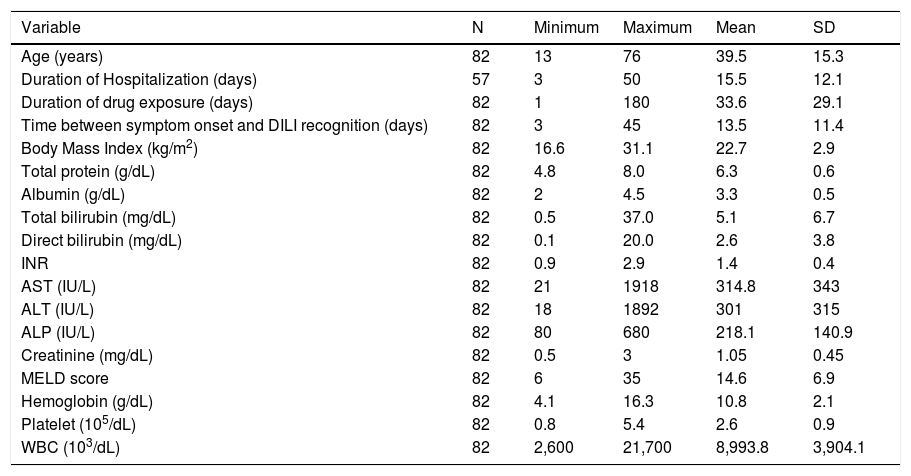
ResultsDemographic and clinical characteristicsDuring the 2 year study period, a total of 82 patients, including 41 (50%) women, mean age of 39.5 years (standard deviation [SD], 15.3 years), fulfilled the criteria for inclusion in the study. The youngest patient was 13 years old and the oldest patient was 76 years old. Most common symptoms were nausea (91%), vomiting (85%), abdominal pain (73%) and anorexia (69%). Jaundice and dark colored urine was presenting feature in 55% and 58%, respectively. The median duration of drug exposure was 28 days (range, 1-180 days). 57 patients were hospitalized (69%) for a median of 10 days (range, 3-50 days). 4 patients (5%) had underlying liver disease in the form of alcoholic liver disease, nonalcoholic steatohepatitis, chronic hepatitis B and C (1 each). Two patients had diabetes with dyslipidemia. Summary of the clinical and laboratory variables is shown in Table 1.
Summary of demographic and laboratory variables in patients with DILI (n = 82).
| Variable | N | Minimum | Maximum | Mean | SD |
|---|---|---|---|---|---|
| Age (years) | 82 | 13 | 76 | 39.5 | 15.3 |
| Duration of Hospitalization (days) | 57 | 3 | 50 | 15.5 | 12.1 |
| Duration of drug exposure (days) | 82 | 1 | 180 | 33.6 | 29.1 |
| Time between symptom onset and DILI recognition (days) | 82 | 3 | 45 | 13.5 | 11.4 |
| Body Mass Index (kg/m2) | 82 | 16.6 | 31.1 | 22.7 | 2.9 |
| Total protein (g/dL) | 82 | 4.8 | 8.0 | 6.3 | 0.6 |
| Albumin (g/dL) | 82 | 2 | 4.5 | 3.3 | 0.5 |
| Total bilirubin (mg/dL) | 82 | 0.5 | 37.0 | 5.1 | 6.7 |
| Direct bilirubin (mg/dL) | 82 | 0.1 | 20.0 | 2.6 | 3.8 |
| INR | 82 | 0.9 | 2.9 | 1.4 | 0.4 |
| AST (IU/L) | 82 | 21 | 1918 | 314.8 | 343 |
| ALT (IU/L) | 82 | 18 | 1892 | 301 | 315 |
| ALP (IU/L) | 82 | 80 | 680 | 218.1 | 140.9 |
| Creatinine (mg/dL) | 82 | 0.5 | 3 | 1.05 | 0.45 |
| MELD score | 82 | 6 | 35 | 14.6 | 6.9 |
| Hemoglobin (g/dL) | 82 | 4.1 | 16.3 | 10.8 | 2.1 |
| Platelet (105/dL) | 82 | 0.8 | 5.4 | 2.6 | 0.9 |
| WBC (103/dL) | 82 | 2,600 | 21,700 | 8,993.8 | 3,904.1 |
ALP: Alkaline phosphatase. AST: Aspartate transaminase. ALT: Alanine transaminase. DILI: Drug induced liver injury. INR: International normalized ratio. MELD: Model for End stage Liver Disease. WBC: White blood cell count. SD: Standard deviation.
By using the RUCAM model for drug causality assess-ment,10,11 4 patients (5%) were classified as possible, 63 as probable (77%) and 15 as highly probable (18%). Out of 90 patients enrolled in the study initially, in 8 patients DILI was deemed unlikely to be responsible for liver injury; the final diagnoses in these patients were acute hepatitis E in 3 patients, autoimmune hepatitis in 2 patients, hepatitis A, B and sarcoidosis in 1 patient each.
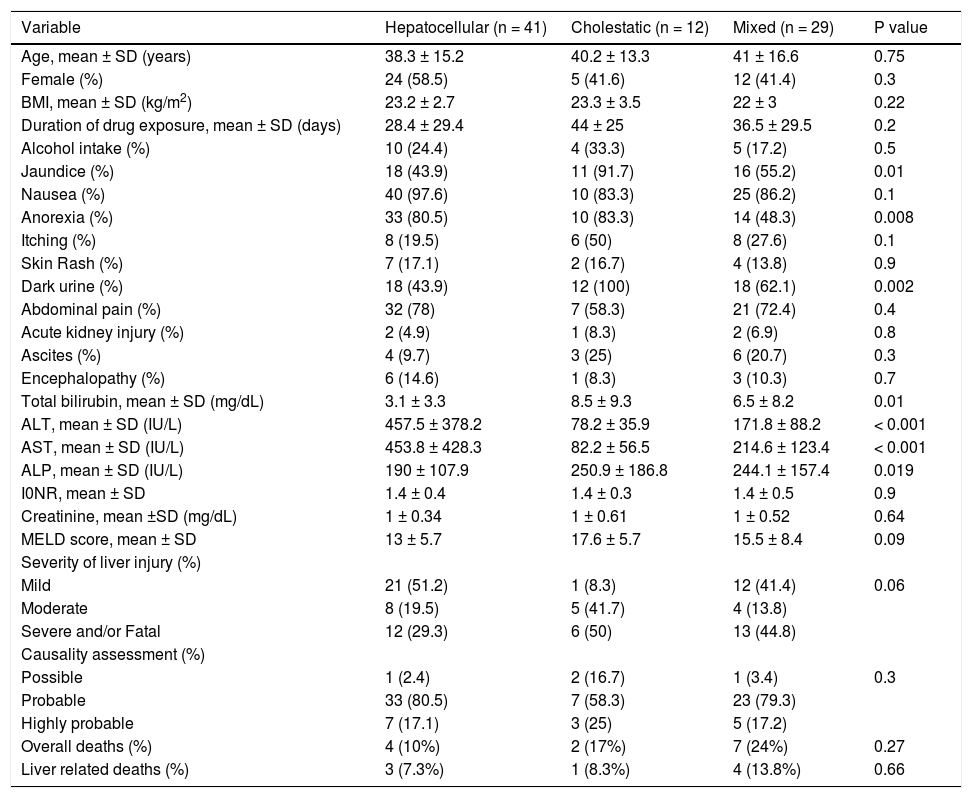
Patterns of DILIThe R value was calculated as per the lab values on the day of DILI recognition. A total of 41 patients (50%) were classified as hepatocellular, 12 (15%) as cholestatic and 29 (35%) as mixed. The clinical and laboratory features of patients with the 3 patterns of DILI are shown in Table 2. Jaundice, anorexia, dark colored urine and high bilirubin were significantly more common in patients with choles-tatic liver disease in comparison to hepatocellular and mixed liver injury (P value 0.01, 0.008, 0.002 and 0.01, respectively). Also, the patients with cholestatic liver injury had higher proportion of moderate to severe injury as compared to hepatocellular or mixed type (P value 0.06). However, there was no significant difference in overall as well as liver related mortality in these groups.
Characteristics of patients with different patterns of liver injury.
| Variable | Hepatocellular (n = 41) | Cholestatic (n = 12) | Mixed (n = 29) | P value |
|---|---|---|---|---|
| Age, mean ± SD (years) | 38.3 ± 15.2 | 40.2 ± 13.3 | 41 ± 16.6 | 0.75 |
| Female (%) | 24 (58.5) | 5 (41.6) | 12 (41.4) | 0.3 |
| BMI, mean ± SD (kg/m2) | 23.2 ± 2.7 | 23.3 ± 3.5 | 22 ± 3 | 0.22 |
| Duration of drug exposure, mean ± SD (days) | 28.4 ± 29.4 | 44 ± 25 | 36.5 ± 29.5 | 0.2 |
| Alcohol intake (%) | 10 (24.4) | 4 (33.3) | 5 (17.2) | 0.5 |
| Jaundice (%) | 18 (43.9) | 11 (91.7) | 16 (55.2) | 0.01 |
| Nausea (%) | 40 (97.6) | 10 (83.3) | 25 (86.2) | 0.1 |
| Anorexia (%) | 33 (80.5) | 10 (83.3) | 14 (48.3) | 0.008 |
| Itching (%) | 8 (19.5) | 6 (50) | 8 (27.6) | 0.1 |
| Skin Rash (%) | 7 (17.1) | 2 (16.7) | 4 (13.8) | 0.9 |
| Dark urine (%) | 18 (43.9) | 12 (100) | 18 (62.1) | 0.002 |
| Abdominal pain (%) | 32 (78) | 7 (58.3) | 21 (72.4) | 0.4 |
| Acute kidney injury (%) | 2 (4.9) | 1 (8.3) | 2 (6.9) | 0.8 |
| Ascites (%) | 4 (9.7) | 3 (25) | 6 (20.7) | 0.3 |
| Encephalopathy (%) | 6 (14.6) | 1 (8.3) | 3 (10.3) | 0.7 |
| Total bilirubin, mean ± SD (mg/dL) | 3.1 ± 3.3 | 8.5 ± 9.3 | 6.5 ± 8.2 | 0.01 |
| ALT, mean ± SD (IU/L) | 457.5 ± 378.2 | 78.2 ± 35.9 | 171.8 ± 88.2 | < 0.001 |
| AST, mean ± SD (IU/L) | 453.8 ± 428.3 | 82.2 ± 56.5 | 214.6 ± 123.4 | < 0.001 |
| ALP, mean ± SD (IU/L) | 190 ± 107.9 | 250.9 ± 186.8 | 244.1 ± 157.4 | 0.019 |
| I0NR, mean ± SD | 1.4 ± 0.4 | 1.4 ± 0.3 | 1.4 ± 0.5 | 0.9 |
| Creatinine, mean ±SD (mg/dL) | 1 ± 0.34 | 1 ± 0.61 | 1 ± 0.52 | 0.64 |
| MELD score, mean ± SD | 13 ± 5.7 | 17.6 ± 5.7 | 15.5 ± 8.4 | 0.09 |
| Severity of liver injury (%) | ||||
| Mild | 21 (51.2) | 1 (8.3) | 12 (41.4) | 0.06 |
| Moderate | 8 (19.5) | 5 (41.7) | 4 (13.8) | |
| Severe and/or Fatal | 12 (29.3) | 6 (50) | 13 (44.8) | |
| Causality assessment (%) | ||||
| Possible | 1 (2.4) | 2 (16.7) | 1 (3.4) | 0.3 |
| Probable | 33 (80.5) | 7 (58.3) | 23 (79.3) | |
| Highly probable | 7 (17.1) | 3 (25) | 5 (17.2) | |
| Overall deaths (%) | 4 (10%) | 2 (17%) | 7 (24%) | 0.27 |
| Liver related deaths (%) | 3 (7.3%) | 1 (8.3%) | 4 (13.8%) | 0.66 |
ALP: Alkaline phosphatase. AST: Aspartate transaminase. ALT: Alanine transaminase. BMI: Body mass index. INR: International Normalized Ratio. MELD: Model for End Stage Liver Disease. SD: Standard deviation. P values compare hepatocellular, cholestatic and mixed categories.
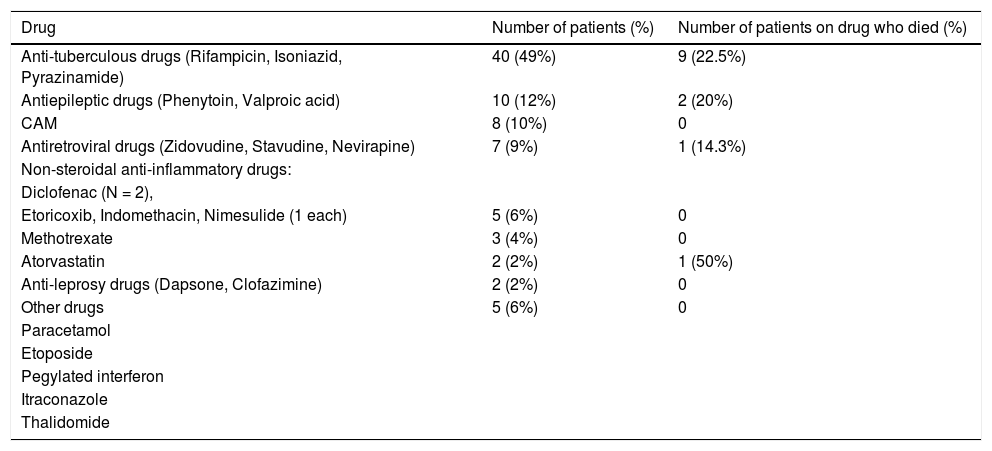
DILI was caused by a single prescription medication in 29%, by complementary and alternative medicine (CAM) in 10%, and by multiple prescription agents in 61% of cases. The most commonly implicated drugs were antitubercu-lar therapy (ATT) (40 of 82; 49%), antiepileptic drugs (12%), antiretroviral drugs (9%), non-steroidal antiinflammatory drugs (6%), methotrexate (4%), atorvastatin (2%), anti-leprosy drugs (2%) and other drugs like paracetamol, etoposide, interferon, itraconazole and thalidomide (6%) (Table 3). Two patients developed chronic DILI due to ATT and pegylated interferon, respectively. One patient of chronic hepatitis C developed pegylated interferon triggered autoimmune hepatitis and another patient had ATT induced immune mediated DILI. Both of these patients responded to oral corticosteroid therapy.
Frequency of drugs causing DILI.
| Drug | Number of patients (%) | Number of patients on drug who died (%) |
|---|---|---|
| Anti-tuberculous drugs (Rifampicin, Isoniazid, Pyrazinamide) | 40 (49%) | 9 (22.5%) |
| Antiepileptic drugs (Phenytoin, Valproic acid) | 10 (12%) | 2 (20%) |
| CAM | 8 (10%) | 0 |
| Antiretroviral drugs (Zidovudine, Stavudine, Nevirapine) | 7 (9%) | 1 (14.3%) |
| Non-steroidal anti-inflammatory drugs: | ||
| Diclofenac (N = 2), | ||
| Etoricoxib, Indomethacin, Nimesulide (1 each) | 5 (6%) | 0 |
| Methotrexate | 3 (4%) | 0 |
| Atorvastatin | 2 (2%) | 1 (50%) |
| Anti-leprosy drugs (Dapsone, Clofazimine) | 2 (2%) | 0 |
| Other drugs | 5 (6%) | 0 |
| Paracetamol | ||
| Etoposide | ||
| Pegylated interferon | ||
| Itraconazole | ||
| Thalidomide |
CAM: complementary and alternative medicine.
Out of 40 patients with ATT DILI, 24 (60%) received ATT empirically, 30 out of 40 (75%) received ATT for extra pulmonary tuberculosis. Also, liver related mortality was significantly higher for ATT DILI (17.5%) vs. those without (2.4%) (P value 0.02). However, the difference in overall mortality between the two groups was statistically non-significant (P value 0.137).
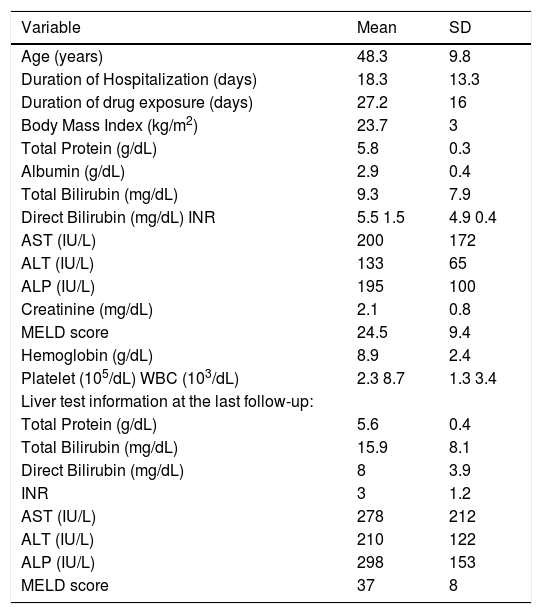
Outcomes and predictors of mortalityOverall mortality was 15.85%. Eight out of 13 patients who died, the cause of death was liver associated. Due to financial constraints and unavailability of transplantation facility at our institution, none of the patients underwent liver transplant. The cause of death in remaining 5 patients was cerebrovascular episode, respiratory failure due to organophosphorous poisoning, acute myocardial infarction, acute leukemia and tubercular meningitis (1 patient each). The mean duration of time from recognition of DILI to death was 14 days with a standard deviation of 6 days (median, 12 days; range 8-28 days).
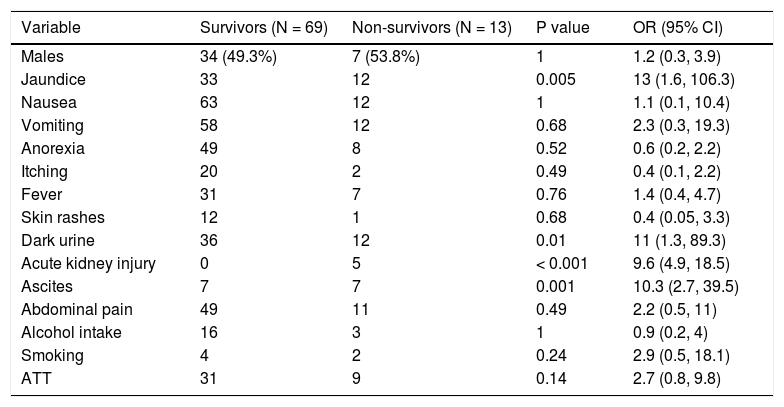
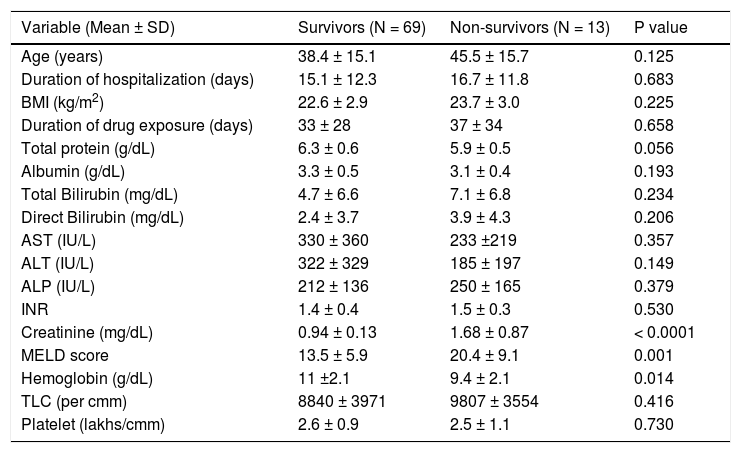
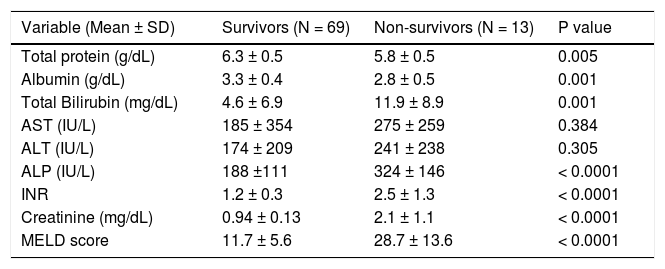
The comparison of clinical features between survivors and non-survivors is shown in Table 4. Jaundice, dark colored urine, encephalopathy, acute kidney injury and as-cites were significantly associated with higher mortality in patients with DILI. Although, high serum creatinine and MELD score along with low hemoglobin on the day of recognition of DILI, were associated with higher mortality, other laboratory parameters did not show significant difference between those who survived and those who did not (Table 5). However, majority of the laboratory parameters after one week of stopping the implicated drug showed a significant difference between survivors and non-survivors. These included a low total protein and albumin, high total and direct bilirubin, alkaline phos-phatase, international normalized ratio, creatinine and MELD score (Table 6). The details of liver related death cases are presented in table 7.
Clinical variables for survivors and non-survivors (overall mortality).
| Variable | Survivors (N = 69) | Non-survivors (N = 13) | P value | OR (95% CI) |
|---|---|---|---|---|
| Males | 34 (49.3%) | 7 (53.8%) | 1 | 1.2 (0.3, 3.9) |
| Jaundice | 33 | 12 | 0.005 | 13 (1.6, 106.3) |
| Nausea | 63 | 12 | 1 | 1.1 (0.1, 10.4) |
| Vomiting | 58 | 12 | 0.68 | 2.3 (0.3, 19.3) |
| Anorexia | 49 | 8 | 0.52 | 0.6 (0.2, 2.2) |
| Itching | 20 | 2 | 0.49 | 0.4 (0.1, 2.2) |
| Fever | 31 | 7 | 0.76 | 1.4 (0.4, 4.7) |
| Skin rashes | 12 | 1 | 0.68 | 0.4 (0.05, 3.3) |
| Dark urine | 36 | 12 | 0.01 | 11 (1.3, 89.3) |
| Acute kidney injury | 0 | 5 | < 0.001 | 9.6 (4.9, 18.5) |
| Ascites | 7 | 7 | 0.001 | 10.3 (2.7, 39.5) |
| Abdominal pain | 49 | 11 | 0.49 | 2.2 (0.5, 11) |
| Alcohol intake | 16 | 3 | 1 | 0.9 (0.2, 4) |
| Smoking | 4 | 2 | 0.24 | 2.9 (0.5, 18.1) |
| ATT | 31 | 9 | 0.14 | 2.7 (0.8, 9.8) |
ATT: Antitubercular therapy. CI: Confidence interval. OR: Odds ratio.
Demographic and laboratory variables for survivors and non-survivors (overall mortality).
| Variable (Mean ± SD) | Survivors (N = 69) | Non-survivors (N = 13) | P value |
|---|---|---|---|
| Age (years) | 38.4 ± 15.1 | 45.5 ± 15.7 | 0.125 |
| Duration of hospitalization (days) | 15.1 ± 12.3 | 16.7 ± 11.8 | 0.683 |
| BMI (kg/m2) | 22.6 ± 2.9 | 23.7 ± 3.0 | 0.225 |
| Duration of drug exposure (days) | 33 ± 28 | 37 ± 34 | 0.658 |
| Total protein (g/dL) | 6.3 ± 0.6 | 5.9 ± 0.5 | 0.056 |
| Albumin (g/dL) | 3.3 ± 0.5 | 3.1 ± 0.4 | 0.193 |
| Total Bilirubin (mg/dL) | 4.7 ± 6.6 | 7.1 ± 6.8 | 0.234 |
| Direct Bilirubin (mg/dL) | 2.4 ± 3.7 | 3.9 ± 4.3 | 0.206 |
| AST (IU/L) | 330 ± 360 | 233 ±219 | 0.357 |
| ALT (IU/L) | 322 ± 329 | 185 ± 197 | 0.149 |
| ALP (IU/L) | 212 ± 136 | 250 ± 165 | 0.379 |
| INR | 1.4 ± 0.4 | 1.5 ± 0.3 | 0.530 |
| Creatinine (mg/dL) | 0.94 ± 0.13 | 1.68 ± 0.87 | < 0.0001 |
| MELD score | 13.5 ± 5.9 | 20.4 ± 9.1 | 0.001 |
| Hemoglobin (g/dL) | 11 ±2.1 | 9.4 ± 2.1 | 0.014 |
| TLC (per cmm) | 8840 ± 3971 | 9807 ± 3554 | 0.416 |
| Platelet (lakhs/cmm) | 2.6 ± 0.9 | 2.5 ± 1.1 | 0.730 |
ALP: Alkaline phosphatase. AST: Aspartate transaminase. ALT: Alanine transaminase. BMI: Body Mass Index. INR: International Normalized Ratio. MELD: Model for End stage Liver Disease. SD: Standard deviation.
Laboratory variables for survivors and non-survivors at one week (overall mortality).
| Variable (Mean ± SD) | Survivors (N = 69) | Non-survivors (N = 13) | P value |
|---|---|---|---|
| Total protein (g/dL) | 6.3 ± 0.5 | 5.8 ± 0.5 | 0.005 |
| Albumin (g/dL) | 3.3 ± 0.4 | 2.8 ± 0.5 | 0.001 |
| Total Bilirubin (mg/dL) | 4.6 ± 6.9 | 11.9 ± 8.9 | 0.001 |
| AST (IU/L) | 185 ± 354 | 275 ± 259 | 0.384 |
| ALT (IU/L) | 174 ± 209 | 241 ± 238 | 0.305 |
| ALP (IU/L) | 188 ±111 | 324 ± 146 | < 0.0001 |
| INR | 1.2 ± 0.3 | 2.5 ± 1.3 | < 0.0001 |
| Creatinine (mg/dL) | 0.94 ± 0.13 | 2.1 ± 1.1 | < 0.0001 |
| MELD score | 11.7 ± 5.6 | 28.7 ± 13.6 | < 0.0001 |
ALP: Alkaline phosphatase. AST: Aspartate transaminase. ALT: Alanine transaminase. BMI: Body Mass Index. INR: International Normalized Ratio. MELD: Model for End Sliver Disease. SD: Standard deviation.
The details of liver related death cases (n = 8).
| Variable | Mean | SD |
|---|---|---|
| Age (years) | 48.3 | 9.8 |
| Duration of Hospitalization (days) | 18.3 | 13.3 |
| Duration of drug exposure (days) | 27.2 | 16 |
| Body Mass Index (kg/m2) | 23.7 | 3 |
| Total Protein (g/dL) | 5.8 | 0.3 |
| Albumin (g/dL) | 2.9 | 0.4 |
| Total Bilirubin (mg/dL) | 9.3 | 7.9 |
| Direct Bilirubin (mg/dL) INR | 5.5 1.5 | 4.9 0.4 |
| AST (IU/L) | 200 | 172 |
| ALT (IU/L) | 133 | 65 |
| ALP (IU/L) | 195 | 100 |
| Creatinine (mg/dL) | 2.1 | 0.8 |
| MELD score | 24.5 | 9.4 |
| Hemoglobin (g/dL) | 8.9 | 2.4 |
| Platelet (105/dL) WBC (103/dL) | 2.3 8.7 | 1.3 3.4 |
| Liver test information at the last follow-up: | ||
| Total Protein (g/dL) | 5.6 | 0.4 |
| Total Bilirubin (mg/dL) | 15.9 | 8.1 |
| Direct Bilirubin (mg/dL) | 8 | 3.9 |
| INR | 3 | 1.2 |
| AST (IU/L) | 278 | 212 |
| ALT (IU/L) | 210 | 122 |
| ALP (IU/L) | 298 | 153 |
| MELD score | 37 | 8 |
ALP: Alkaline phosphatase. AST: Aspartate transaminase. ALT: Alanine transaminase. DILI: Drug induced liver injury. INR: International Normalized Ratio. MELD: Model for End stage Liver Disease. WBC: White blood cell count.
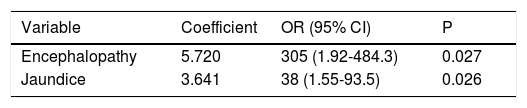
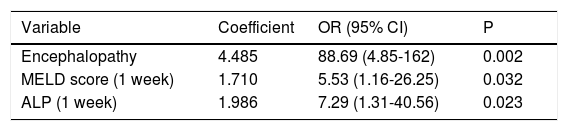
On multivariate analysis by logistic regression after adjusting for clinical and initial laboratory variables at the recognition of DILI, presence of encephalopathy (OR = 305, P = 0.027) and jaundice (OR = 38, P = 0.026) independently predicted mortality (Table 8). However, after adjusting for clinical and laboratory variables at one week, encephalopathy (OR = 88.69, P = 0.002), MELD score at one week (OR = 5.53, P = 0.032) and alkaline phos-phatase at one week (OR = 7.29, P = 0.023), independently predicted mortality (Table 9).
Independent variables associated with mortality in patients with DILI after adjusting for initial laboratory variables at recognition of DILI.
| Variable | Coefficient | OR (95% CI) | P |
|---|---|---|---|
| Encephalopathy | 5.720 | 305 (1.92-484.3) | 0.027 |
| Jaundice | 3.641 | 38 (1.55-93.5) | 0.026 |
CI: Confidence interval. OR: Odds ratio. Constant = - 0.668
Independent variables associated with mortality in patients with DILI after adjusting for laboratory variables at one week.
| Variable | Coefficient | OR (95% CI) | P |
|---|---|---|---|
| Encephalopathy | 4.485 | 88.69 (4.85-162) | 0.002 |
| MELD score (1 week) | 1.710 | 5.53 (1.16-26.25) | 0.032 |
| ALP (1 week) | 1.986 | 7.29 (1.31-40.56) | 0.023 |
ALP: Alkaline phosphatase. CI: Confidence interval. MELD: Model for End Stage Liver Disease. OR: Odds ratio. Constant = - 3.798.
Drug induced liver injury still remains a challenge in modern day hepatology. Although it is relatively rare cause of liver injury, the overall mortality associated with DILI is significant across all regions of the world. In our series, overall mortality was 15.85%. Overall mortality from 10 to 17.3% has been observed in several series.1,2,5-7 However, in the study from Iceland, out of 11 deaths, only 1 patient died as consequence of DILI.1 In our series, 8 deaths were related to liver injury. A study from Thailand13 reported 26% mortality with DILI caused by antimicrobial agents. In this study, 21 out of 26 deaths due to all causes (76%) were observed in patients with ATT DILI. This is similar to our study in which 70% of deaths due to all causes was seen in ATT DILI patients. Also, the liver related mortality was significantly higher in ATT group as compared to non-ATT group (17.5% vs. 2.4%), which was also reported in the previous study from India.5 However, there was no significant difference in overall mortality between the two groups, as also observed in the study from Thailand.13
Similar to our study, other studies from different regions of the world including Indian subcontinent, antimicrobial agents remained the commonest cause of DILI.1,2,8 However, different class of antimicrobials was found to be causative in these studies, probably reflecting the differences in common infectious diseases seen in these regions. Tuberculosis being one of the most common infectious diseases in our country, ATT was amongst the most commonly implicated drugs, as observed by other studies from this region.5,13 Although CAM is increasingly being reported worldwide to cause DILI, our series reported 10% of patients due to CAM.
In contrast to several previous studies1,14,15 older age and female gender were not associated with increased risk of DILI in our study. The median age in previous studies was 58 years14,15 and 56% patients were females.1,15 The male-to-female gender ratio was 1:1 in our series similar to that observed by the Spanish group.8 The median age in our study was 38 years, as also observed in the previous study from India.5 Thus, in our series, with comparatively younger patients and equal gender ratio, it appears that neither older age nor female sex is predisposing factors for DILI. Similar observation was reported by the Lucena, et al. in the Spanish group.16 Symptoms of nausea, vomiting, and abdominal pain could be related to DILI or merely reflect general adverse effects related to the drug intake. It could not be differentiated. However, the criteria for DILI required laboratory parameters regardless of symptoms for inclusion in the study.
We also analyzed if different patterns of liver injury could predict severity and outcome in DILI patients. However, although patients with cholestatic liver injury appeared to have higher proportion of moderate and severe injury as compared to hepatocellular or mixed type (P value 0.06), there was no significant difference in overall as well as liver related mortality in these groups. Similarly, in the DILIN prospective study,2 authors found that hepa-tocellular cases had higher proportions that were mild, as found in our series. Although hepatocellular cases had a higher frequency of fatal cases (liver related deaths or transplantation), there was no significant difference in overall as well as liver related mortality between the 3 types of liver injury. In the study from China, 9.9% mortality was reported in patients with hepatocellular damage and 9.5% in patients with cholestatic/mixed damage (P < 0.05).17 However, the difference was very small. Similarly, in the Spanish and Swedish studies hepatocellular type of liver injury was associated high but variable mortality rate, depending on the presence of jaundice or drug in-volved.8,14 The differences in observations made by several authors could be due the fact that these patterns of liver disease are not mutually exclusive18 and the pattern of liver disease may change from one type to another as injury progresses.19 Hence, the usefulness of different patterns of liver injury in predicting severity and outcome of DILI is questionable and needs further evaluation.
There are few studies that have reported predictors of outcome in DILI.5,8,13,14,17,20,21 In all these studies, various independent risk factors for acute liver failure or mortality were identified. These included hepatocellular damage, high bilirubin and female sex,8 high MELD score or a combination of encephalopathy, ascites, high bilirubin, pro-thrombin time and leucocyte count,5 presence of jaundice,13 age, AST and bilirubin in the hepatocellular group, whereas bilirubin in the cholestatic/mixed liver injury group,14 hepatic encephalopathy, ascites, jaundice, alcohol abuse and direct bilirubin,17 female gender, high total bilirubin and high AST:ALT ratio,20 high MELD and low hemoglobin.21 Similar to these studies, our study also found jaundice and encephalopathy as independent clinical predictors of mortality. However, laboratory variables at one week predicted mortality better than those at initial recognition of DILI. This is a unique finding in our study. The probable explanation to this finding is due to the fact that in some instances, bilirubin, ALT or ALP may continue to rise for several days even after the drug is stopped.22 Besides, the R value may advance towards cholestatic type of liver injury (i.e. R ≤ 2) with progression of the disease.23 The other reason for this could be, delay in access to tertiary care centers and in recognition of DILI. This is the limitation of the study and needs further evaluation in larger studies.
In our study, baseline alkaline phosphatase (ALP) in the patients receiving ATT was normal. Gamma glutamyl transferase (GGT) was done only in few patients with borderline ALP, to exclude pretreatment cholestatic liver damage or bone disease due to the tuberculosis. Hence, GGT values were not included in the analysis of final data. Also, the natural outcome of DILI would be affected by interventions like liver transplantation which is not easily available for the patients from low middle income country like ours. The risk for DILI involves several interrelated factors. However, there is little data available to support the validity of these factors.24 The natural course of DILI without transplantation would help to predict actual factors that are associated with mortality. This would help us identify those patients who would benefit the most from referral to centers with transplantation facility in a country with financial constraints like India.
Limitations of the study include a relatively small sample size of the study, study based in single tertiary care center and non-availability of transplantation facility.
ConclusionsDILI results in significant overall mortality (15.85%). ATT, anti-epileptic drugs, CAM and antiretroviral drugs are leading causes of DILI in India. Presence of jaundice, encephalopathy, MELD score at one week, and alkaline phosphatase at one week are independent predictors of mortality. The unique finding in our study was that the laboratory variables at one week predicted mortality better than those at initial recognition of DILI, however, it needs further evaluation in larger studies.
AcknowledgementAuthors are thankful to Dr. Harshad Devarbhavi, Professor and Head, Department of Gastroenterology, St. John's Medical College Hospital, Bangalore, for his guidance during the study.
Abbreviations- •
ALP: Alkaline phosphatase.
- •
ALT: Alanine aminotransferase.
- •
AST: Aspartate aminotransferase.
- •
ATT: Antitubercular therapy.
- •
CAM: Complementary and alternative medicine.
- •
DILI: Drug-induced liver injury.
- •
GGT: Gamma glutamyl transferase.
- •
INDILI: Indian Network for DILI.
- •
MELD: Model for End Stage Liver Disease.
- •
NSAIDS: Non-steroidal anti-inflammatory drugs.
- •
RUCAM: Roussel Uclaf Causality Assessment Method.
- •
SD: Standard deviation.
- •
ULN: Upper limit of normal.
None.
Potential Competing InterestsNone.