Chronic liver disease may involve the lung through abnormal communications between the portal and pulmonary veins or by changes in the lungs caused by similar biochemical abnormalities to those in liver parenchyma. Lymphocytic interstitial pneumonitis(LIP) is more common in women and is associated with autoimmune diseases. Chest x-ray findings include reticular or reticulonodular opacities while computed tomography (CT) usually shows subpleural fibrosis (predominately in basal areas), ground-glass attenuation, traction bronchiectases and pulmonary parenchymal cysts.
A 35 year-old-man, heavy smoker (20 pack/years), presented with facial rash, jaundice, nausea and vomiting.
His initial investigations included liver function tests (LFTs) which showed ALT: 1721 IU/L & AST: 752 IU/L (normal range: 0-40), ALP: 124 IU/L (normal range: 39-118) & bilirubin: 241 mmol/L (normal range: 0-17). He used to drink only on special occasions and he had never used over-the-counter, herbal or homeopathic medicines.
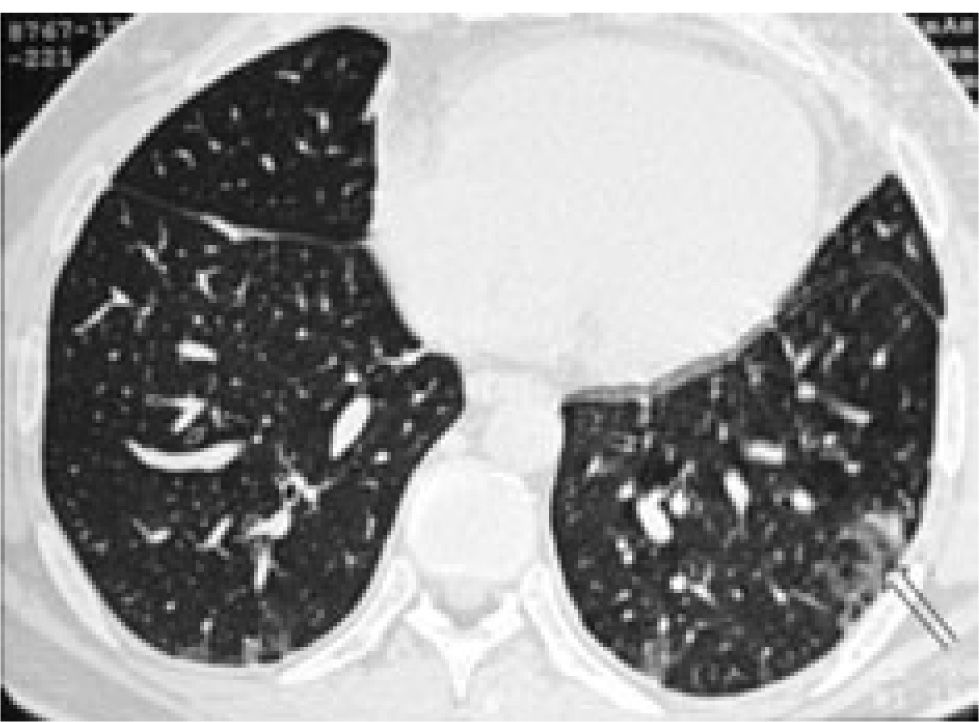
He had positive double stranded anti-DNA (ds-DNA) at 39 RU/mL (normal range: 0-20), positive anti-smooth muscle antibody (ASMA) with titre 1:160 and positive anti-nuclear antibody (ANA) with titre 1:40. His anti-mitochondrial antibodies (AMA) were negative and his Im-munoglobulin G (IgG) was raised only marginally at 17.2 (normal range: 6.0-15.0). A liver biopsy was obtained & showed changes of interface hepatitis with lobular necrosis, cholestasis and pericellular fibrosis while, in the portal tract edges non-caseating granulomas and lymphoid aggregates were present. Due to complaints of chest pain - on a follow-up examination-, a chest radiograph was requested (Figure 1) This x-ray was repeated one month later (Figure 2), while his CT scan findings are shown in figure 3.
The diagnosis of autoimmune hepatitis complicated by lymphocytic interstitial pneumonitis was made and after a detailed but negative septic screen the patient was started on prednisone and later on azathioprine and showed remarkable improvement of both the liver biochemistry and long-lasting resolution of his radiographic findings.
Chronic liver disease may involve the lung through abnormal communications between the portal and pulmonary veins or by changes in the lungs caused by similar biochemical abnormalities to those in liver parenchyma. They manifest morphologically in the form of lymphocytic interstitial pneumonitis (LIP). Fibrosing alveolitis, bronchiolitis obliterans and pleurisy are amongst other recorded pulmonary associations of autoimmune hepatitis.1,2
Although our diagnosis was not conformed by histology, we can assume with certainty that, the observed pulmonary infiltrates were due to LIP. This is supported by the characteristic radiographic findings & the marked improvement after treatment with corticosteroids and azathioprine.
LIP is more common in women (average age 55 years) and it has been associated with autoimmune diseases, pulmonary infections, immunodeficiency, serum dysproteinaemias and drug reactions and graft vs host disease (GVHD). Symptoms mostly consist of chronic cough, dyspnoea, weight loss, fatigue and rarely fever while, haemoptysis or chest pain can occur. Few patients (< 4%) are asymptomatic on presentation. Chest x-ray findings include reticular or reticulonodular opacities and to a lesser extend hilar lymphadenopathy, pleural effusions and honeycomb appearance (from extended fibrosis).4,6 High resolution Ctscan images typically show subpleural fibrosis (predominately in basal areas), ground-glass attenuation, traction bronchiectasis and pulmonary parenchymal cysts.3,5
On blood gas analysis, partial oxygen pressure (PO2) is normal or decreased and alveolar-arterial oxygen gradient (A-a gradient) increased. Bronchoalveolar lavage may reveal increased number of lymphocytes. Spirometry usually shows a restrictive pattern with reduced or normal lung volumes and decreased carbon monoxide diffusing capacity.
Diagnosis is confirmed, where possible, with histology examination of biopsy specimens obtained either by bronchoscopy or open lung biopsy. Patients with respiratory distress require therapy with corticosteroids and/or immunosuppressive drugs. Approximately half of patients improve with treatment but relapses are common and disease progression may occur despite successful treatment and initial clinical response.
The clinical course of LIP is variable. Spontaneous resolution, even without treatment, as well as progression to pulmonary fibrosis and/or malignant transformation to lymphoma (less than 5%) -despite immunosuppression-must be expected. Older patients have increased mortality (40-50% in 5 years) if complicated disease (recurrent pulmonary infections, respiratory failure) is encountered.