There is no consensus on the best treatment option for choledocholithiasis. Therefore, the aim of this study was to compare endoscopic retrograde cholangiopancreatography (ERCP) and common bile duct surgery (CBDS) for the treatment of choledocholithiasis.
Materials and methodsWe performed a systematic review of randomized controlled trials (RCTs) comparing ERCP and CBDS in the treatment of choledocholithiasis. MEDLINE and EMBASE were the used databases. RCTs assessing mortality, bile duct clearance failure, complications, or length of hospital stay were considered eligible. Meta-analysis was performed using random effects model, through the Mantel–Haenszel method for binary outcomes and through the inverse variance method for continuous outcomes. The quality of the evidence was evaluated according to the Grading of Recommendations Assessment, Development and Evaluation Working Group. The study protocol was registered at the PROSPERO platform (CRD42017073196).
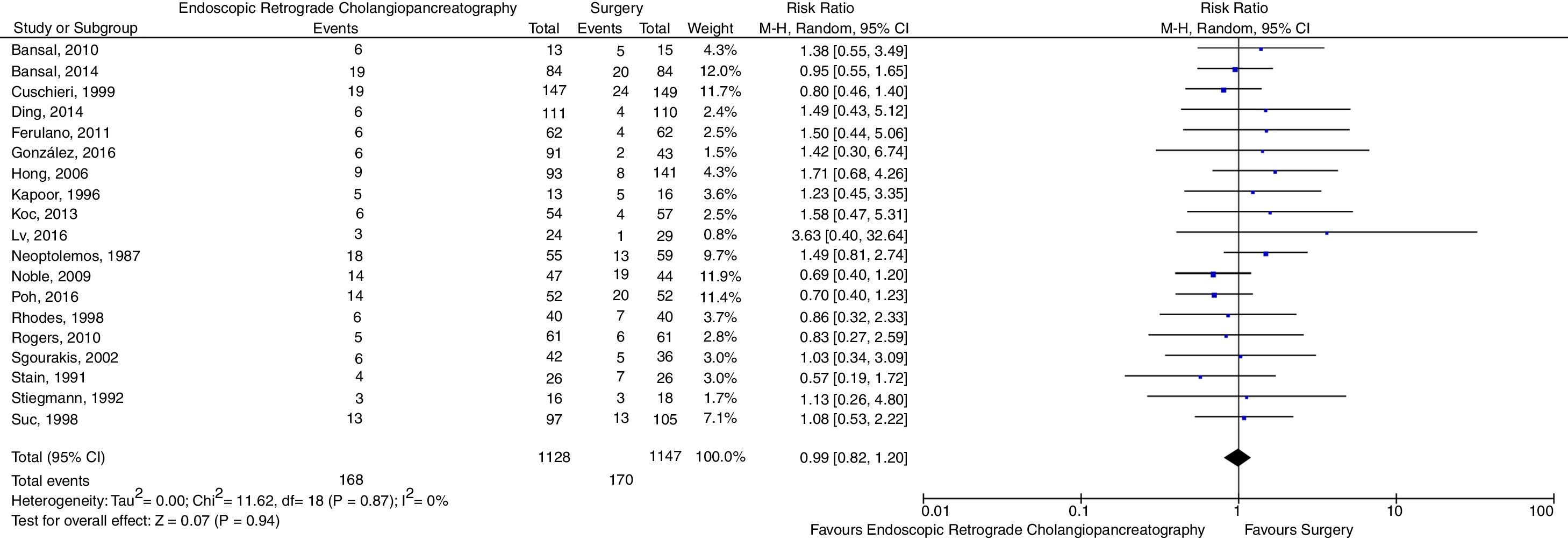
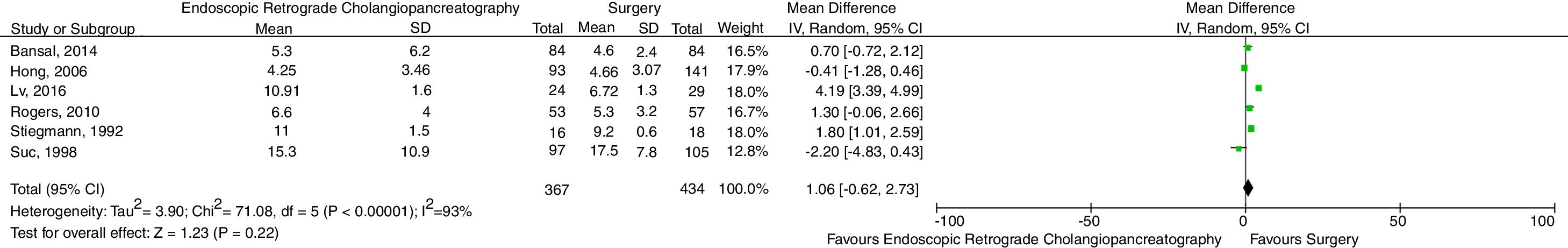
ResultsNineteen RCTs (2466 patients) were included in the meta-analysis. There was no evidence of significant difference between interventions regarding mortality (risk ratio – RR=1.31, 95% confidence interval – 95% CI=0.60–2.85, p=0.49), bile duct clearance failure (RR=1.17, 95% CI=0.86–1.59, p=0.31), complications (RR=0.99, 95% CI=0.82–1.20, p=0.94) and length of hospital stay (weighted mean difference – MD=1.06, 95% CI=−0.62–2.73, p=0.22). Sensitivity analyses failed to demonstrate significant changes in results compared to the main analyses. The quality of the evidence was considered to be low.
ConclusionThere was no evidence of significant difference between ERCP and CBDS for the treatment of choledocholithiasis.
Estimates are that about 10–20% of people will have cholelithiasis [1] and that 15% of these will develop choledocholithiasis [2]. There is no consensus on the best treatment option. There seems to be a tendency in current medical literature of suggesting laparoscopic cholecystectomy associated with common bile duct surgery (CBDS) [3]. However, 75% of the surgeons in the United States choose to manage their patients through endoscopic retrograde cholangiopancreatography (ERCP) followed by laparoscopic cholecystectomy [4]. Some of the reasons for the limited diffusion of laparoscopic CBDS as the first-choice technique are the low reproducibility of results from reference centers [5], the long surgical time and the limited availability of the necessary equipment for such intervention [4]. Recently, the use of intraoperative ERCP (performed at the time of cholecystectomy) is also being studied as a treatment option for patients with choledocholithiasis [6].
While some studies point to an apparent superiority of CBDS over ERCP [3,7,8], other studies show divergent findings [9,10]. Thus, we performed a systematic review with meta-analysis of randomized controlled trials (RCTs) in order to compare the efficacy and safety of these therapeutic alternatives for choledocholithiasis.
2Materials and methodsA systematic review of RCTs comparing ERCP and CBDS was conducted using MEDLINE and EMBASE databases. Search and data extraction were performed by independent investigators (FCS, SMG and FJPT), using a predefined data collection sheet. In case of disagreement, differences were settled by a senior researcher (AZM). Databases were last searched in January 2018, and there were no limitations regarding language or date of publication. The search strategy used for MEDLINE was as follows: (((choledocholithiasis) AND Cholangiopancreatography, Endoscopic Retrograde) AND surgery) AND (((randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized controlled trials[mh] OR random allocation[mh] OR double-blind method[mh] OR single-blind method[mh] OR clinical trial[pt] OR clinical trials[mh] OR (“clinical trial”[tw]) OR ((singl*[tw] OR doubl*[tw] OR trebl*[tw] OR tripl*[tw]) AND (mask*[tw] OR blind*[tw])) OR (“latin square”[tw]) OR placebos[mh] OR placebo*[tw] OR random*[tw] OR research design[mh:noexp] OR follow-up studies[mh] OR prospective studies[mh] OR cross-over studies[mh] OR control*[tw] OR prospective*[tw] OR volunteer*[tw]) NOT (animal[mh] NOT human[mh]))). An analogous search strategy was used for EMBASE.
Studies were considered eligible if they were RCTs; evaluated patients with choledocholithiasis not previously submitted to cholecystectomy; compared ERCP and CBDS in a head-to-head manner; evaluated at least one of the outcomes of interest, namely mortality, bile duct clearance failure, complications and length of hospital stay. Studies in pediatric population and studies published exclusively in the form of abstracts were excluded. The quality of the evidence was assessed according to the Grading of Recommendations Assessment, Development and Evaluation Working Group (GRADE).
The primary outcome was mortality by any cause. Secondary outcomes were bile duct clearance failure (for this outcome, data on bile duct stone extraction failure and on retained stones during follow-up were considered), complications associated with procedures and length of hospital stay. A random effects model was used, anticipating the possible heterogeneity among the populations evaluated in each study. Data were collected according to intention-to-treat analyses whenever they were available. Otherwise, data from per protocol analyses were accepted. For binary outcomes, risk ratio (RR) with a 95% confidence interval (CI) was chosen as the main effect measure, and the Mantel–Haenszel method was used in the analysis. For continuous outcomes, weighted mean difference (MD) with 95% CI was chosen as the main effect measure, and the inverse variance method was used in the analysis. Statistical significance was set at p<0.05. Heterogeneity was assessed by the I2 statistic (I2≥50% indicated relevant heterogeneity) and by the Cochran Q test (p<0.10).
Publication bias was assessed through funnel plot analysis when 10 or more studies were included in the meta-analysis of a given outcome. Sensitivity analyses were planned excluding studies in which an intraoperative ERCP was performed; excluding studies in which the primary surgical technique was not laparoscopic; and, in cases of heterogeneity, excluding each study at a time. The Review Manager 5.3 software (The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark) was used in the analyses. The suggestions of the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes – PRISMA statement were followed. The study was registered in PROSPERO platform under the number CRD42017073196.
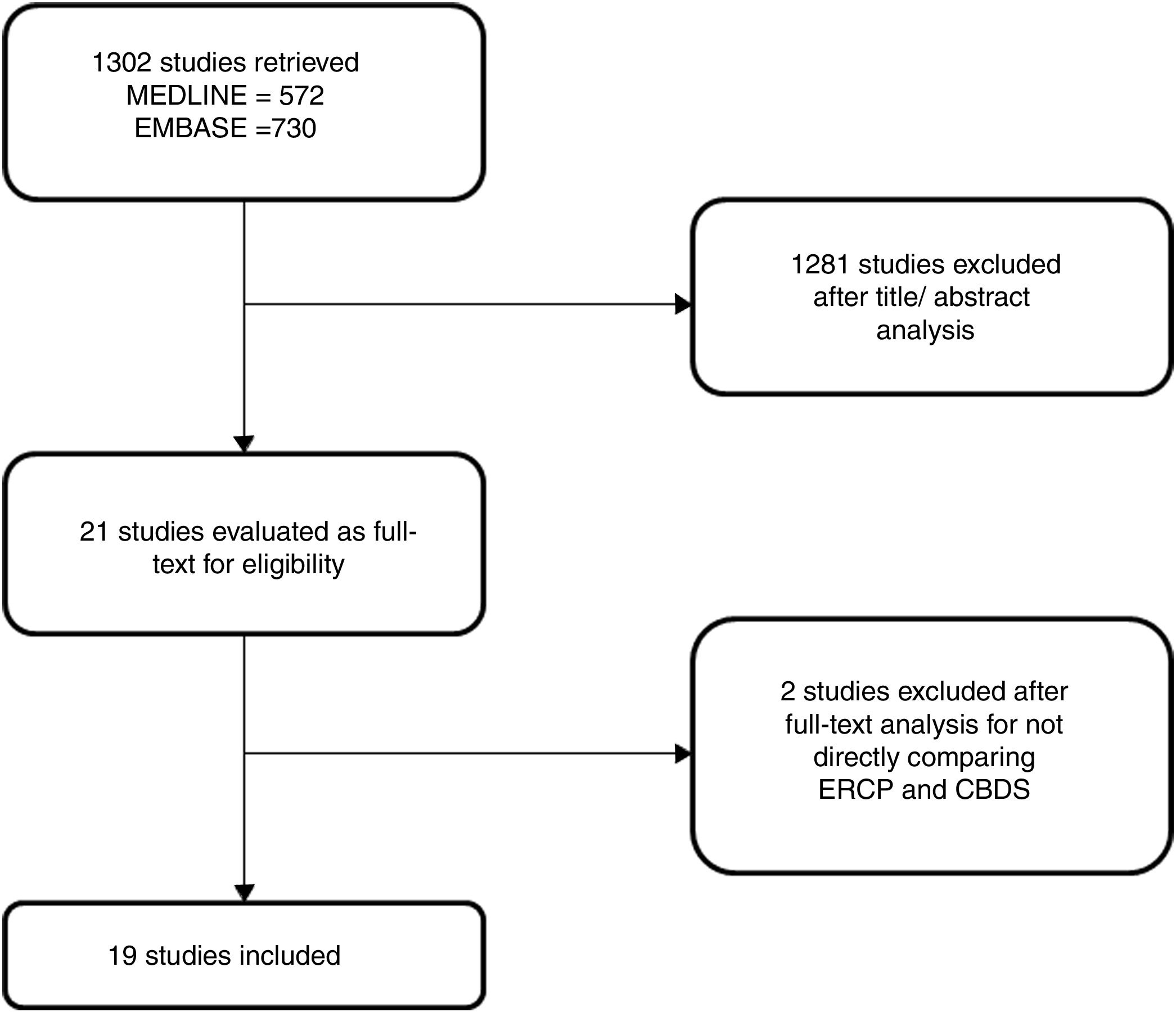
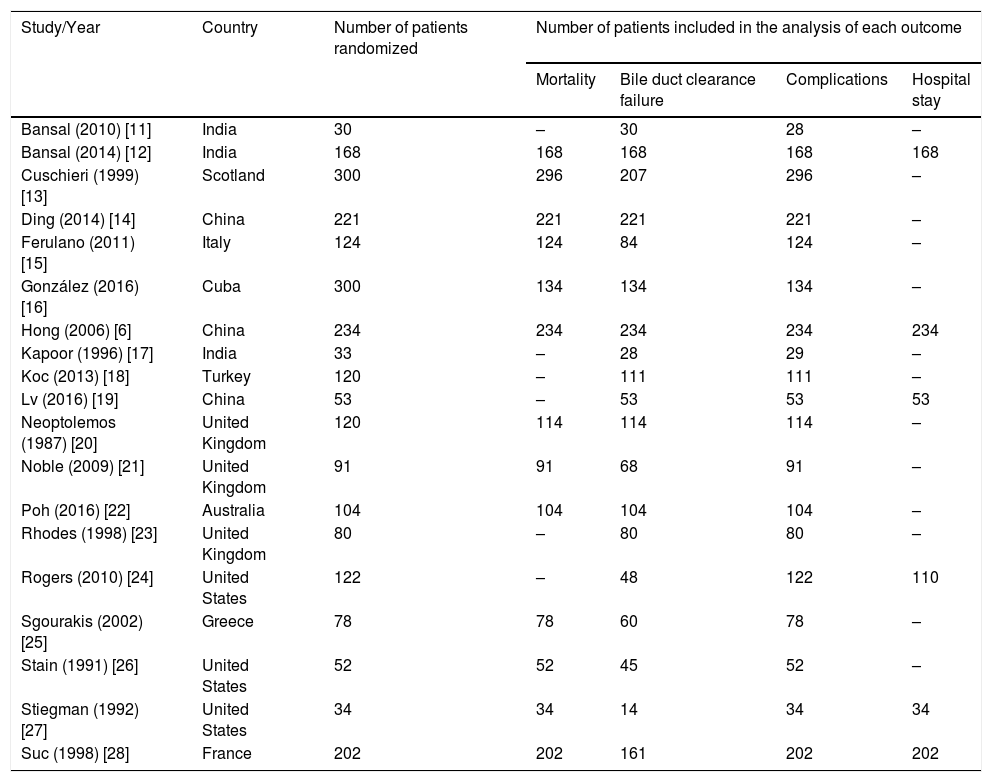
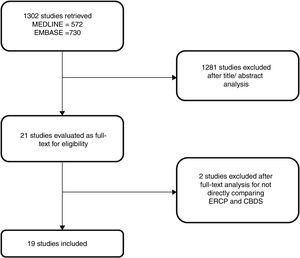
3ResultsThe search strategy retrieved 1302 references. After exclusion of duplicates and evaluation of titles and abstracts, 1281 were excluded and 21 were selected for full text analysis. After the full text analysis, 2 studies were excluded for not directly comparing ERCP with CBDS. Finally, 19 studies, with 2466 patients, were included in the meta-analysis (Table 1) [6,11–28]. The flowchart of the systematic review is shown in Fig. 1.
Characteristics of included studies.
| Study/Year | Country | Number of patients randomized | Number of patients included in the analysis of each outcome | |||
|---|---|---|---|---|---|---|
| Mortality | Bile duct clearance failure | Complications | Hospital stay | |||
| Bansal (2010) [11] | India | 30 | – | 30 | 28 | – |
| Bansal (2014) [12] | India | 168 | 168 | 168 | 168 | 168 |
| Cuschieri (1999) [13] | Scotland | 300 | 296 | 207 | 296 | – |
| Ding (2014) [14] | China | 221 | 221 | 221 | 221 | – |
| Ferulano (2011) [15] | Italy | 124 | 124 | 84 | 124 | – |
| González (2016) [16] | Cuba | 300 | 134 | 134 | 134 | – |
| Hong (2006) [6] | China | 234 | 234 | 234 | 234 | 234 |
| Kapoor (1996) [17] | India | 33 | – | 28 | 29 | – |
| Koc (2013) [18] | Turkey | 120 | – | 111 | 111 | – |
| Lv (2016) [19] | China | 53 | – | 53 | 53 | 53 |
| Neoptolemos (1987) [20] | United Kingdom | 120 | 114 | 114 | 114 | – |
| Noble (2009) [21] | United Kingdom | 91 | 91 | 68 | 91 | – |
| Poh (2016) [22] | Australia | 104 | 104 | 104 | 104 | – |
| Rhodes (1998) [23] | United Kingdom | 80 | – | 80 | 80 | – |
| Rogers (2010) [24] | United States | 122 | – | 48 | 122 | 110 |
| Sgourakis (2002) [25] | Greece | 78 | 78 | 60 | 78 | – |
| Stain (1991) [26] | United States | 52 | 52 | 45 | 52 | – |
| Stiegman (1992) [27] | United States | 34 | 34 | 14 | 34 | 34 |
| Suc (1998) [28] | France | 202 | 202 | 161 | 202 | 202 |
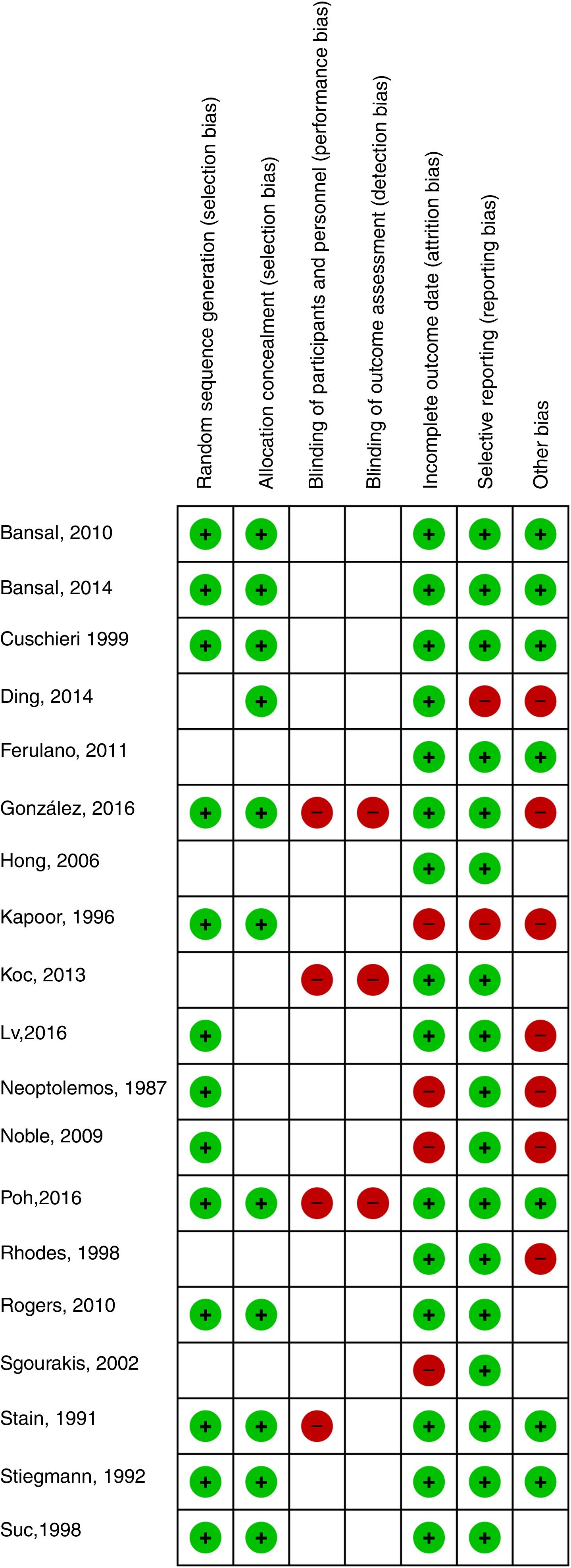
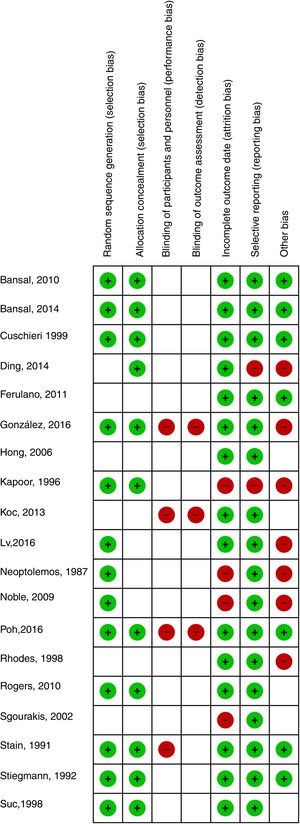
All included studies compared ERCP and CBDS in a head-to-head manner. Mortality was described in 13 studies, bile duct clearance failure and complications were described in 19 studies, and the mean length of hospital stay with standard deviation was provided in 6 studies. The quality of the evidence was considered to be low according to GRADE (Fig. 2).
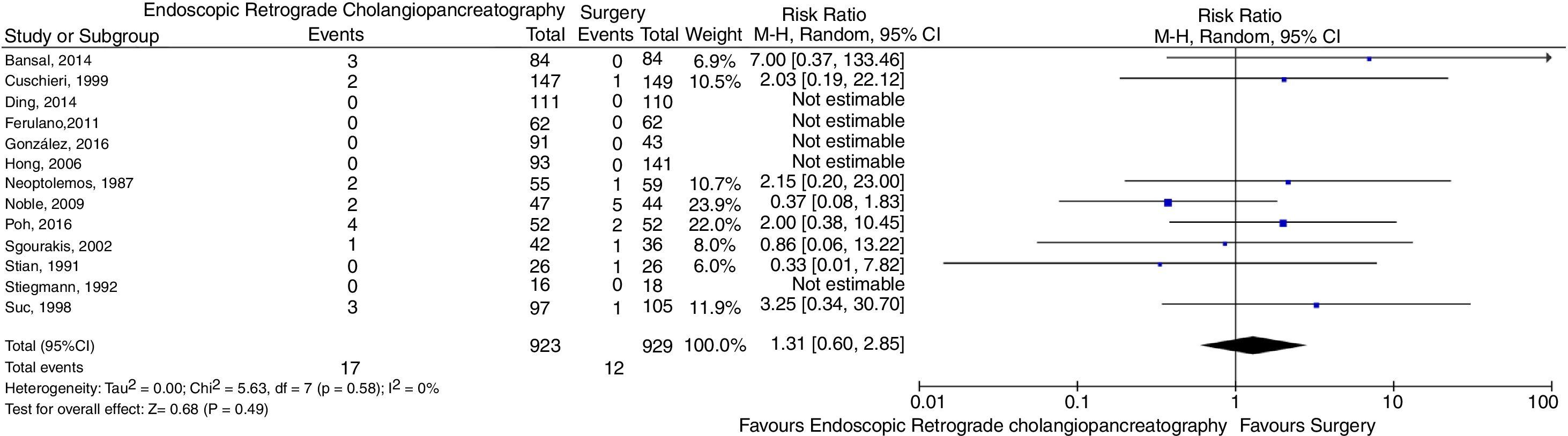
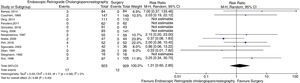
Regarding mortality, there was no evidence of significant difference between the interventions (RR=1.31, 95% CI=0.60–2.85, p=0.49, I2=0%). The forest plot is shown in Fig. 3. Sensitivity analysis was performed excluding studies using open surgery [20,26,27], without any significant change in results (RR=1.36, 95% CI=0.58–3.18, p=0.48, I2=0%). Sensitivity analysis excluding studies using intraoperative ERCP was not performed because these studies did not contribute with events in the main analysis.
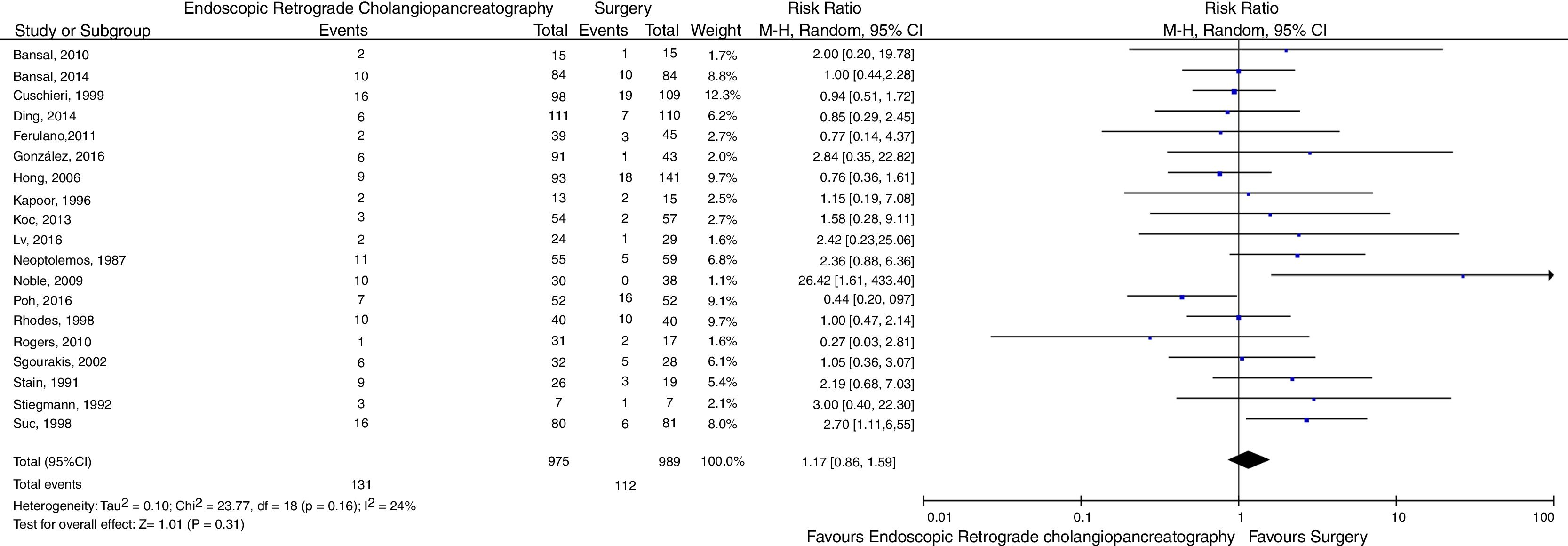
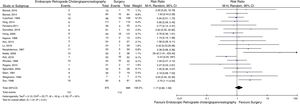
Concerning bile duct clearance failure, there was also no evidence of significant difference between ERCP and CBDS (RR=1.17, 95% CI=0.86–1.59, p=0.31, I2=24%). The forest plot is shown in Fig. 4. Sensitivity analysis was performed excluding studies using open technique [17,20,26,27], with no relevant changes in the findings (RR=1.04, 95% CI=0.74–1.45, p=0.83, I2=26%). Another sensitivity analysis was performed, excluding studies using intraoperative ERCP [6,22], demonstrating RR=1.35 (95% CI=1.00–1.82, p=0.05, I2=7%).
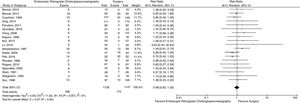
Regarding complications, again there was no evidence of significant difference between the evaluated therapeutic techniques (RR=0.99, 95% CI=0.82–1.20, p=0.94, I2=0%). The forest plot is shown in Fig. 5. In the sensitivity analysis which excluded studies using open surgery [17,20,26,27], there were no changes in the findings (RR=0.95, 95% CI=0.77–1.18, p=0.66, I2=0%). The sensitivity analysis excluding the studies using intraoperative ERCP [6,22] also did not significantly modify the results (RR=1.03, 95% CI=0.83–1.26, p=0.81, I2=0%).
Regarding length of hospital stay, no evidence of significant difference between treatments was found (MD=1.06, 95% CI=−0.62–2.73, p=0.22, I2=93%). The forest plot is shown in Fig. 6. Due to the high heterogeneity among studies, sensitivity analyses were performed excluding each study at a time, without however detecting relevant changes in the findings.
In the evaluation of funnel plots, there was possible publication bias regarding bile duct clearance failure and complications (data not shown). Funnel plots were not developed for mortality and length of hospital stay since less than 10 studies contributed with events for each of these outcomes.
4DiscussionCholedocholithiasis is an important complication of cholelithiasis. Its treatment can be performed through ERCP followed by cholecystectomy or CBDS associated with cholecystectomy at the same surgical time. To date, there is no clarity as to the best therapeutic option for choledocholithiasis. The present study is the most comprehensive meta-analysis on the subject and did not identify evidence of significant difference between the evaluated interventions.
The results of this systematic review are in line with those of a recent meta-analysis published by Singh et al. [29], regarding the absence of significant difference between ERPC and surgery regarding mortality and complications. On the other hand, contrary to our findings, the study by Singh et al. [29] showed that length of hospital stay was shorter with surgical treatment than it was with ERCP. This difference could be explained by the fact that our systematic review included more studies than that published by Singh et al. [29] The absence of difference between these treatments regarding length of hospital stay could be considered counterintuitive, but one must keep in mind that CBDS associated to cholecystectomy is a much more complex surgical procedure than cholecystectomy alone, which might lead to a more prolonged postoperative recovery, compensating for the time spent between ERCP and cholecystectomy.
Data from two other meta-analyses have shown conflicting results when compared to the present study. Zhu et al. [8] found evidence of superiority of surgery over ERCP, since there was greater bile duct clearance and shorter hospital stay in the surgical group, with no evidence of difference regarding mortality and total postoperative morbidity. These differences may be explained by the fact that the systematic review by Zhu et al. [8] included only 8 studies and by the inclusion of a study [30] which evaluated patients who had previously failed surgical trans-cystic duct clearance, a population which is different from that assessed by the other studies. In addition, authors chose to use a fixed effects model in the meta-analysis, which could be inadequate due to the heterogeneity of the populations evaluated in the different trials. The weakness of the results of the study by Zhu et al. [8] can be seen in their own sensitivity analysis regarding bile duct clearance, in which the difference between both treatments disappeared.
The other meta-analysis with results that differ from ours was published by Dasari et al. [9]. The authors found evidence of superiority of the open surgery group over ERCP with regard to bile duct clearance, with no difference in mortality or complications. That benefit, however, was verified using the fixed effects model in the meta-analysis, which seems inappropriate given the heterogeneity of the populations studied in the different trials. When the analysis was performed using random effects model, that benefit was no longer identified, which is in agreement with our findings. Moreover, it must be taken into account that open surgery has become increasingly obsolete and that, when the trials using this technique were performed, ERCP was probably in its early stages of development, which could justify finding worse results. When only laparoscopic surgeries were evaluated, no evidence of difference was found between ERCP and CBDS.
Two other meta-analyses had results which are similar to ours. The studies by Lu et al. [10] and Prasson et al. [31] failed to find evidences of significant differences between the evaluated treatments. Nevertheless, it must be highlighted that both systematic reviews included less trials than ours and that both of them included a study [30] which evaluated patients who had previously failed surgical trans-cystic duct clearance, a population which differs from those assessed by other trials.
The results of the present study are robust since there was no evidence of significant differences between the interventions for any of the different endpoints, even after sensitivity analyses. In addition, there was no significant heterogeneity among the included studies, except for the outcome length of hospital stay. Specifically regarding bile duct clearance failure, it is noteworthy that the sensitivity analysis that excluded studies using intraoperative ERCP suggested a possible trend in favor of surgical treatment. Nevertheless, it should be considered that studies using intraoperative ERCP presented some of the best results for the endoscopic treatment, possibly because they are among the most recent trials.
Despite being the most comprehensive meta-analysis on the subject and presenting robust results, some considerations regarding included studies are in order. The studies were carried out over almost three decades, a period in which technical and technological developments certainly took place. In addition, the studies presented some variability regarding the employed therapeutic techniques. Sensitivity analyses aimed at minimizing the impact of these issues.
Another limitation of the present study concerns especially the evaluation of mortality and length of hospital stay, for which the number of included studies and the number of recorded events were below ideal. Nonetheless, as previously mentioned, this is the most comprehensive systematic review on the subject.
Regarding quality of the evidence, some limitations should also be noticed. None of the studies was blinded. Six studies did not adequately describe the generation of the randomization sequence, and 8 did not properly describe allocation concealment. In addition, 4 trials presented attrition bias, and 2 presented reporting bias. For these reasons, the quality of the evidence was considered to be low, which evidently requires careful interpretation of our findings.
Yet another limitation of this meta-analysis might be the identification of possible publication bias. It is known that negative studies are less likely to be published, which could have interfered with our results. However, considering that the present study found no evidence of significant differences between ERCP and CBDS, if more negative studies were to be published, our findings would probably remain the same.
In conclusion, the present meta-analysis found no evidence of significant differences between ERCP and CBDS for the treatment of choledocholithiasis. Therefore, we consider that the therapeutic choice between ERCP and CBDS should be made on a case-by-case basis and according to local expertise.
AbbreviationsERCP
endoscopic retrograde cholangiopancreatography
RCTsrandomized controlled trials
CBDScommon bile duct surgery
GRADEGrading of Recommendations Assessment, Development and Evaluation Working Group
RRrisk ratio
CIconfidence interval
Author contributionsSchacher FC contributed for acquisition of data, analysis and interpretation of data, drafting of the manuscript and approval of the final version of the manuscript. Giongo SM contributed for acquisition of data, analysis and interpretation of data, critical revision of the manuscript for important intellectual content and approval of the final version of the manuscript. Teixeira FJP contributed for acquisition of data, analysis and interpretation of data, critical revision of the manuscript for important intellectual content and approval of the final version of the manuscript. Mattos AZ contributed for the study concept and design, statistical analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content and approval of the final version of the manuscript.
Financial supportThere was no financial support.
Conflict of interestThere are no conflicts of interest to declare.