A 40-year old woman presented with symptomatic intrahepatic gallstones in one liver segment only four years after cholecystectomy for cholelithiasis. Multiple small, yellow and round calculi were completely removed from the intrahepatic bile ducts via ERCP. The young age of the patient, recurrence of gallstones after cholecystectomy and intrahepatic gallstones suggested a subtype of the low-phospholipid associated cholelithiasis syndrome, a monogenic form of cholesterol cholelithiasis due to variations of the ABCB4 gene that encodes the canalicular phospholipid transporter MDR3.
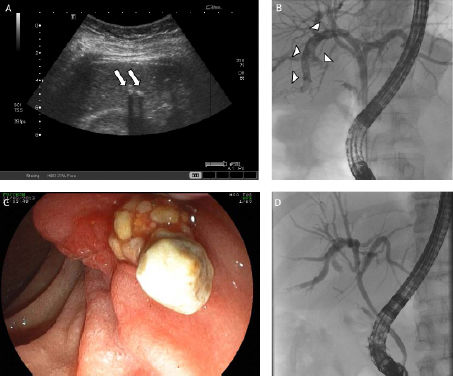
A 40-year old woman presented to our emergency department due to recurrent abdominal pain in the right upper quadrant with no fever or jaundice consistent with biliary colics. A cholecystectomy for symptomatic cholecystolithiasis was performed four years previously. Besides hypothyroidism, the past medical history was unremarkable. Physical exam revealed adiposity grade 1 (BMI 32) and tenderness in the right upper quadrant. Liver function tests (ASAT, ALAT, GGT, AP, total bilirubin) were slightly elevated. Abdominal ultrasound showed multiple small hyperechoic foci with complete acoustic shadows in the ventral segments of the right liver lobe (Figure 1A, arrows). These finding were confirmed on MRCP (not shown). For removal of symptomatic intrahepatic gallstones, an ERCP was performed (Figure 1B). The cholangiogram showed trifurcation of the hilus and confirmed dilatation of the bile ducts filled with multiple intraductalar small calculi in liver segment V only (Figure 1B, arrowheads). Employing dormia baskets and stone extraction balloons, gallstones were removed from the intrahepatic bile ducts. Gross appearance of multiple small, round, white to yellowish calculi suggested cholesterol gallstones (Figure 1C). Finally, following repeated ERCPs, the intrahepatic gallstones were completely removed (Figure 1D). The patient’s symptoms revolved.
Abdominal ultrasound showed multiple small hyperechoic foci (Figure A, arrows). The cholangiogram showed trifurcation of the hilus and confirmed dilatation of the bile ducts filled with multiple small gallstones (B, arrowheads). C. Multiple small, round and yellow calculi consistent with intrahepatic cholesterol gallstones were removed from the intrahepatic bile ducts via ERCP. D. Cholangiogram after complete removal of intrahepatic gallstones.
The location of the calculi in this patient suggested primary intrahepatic cholesterol gallstones rather than secondary intrahepatic stones due to migration from the gallbladder. Variation of the anatomy of the bile ducts as a cause for intrahepatic cholelithiasis is controversial. However, some authors explain the predominance of intrahepatic gallstones in the left liver lobe with impaired bile flow due to the acute angle of the left hepatic duct. In our case, trifurcation of the hilus with an arcuated course of the segmental duct may have predisposed to primary intrahepatic stone formation in liver segment V only.
The young age of the patient with cholelithiasis, recurrence of symptoms after cholecystectomy and intrahepatic calculi suggested the low phospholipid associated cholelithiasis (LPAC) syndrome.1 Intrahepatic bile ducts filled with gallstones but no stricture as we found in our patient was recently described as one phenotype of the LPAC syndrome.2 In patients with LPAC, the presumed low phospholipid concentration in bile is due to mutations of the ABCB4 gene that encodes the phospholipid transporter MDR3 that is located on the canalicular membrane of hepatocytes and transport phospholipids into bile. In this patient, we did not examine bile under the polarizing light microscope, measure phospholipid content in bile or, to date, sequence the ABCB4 gene. However, in this subtype of the LPAC syndrome ursodeoxycholic acid was reported to be beneficial and we recommended therapy with ursodeoxycholic acid (1,000 mg/day) for dissolution of remaining microliths and prevention of recurrent disease.