Bleeding varices at the stomal site is an uncommon complication of ileal conduit urinary diversion in patients with portal hypertension. We describe a case with the longest delay reported in the literature, involving the onset of massive hematuria secondary to ectopic variceal bleeding in an alcoholic cirrhotic patient with external urinary ileal conduit.
Peristomal varices in cirrhotic patients with ileal conduit urinary diversion after radical cystectomy represent ectopic portosystemic shunts. Their bleeding is a very rare but life-threatening complication. Many treatments have been proposed, with various recurrence rates.
Case ReportA 60-year-old man, who had undergone cystoprostatectomy with ileal conduit urinary diversion for invasive bladder cancer 16 years previously (1991) and partial hepatectomy for hepatocellular carcinoma in chronic alcoholic cirrhosis 2 years later (1993), presented with episodes of massive spontaneous urostomal gross hematuria (2007).
The patient had been treated with vasoactive drugs (beta-blocker therapy) and sclerotherapy (three times from 2002 and 2003) for esophageal variceal bleeding due to varices. The severity of cirrhosis at the moment of bleeding was Child-Pugh class B7 and MELD score 14, respectively, with a hepatic venous gradient (HVPG) of 18.1 mm/Hg.
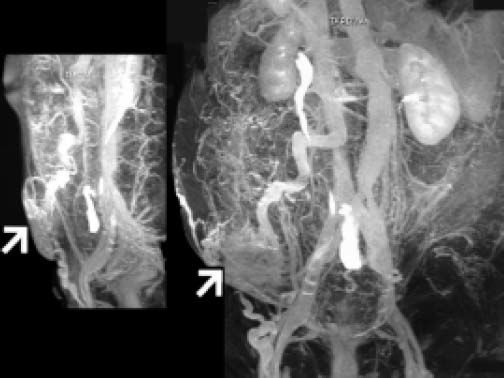
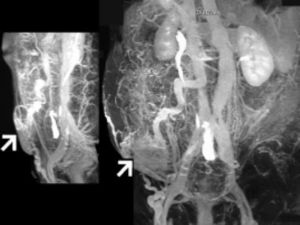
CT angiography performed during urostomal bleeding revealed large dilation of the portal vein and superior mesenteric vein, with a rich system of collateral veins at the level of the ileal conduit (Figure 1).
Due to the severity of acute bleeding, the patient was successfully treated with an emergency transjugular intrahepatic portosystemic shunt (2007). He survived without episodes of bleeding for 5 years before his death from neoplastic causes in 2012.
The initial factor in the pathophysiology of portal hypertension is known to be increased vascular resistance to portal blood flow. The increase in both blood pressure and flow in the portal veins explains why portal hypertension exists, despite the formation of an extensive network of portosystemic collaterals. Increased portal pressure contributes to the formation of ectopic varices. Fewer than 5% of patients with portal hypertension present intestinal varices.1,2 Rupture and consequent hemorrhage occur when the tension of the varices exceeds the elastic limits of the variceal wall. The development of ectopic varices and their further bleeding, due to cirrhosis and portal hypertension, are a rare cause of hematuria in patients with surgically augmented bladder volume or urinary diversion.3,4
Bleeding stomal varices in patients with ileostomy and portal hypertension were described by Resnick in 1968,5 but the first description of variceal bleeding in an urinary ileal conduit was reported only in 1975 by Foulkes and Wallace.6
One review reported that the average time from the creation of ileal conduit urinary diversion to the development of ectopic varices and consequent bleeding is 38 months.7 The period of 167 months with urinary ileal conduit before stomal variceal bleeding recorded in our case is, to our knowledge, the longest delay of a similar complication reported in the literature.
Proper diagnosis requires careful inspection of the muco-cutaneous region of the stoma and endoscopic examination of the ileal conduit. However, reconstruction of portal-phase CT angiograms enhances perception of the courses and anatomic relationships of varices. In our case, by precisely demonstrating the courses of ileal varices, CT angiography allows the surgeon to plan the operative approach.8
Emergency treatment of bleeding may involve several methods, such as local compression (i.e., a Foley catheter is introduced into the ileal conduit) or sclerotherapy. In our case, because of the severity of acute bleeding, a transjugular intrahepatic portosystemic shunt procedure was successfully emplaced.
Financial Support/Conflict of InterestI have no financial support and no conflict of interest to disclose.