Introduction. Few studies have evaluated the factors involved in the spontaneous HBsAg seroclearance in patients with chronic hepatitis B (HBV) followed up on a long-term basis from areas with a low prevalence of HBV infection. We aimed to determine the rate of spontaneous HBsAg seroclearance and the factors related to it in patients with chronic HBV infection followed up at the Hepatitis Outpatient Clinic of HCFMRP from 1992-2008.
Materials and methods. A total of 548 patients with chronic HBV infection (366 with chronic hepatitis B and 182 inactive carriers) were followed for 15 years and 9 months with an annual measurement of HBV-DNA, ALT, AST and GGT (average of 4 annual determinations) and serology (HBsAg, HBeAg, Anti-HBeAg and Anti-HBsAg).
Results. Spontaneous HBsAg seroclearance occurred in 40 patients (7.3%) with a mean age of 46.0 ± 14.4 years, corresponding to an annual rate of 0.7%.The factors related to spontaneous HBsAg seroclearance were inactive carrier status (67.5 vs. 32.5%, p = 0.000191) and age of more than 40 years (p = 0.0007). There was no difference in the rate of spontaneous HBsAg seroclearance when comparing males and females (p = 0.383). Patients with spontaneous HBsAg seroclearance did not progress to more severe forms of the disease during follow-up.
Conclusion. Spontaneous HBsAg seroclearance has a favorable long-term prognosis in patients with chronic HBV infection. HBsAg seroclearance occurred at rates compatible with low prevalence areas and was associated with low serum HBV-DNA levels and an age older than 40 years.
Hepatitis B virus infection (HBV) isa global public health concern, especially in developing countries. It is estimated that there are 50 to 400 million individuals chronically infected with HBV world-wide.1,2 In Brazil, studies carried out in state capitals and in large cities have shown data consistent with low or intermediate levels of endemicity, except for the Amazon region and some regions of Santa Catarina, Paraná, and Espírito Santo, where the prevalence was high.3–9
Chronic HBV infection is associated with a risk of developing severe forms of hepatic disease, such as cirrhosis, hepatic insufficiency and hepatocellular carcinoma (HCC).1,2,10,11
Several epidemiological studies have demonstrated that seropositivity of the hepatitis B surface antigen (HBsAg) represents an important risk factor for disease progression, including cirrhosis and HCC.12–15 A negativation of HBsAg during the course of HBV infection can be considered as resolved hepatitis B infection.12,13,16 Some patients clear HBsAg spontaneously, which usually confers a good long-term prognosis in the absence of cirrhosis or concomitant infections with hepatitis C or D virus at the time of seroclearance.17–21 However, HBsAg seroclearance occurs in a small proportion of patients during the natural history of chronic HBV infection, with an estimated annual incidence of 1 to 2% in western countries20,22,23 and an even lower incidence of 0.1 to 0.8% in patients from endemic areas for HBV, where infection is usually acquired during the neonatal periods or at the start of childhood.24,26
Previous studies have reported low HBV-DNA levels, genotype B infection and male as factors related to higher likelihood of spontaneous HBsAg seroconversion.21,25
Few studies are currently available, specifically regarding Brazil,22 that evaluate the possible factors related to spontaneous HBsAg seroconversion in the natural history of chronic HBV infection. Thus, the objective of the present study was to determine possible factors related to spontaneous HBsAg seroconversion in a group of 548 patients with a diagnosis of chronic HBV infection followed at the Hepatitis Outpatient clinics of the University Hospital, Faculty of Medicine of Ribeirão Preto, University of São Paulo (HCFMRP-USP), during the period from January 1992 to September 2008.
Material and MethodsPatientsA total of 548 patients with a diagnosis of chronic HBV infection were evaluated from January 1992 to September 2008.
The diagnosis of chronic hepatitis B was based on the positivity of the surface antigen of hepatitis B (HBsAg) and of the IgG antibody against the core antigen of hepatitis B virus (anti-HBcAg IgG) for a period of more than 6 months.
Spontaneous HBsAg seroclearance was defined as HBsAg negativity in serum with or without anti-HBsAg positivity (> 10 IU) in the absence of any antiviral treatment since the date of diagnosis of the infection.
Patients co-infected with hepatitis C virus (HCV) or with human immunodeficiency virus (HIV) and patients with other hepatic diseases were excluded from the study.
Clinical and laboratory data at the beginning of the study and during follow-upDuring follow-up, serum liver enzymes [alanine aminotransferase (ALT), aspartate aminotransferase (AST) and gamma glutamyl transferase (GGT)] were measured four times a year on average. Serum albumin, prothrombin time (PT), bilirubins and HBV serologic marker (HBsAg, anti-HBcAg IgG, HBeAg, anti-HBeAg, anti-HCV, anti-HIV) levels were determined, on average, once a year. HBV DNA was also quantified, on average, three times a year.
During follow-up, the patients were classified according to the different stages of the disease as having chronic replicating hepatitis, immunotolerant phase and inactive HBV carriers according to their serologic profile and serum ALT and HBV-DNA levels. The status of inactive HBV carrier was characterized by the presence of HBsAg in serum, persistently normal serum aminotransferase levels, HBeAg negativity, anti-HbeAg positivity and serum HBV-DNA levels that were undetectable or lower than 2 x 103 IU/mL.1 Chronic replicating hepatitis B was characterized by the presence of HBsAg in serum, elevated serum aminotransferase levels, HBeAg negativity or positivity, and serum HBV-DNA levels equal to or higher than 2 x 103 IU/mL. Immunotolerant phase was characterized by the presence of HBsAg in serum, normal serum aminotransferase levels, HBeAg positivity and high serum HBV-DNA levels.
Liver biopsy was performed in 260 patients during the follow-up period. The classification of Knodell, et al. (1981), modified by Desmet, et al. (1994), was used to define the stage of fibrosis (scores 0-4) and necroinflammatory activity [histologic activity index (HAI scores 0-18)].
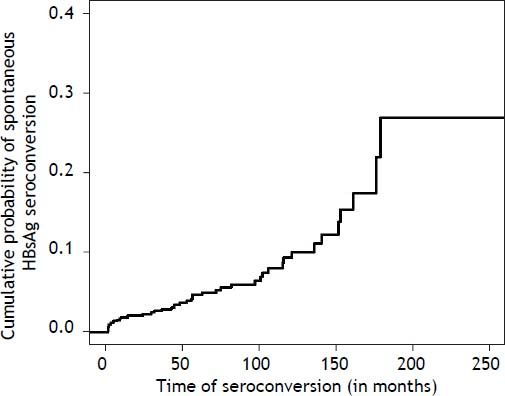
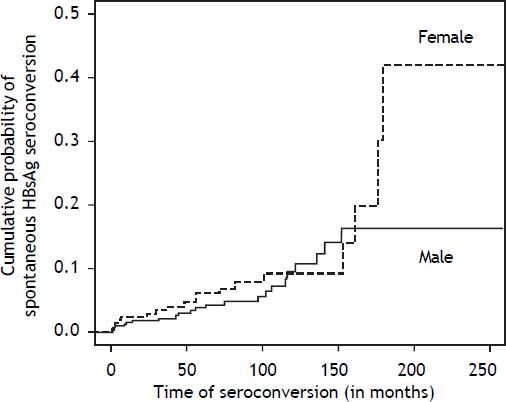
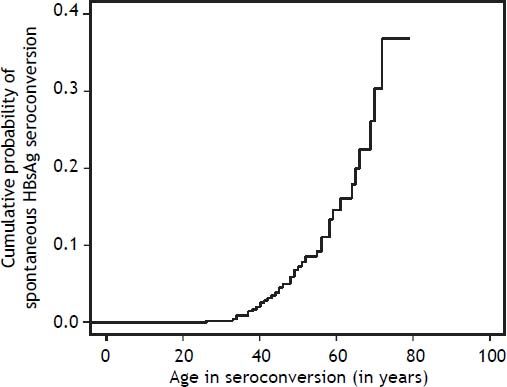
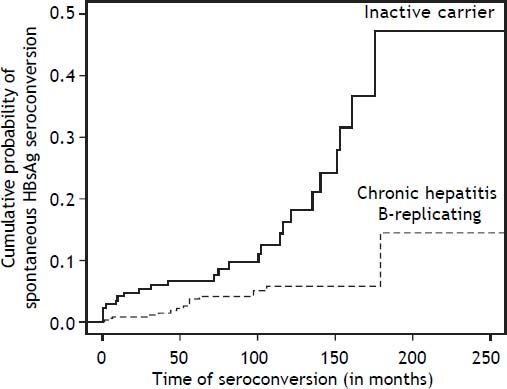
To assess the probability of spontaneous HBsAg seroclearance, we considered the value estimated using the Kaplan-Meier method for the group as a whole (548 patients), according to sex, evolutionary form of the disease (inactive carriers and chronic replicating hepatitis B), and patient age at the time of the event.
Epidemiological dataDuring the follow-up period, the patients were evaluated in a descriptive manner regarding the possible risk factors for the acquisition of chronic HBV infection, alcohol intake and the source of referral of patients.
Ethical aspectsThis study was approved by the Research Ethics Committee of the University Hospital, Faculty of Medicine of Ribeiráo Preto, University of São Paulo, Ribeirão Preto (HC-FMRP-USP) (protocol number 1351/2007).
Statistical analysisFor the comparison of the characteristics of the groups, the χ2 test or Fisher exact test was used to analyze the categorical variables. The qualitative variables are reported as absolute (n) and relative (%) frequency, whereas the quantitative variables are reported as the mean, standard deviation (SD) and median.
The Kaplan-Meier method was used to examine the cumulative probability of spontaneous HBsAg seroclearance, and the differences were determined using the log-rank test.
The event of interest considered for each patient was the time of spontaneous HBsAg seroclearance, in months, from the date of the beginning of follow-up (time when the patients were recognized as having chronic HBV infection) to the date of occurrence of the event of interest.
The collected information was stored in a database using Excel 2007 software (Microsoft Office, Albuquerque, NM). The data were analyzed statistically using SPSS software (version 17.0; SPSS, Chicago, IL). The level of significance was set at p < 0.05 for all analyses.
ResultsA total of 548 patients were evaluated during a period of 15 years and 9 months. There was a predominance of men (61.2%), with a mean age of 37.7 ± 13.3 years at diagnosis. The mean follow-up time was 86.25 months.
Regarding the different evolutionary forms of chronic HBV infection, 277 patients (50.6%) were HBeAg-negative chronic hepatitis and 89 (16.2%) HBeAg-positive chronic hepatitis, whereas 182 (33.2%) were inactive carriers of HBV. Among the patients with chronic hepatitis B and HBeAg-positive, 8 (8.9%) were in the immunotolerance stage, and 81 (91%) were in the immune clearance phase during the follow-up period.
Regarding the staging of fibrosis, the following results were obtained: 140 (53.8%) patients with mild fibrosis, 79 (30.4%) with moderate fibrosis and 41 (15.8%) with severe fibrosis/cirrhosis. Necroinflammatory activity (HAI) was determined in 255 biopsies, and the following results were obtained: 50 patients (19.6%) showed histological activity index (HAI) minimum (score 0-3), 102 (40.0%) had mild HAI (score 4-8), 76 (29.8%) had moderate HAI (score 9-12) and 27 patients (10.6%) had severe HAI (score 13-18).
During the follow-up period, spontaneous HBsAg seroclearance occurred in 40 (7.3%) patients, 29 of whom (72.5%) presented with detectable anti-HBsAg antigen.
In the group of patients with spontaneous HBsAg seroclearance, there was a predominance of men (55.0%) with a mean age of 46.0 ± 14.4 years at the time of HBsAg seroconversion, and 62.5% were inactive carriers, which is the most common evolutionary form of the disease.
At least one risk factor for the transmission of infection was identified in 25 (62.5%) patients with spontaneous seroconversion. Vertical transmission was the most evident risk factor, which was present in 9 patients (22.5%), followed by sexual transmission in 5 patients (12.5%). In 15 patients (37.5%), no risk factor could be determined. More than one risk factor was detected in 8 patients (20.0%). Regarding the referring source, the blood bank was responsible for 40% of cases, followed by medical services, which were responsible for 30% of cases. Most patients (55%) did not consume alcohol, and 5 patients (12%) had an alcohol intake of more than 40 g alcohol/day.
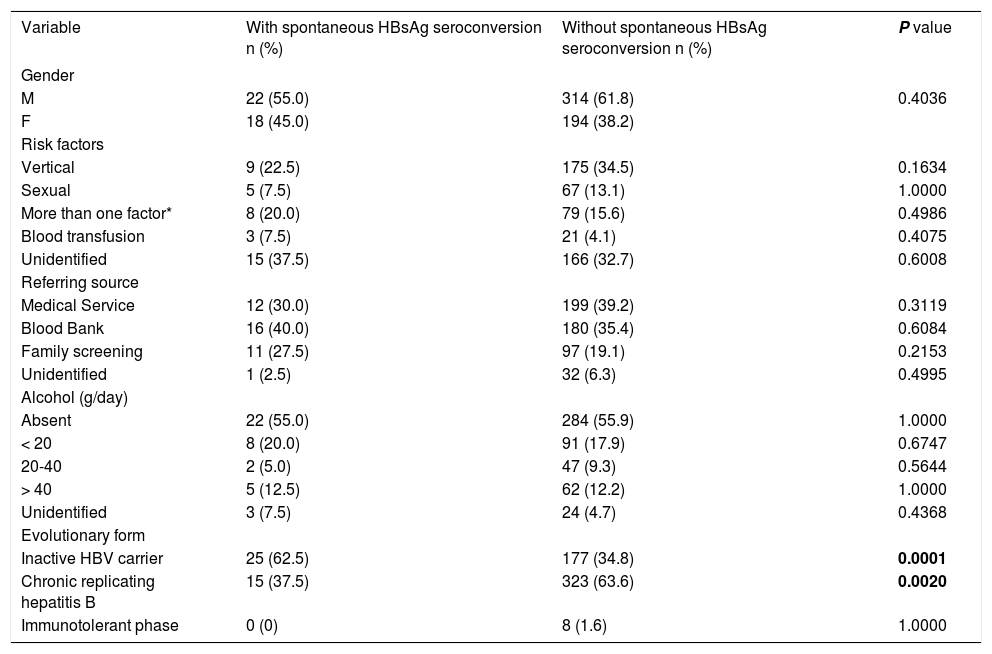
On the other hand in the group of patients without spontaneous HBsAg seroclearance, there was a predominance of men (61.8%) and chronic replicating hepatitis B as the most common evolutionary form of the disease (63.6%). Vertical transmission was the most evident risk factor, which was present in 175 patients (34.5%). Regarding the referring source, the medical services were responsible for 39.2% of cases. The characteristics and comparisons of these patients are shown in tables 1 and 2.
Characteristics of the patients with and without spontaneous HBsAg seroconversion followed up at the Hepatitis Outpatient Clinic of HCFMRP from January 1992 to September 2008.
| Variable | With spontaneous HBsAg seroconversion n (%) | Without spontaneous HBsAg seroconversion n (%) | P value |
|---|---|---|---|
| Gender | |||
| M | 22 (55.0) | 314 (61.8) | 0.4036 |
| F | 18 (45.0) | 194 (38.2) | |
| Risk factors | |||
| Vertical | 9 (22.5) | 175 (34.5) | 0.1634 |
| Sexual | 5 (7.5) | 67 (13.1) | 1.0000 |
| More than one factor* | 8 (20.0) | 79 (15.6) | 0.4986 |
| Blood transfusion | 3 (7.5) | 21 (4.1) | 0.4075 |
| Unidentified | 15 (37.5) | 166 (32.7) | 0.6008 |
| Referring source | |||
| Medical Service | 12 (30.0) | 199 (39.2) | 0.3119 |
| Blood Bank | 16 (40.0) | 180 (35.4) | 0.6084 |
| Family screening | 11 (27.5) | 97 (19.1) | 0.2153 |
| Unidentified | 1 (2.5) | 32 (6.3) | 0.4995 |
| Alcohol (g/day) | |||
| Absent | 22 (55.0) | 284 (55.9) | 1.0000 |
| < 20 | 8 (20.0) | 91 (17.9) | 0.6747 |
| 20-40 | 2 (5.0) | 47 (9.3) | 0.5644 |
| > 40 | 5 (12.5) | 62 (12.2) | 1.0000 |
| Unidentified | 3 (7.5) | 24 (4.7) | 0.4368 |
| Evolutionary form | |||
| Inactive HBV carrier | 25 (62.5) | 177 (34.8) | 0.0001 |
| Chronic replicating hepatitis B | 15 (37.5) | 323 (63.6) | 0.0020 |
| Immunotolerant phase | 0 (0) | 8 (1.6) | 1.0000 |
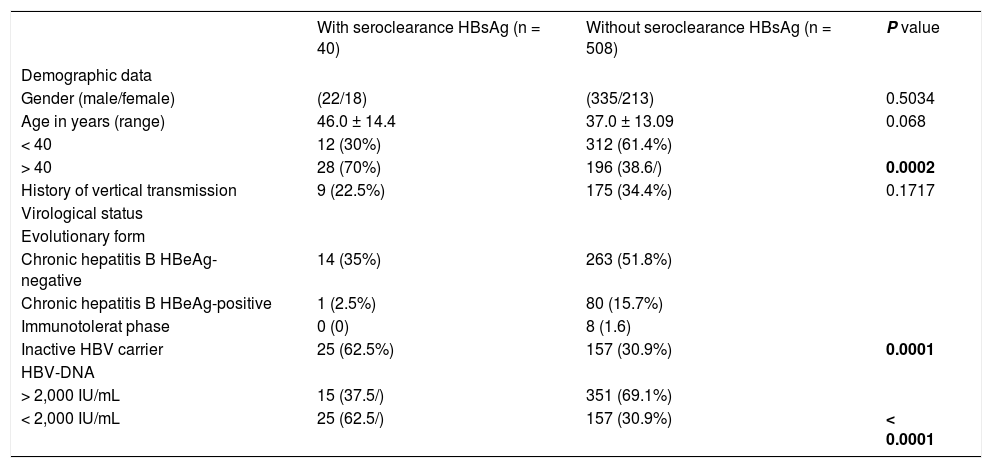
Clinical and laboratory characteristics of 548 patients with HBV infection followed up at the Hepatitis Outpatient Clinic of HCFMRP from January 1992 to September 2008.
| With seroclearance HBsAg (n = 40) | Without seroclearance HBsAg (n = 508) | P value | |
|---|---|---|---|
| Demographic data | |||
| Gender (male/female) | (22/18) | (335/213) | 0.5034 |
| Age in years (range) | 46.0 ± 14.4 | 37.0 ± 13.09 | 0.068 |
| < 40 | 12 (30%) | 312 (61.4%) | |
| > 40 | 28 (70%) | 196 (38.6/) | 0.0002 |
| History of vertical transmission | 9 (22.5%) | 175 (34.4%) | 0.1717 |
| Virological status | |||
| Evolutionary form | |||
| Chronic hepatitis B HBeAg-negative | 14 (35%) | 263 (51.8%) | |
| Chronic hepatitis B HBeAg-positive | 1 (2.5%) | 80 (15.7%) | |
| Immunotolerat phase | 0 (0) | 8 (1.6) | |
| Inactive HBV carrier | 25 (62.5%) | 157 (30.9%) | 0.0001 |
| HBV-DNA | |||
| > 2,000 IU/mL | 15 (37.5/) | 351 (69.1%) | |
| < 2,000 IU/mL | 25 (62.5/) | 157 (30.9%) | < 0.0001 |
Determination of liver enzymes (measured, on average, 4 times a year) in the group of patients with spontaneous HBsAg seroclearance revealed mean ALT values of 40.4 ± 53.5 IU/mL, mean AST values of 38.3 ± 42.1 IU/mL and mean GGT values of 41.6 ± 61.9 IU/mL.
Quantification of serum HBV-DNA (measured, on average, 3 times a year) in the group of patients with spontaneous HBsAg seroclearance revealed mean HBV-DNA values of 12,108.23 ± 38,375.75 IU/mL.
No histological, clinical or ultrasonographic evidence of liver cirrhosis was detected in any patient with spontaneous HBsAg seroclearance.
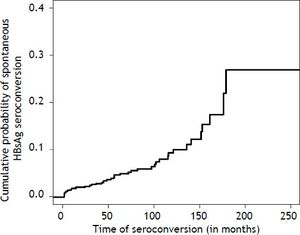
The cumulative probability of spontaneous HB-sAg seroclearance for the present patients with chronic HBV infection was 5.0, 10.0 and 28.0% after 60, 120 and 180 months, respectively, as shown in figure 1.
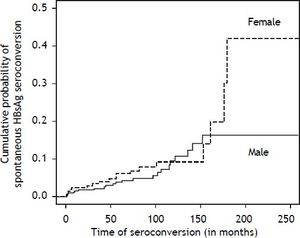
Although a higher prevalence of spontaneous HB-sAg seroclearance was observed in male patients (55 vs. 45%), there was no statistically significant difference in the probability of this event being related to gender, with cumulative probabilities of spontaneous HBsAg seroclearance being 5.0, 9.0 and 14.0% after 50,100 and 120 months, respectively, for women and 3.0, 6.0 and 16.0% after 50, 100 and 120 months, respectively, for men (p = 0.383).
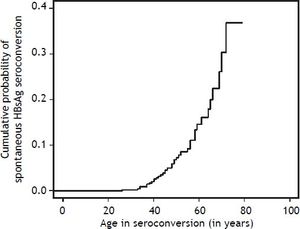
The peak occurrence of spontaneous HBsAg seroclearance was observed between 40 and 60 years of age, occurring after 40 years of age in 67.5% (28/40) of cases. The cumulative probability of spontaneous HBsAg seroclearance was less than 5% in patients younger than 40 years and was 35% in those older than 40 years (p = 0.0007). The cumulative probabilities of spontaneous HBsAg seroclearance according to sex and age are presented in figures 2 and 3, respectively.
Cumulative probability of spontaneous HBsAg seroconversion in patients with chronic HBV infection followed at the outpatient clinics of Hepatitis and Gastroenterology of HCFMRP from January 1992 to September 2008 according to age. * p = 0.0007 comparing patients younger than 40 years with patients older than 40 years.
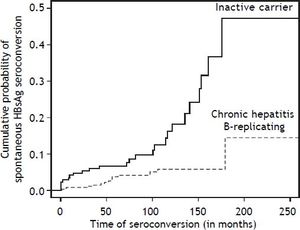
Regarding the evolutionary forms of the diseases, inactive HBV carriers presented a significantly greater probability of spontaneous HBsAg seroclearance than patients with chronic replicating hepatitis B. The cumulative probabilities of spontaneous HB-sAg seroclearance were 7.0, 11.0 and 47.0% after 50, 100 and 180 months of follow-up for inactive HBV carriers, respectively, and were 3.0, 6.0 and 14%, respectively, for patients with chronic replicating hepatitis B (p = 0.000191). The cumulative probabilities of spontaneous HBsAg seroclearance according to the evolutionary form of the disease are presented in figure 4.
Cumulative probability of spontaneous HBsAg seroconversion in patients with chronic HBV infection followed at the outpatient clinics of Hepatitis and Gastroenterology of HCFMRP from January 1992 to September 2008 according to the form of disease progression. * p = 0.000191 comparing inactive carrier with chronic hepatitis B replicating.
After a mean follow-up period of 86.25 months, serum anti-HBsAg became detectable (> 10 IU) in 29 (72.5%) patients who progressed to spontaneous HBsAg seroclearance, 18 of whom (62.0%) were inactive HBV carriers.
DiscussionThis study was conducted at HCFMRP-USP, which is considered to be the main tertiary referral center in the Ribeirão Preto region, covering 26 municipalities with an estimated population of 1,130,000 inhabitants. The patient series was of an impressive size, consisting of 548 patients who were evaluated for the occurrence of spontaneous HBsAg seroclearance and of the factors related to this event over a period of 15 years and 9 months, thus providing better knowledge of the evolutionary aspects of the infection. We observed an annual rate of spontaneous HBsAg seroclearance of 0.7%.
Most of the studies regarding spontaneous HBsAg seroconversion are conducted in endemic areas for HBV infection, where the infection is usually acquired during the perinatal period or in early infancy. In a country of continental dimensions such as Brazil, where most regions, except for the western Amazon region and the western part of the states of Santa Catarina and Paraná, have low or intermediate patterns of endemicity, this aspect of the natural history of chronic HBV infection has been barely studied.
Spontaneous HBsAg seroclearance is associated with a good prognosis, including improved liver injury and function, and increased long-term survival.21,27 However, spontaneous seroclearance occurs in a small proportion of patients during the natural history of chronic HBV infection.
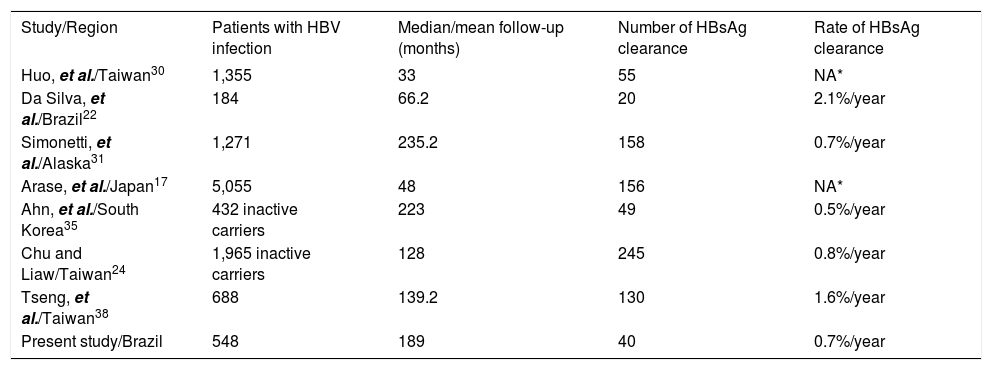
Spontaneous HBsAg seroclearance rates vary from 0.50 to 2.26% per year depending on the cohort group studied and the inclusion criteria. An annual rate of 0.1 to 0.8% and of 0.4 to 2% has been found in areas of high24,25,27–30 and low prevalence,22,23 respectively. A study from Alaska showed an annual rate of spontaneous HBsAg seroconversion of 0.5%, which is considered to be relatively low and can be explained by the inclusion of patients regardless of HBeAg status, a factor associated with HBsAg seroconversion.29 A study from Taiwan 24 that evaluated only inactive carriers of HBV showed an annual rate of HBsAg seroconversion of 1.15%; however, it should be noted that the mean patient age was much younger than ours. Conversely, in a study from South Korea, which included older patients (mean age of 50 years), a higher annual HB-sAg-seroclearance rate (2.69%) than that observed in our study was reported. In a Brazilian study where a group of 184 patients were followed up for 66.2 months, the annual rate of spontaneous HBsAg seroclearance was 2.1%.22Table 3 shows studies reporting spontaneous HBsAg clearance in patients with chronic HBV infection in different populations.
Studies reporting spontaneous HBsAg clearance in patients with chronic HBV infection in different populations.
| Study/Region | Patients with HBV infection | Median/mean follow-up (months) | Number of HBsAg clearance | Rate of HBsAg clearance |
|---|---|---|---|---|
| Huo, et al./Taiwan30 | 1,355 | 33 | 55 | NA* |
| Da Silva, et al./Brazil22 | 184 | 66.2 | 20 | 2.1%/year |
| Simonetti, et al./Alaska31 | 1,271 | 235.2 | 158 | 0.7%/year |
| Arase, et al./Japan17 | 5,055 | 48 | 156 | NA* |
| Ahn, et al./South Korea35 | 432 inactive carriers | 223 | 49 | 0.5%/year |
| Chu and Liaw/Taiwan24 | 1,965 inactive carriers | 128 | 245 | 0.8%/year |
| Tseng, et al./Taiwan38 | 688 | 139.2 | 130 | 1.6%/year |
| Present study/Brazil | 548 | 189 | 40 | 0.7%/year |
Long-term follow-up studies have shown excellent intrahepatic viral clearance and low viral replication activity, along with a drastic reduction in the risk of developing liver cirrhosis and HCC among the patients who seroconvert HBsAg, especially when this event occurs before 50 years of age.31,32
Previous studies have reported that the prognosis after spontaneous HBsAg seroclearance is excellent, except for patients with liver cirrhosis or concomitant infection with other types of viral hepatitis before spontaneous HBsAg seroclearance.17,18,24,33–35 Alternatively, the detection of HCC after spontaneous HBsAg seroclearance has been detected in some cases, especially in individuals with a diagnosis of liver cirrhosis prior to spontaneous HBsAg seroclearance.31,32,36,37
None of the present patients who achieved spontaneous HBsAg seroclearance showed any evidence of liver cirrhosis on the occasion of the event or during follow-up. Similarly, in the present study, HCC did not arise in any of the patients who achieved spontaneous HBsAg seroclearance. This result can most likely be explained by the absence of patients with advanced liver disease in the group that achieved spontaneous HBsAg seroclearance. Analyses of the present data and of those reported in different studies, where complications of hepatic disease did not occur in the absence of liver cirrhosis at the time of spontaneous HBsAg seroclearance, support the long-term good prognosis of this condition.
Some reports have demonstrated that serum HBV-DNA levels at the beginning of the study and during follow-up were the most significant indicators of spontaneous HBsAg seroclearance.21,28,38 These authors observed that most of the patients who experienced spontaneous HBsAg seroclearance had undetectable HBV-DNA levels before seroconversion.
Similarly, in the present study, we observed that low HBV-DNA levels were associated with the occurrence of spontaneous HBsAg seroclearance. Additionally, inactive HBV carriers had a greater probability of spontaneous HBsAg seroclearance than patients with chronic replicating hepatitis B. Thus, these data support the idea that a low viral load is an important factor for spontaneous HBsAg seroclearance in addition to having significant clinical implications for the prognosis of chronic hepatitis B.
Additionally, regarding viral factors possibly related to spontaneous HBsAg seroclearance, it has been demonstrated that individuals infected with genotype B of HBV have a greater probability of HB-sAg seroconversion than individuals infected with genotype C.21,39 However, the reasons for this occurrence have not been fully clarified. As mentioned earlier, data regarding the HBV genotype were not available for our patients.
Recent studies have shown that the level of HB-sAg is the most reliable factor for predicting spontaneous HBsAg seroconversion.38,40,41 In a study from Japan, which followed up 423 patients for a period of 23 years, spontaneous HBsAg seroconversion was observed in 25 patients with an incidence rate of 0.97% per year. In this study, the only predictive factor for HBsAg seroclearance was serum HBsAg titer at baseline.40 Tseng, et al. demonstrated thata lower serum HBsAg level was found to be associated with a higher rate of HBsAg loss and that a HBsAg level < 10 IU/mL immensely increased the likelihood of HBsAg loss.38 Despite evidence on the role of low levels of HBsAg for predicting the occurrence of spontaneous HBsAg seroconversion, our patients did not have HBsAg evaluated.
Another aspect of the present study was that males with chronic HBV infection were more likely than females to experience spontaneous HBsAg seroclearance, although the difference was not statistically significant. Liu, et al. and Liaw, et al. demonstrated a significant greater probability of spontaneous HBsAg seroclearance among males.25,28 Another important aspect regarding sex is the greater probability of recurrence of HBV infection in males.24 Thus, the present study, among others, demonstrates a possible relationship between spontaneous HBsAg seroclearance and male sex. However, the role of genetic or hormonal factors remains unknown.
Analysis of the present data showed that the peak incidence of spontaneous HBsAg seroclearance occurred between the fourth and fifth decade of life, and after 40 years of age in 67.5% of cases. Despite the small population studied here, these data suggest that, among patients with chronic HBV who are younger at the beginning of follow-up, the occurrence of spontaneous HBsAg seroclearance is relatively uncommon during the first years of follow-up, increasing with time, especially after the fourth decade of life.
Some limitations of the present study should be addressed. This was a retrospective study whose data originated from the routine medical follow-up of a tertiary referral hospital and some data were not available, such as HBV genotype. Moreover, the series of patients who progressed to spontaneous HBsAg seroclearance was small. However, despite these limitations, a study that considers spontaneous HBsAg seroclearance in an area of low prevalence of chronic HBV infection permits a better knowledge of this aspect in chronic HBV infection.
In conclusion, spontaneous HBsAg seroclearance represents a favorable clinical condition and was observed in 7.2% of patients in this study, with an estimated 0.7% annual incidence during a period of 15 years and 9 months. The occurrence of spontaneous HBsAg seroclearance was associated with low levels of HBV-DNA and apatient age higher than 40 years. This rate was similar to that reported for areas with alow prevalence of chronic HBV infection.
Conflict of InterestThe authors have declared no conflicting interests.
AcknowledgementsThis research was supported by Fundação de Apoio ao Ensino Pesquisa e Assistência (FAEPA), University Hospital, Faculty of Medicine Ribeirão Preto, University São Paulo (HCFMRP-USP). We wish to thank the staff of the Hepatitis Outpatient Clinic and the group of Clinical and Surgical Hepatology of HCFMRP-USP.