The term minimal hepatic encephalopathy (MHE) refers to the subtle changes in cognitive function, electrophysiological parameters, cerebral neurochemical/neurotransmitter homeostasis, cerebral blood flow, metabolism, and fluid homeostasis that can be observed in patients with cirrhosis who have no clinical evidence of hepatic encephalopathy; the prevalence is as high as 84% in patients with hepatic cirrhosis. Physician does generally not perceive cirrhosis complications, and neuropsychological tests and another especial measurement like evoked potentials and image studies like positron emission tomography can only make diagnosis. Diagnosis of minimal hepatic encephalopathy may have prognostic and therapeutic implications in cirrhotic patients. The present review pretends to explore the clinic, therapeutic, diagnosis and prognostic aspects of this complication.
Nearly 2,500 years ago, Hippocrates (460-370 B.C.) observed that “those who are mad on account of phlegm are quiet, but those on account of bile are vociferous, vicious, and do not keep quiet”; it can thus be assumed that he was the first to make an association between hepatic disease and impaired brain function.1
It is well recognized that patients with cirrhosis or chronic hepatic disease develop neurocognitive impairment, characterized by manifestations that vary from subtle to severe enough to limit functional operability. This impairment increases morbidity and mortality and progresses to hepatic encephalopathy (HE).2-6
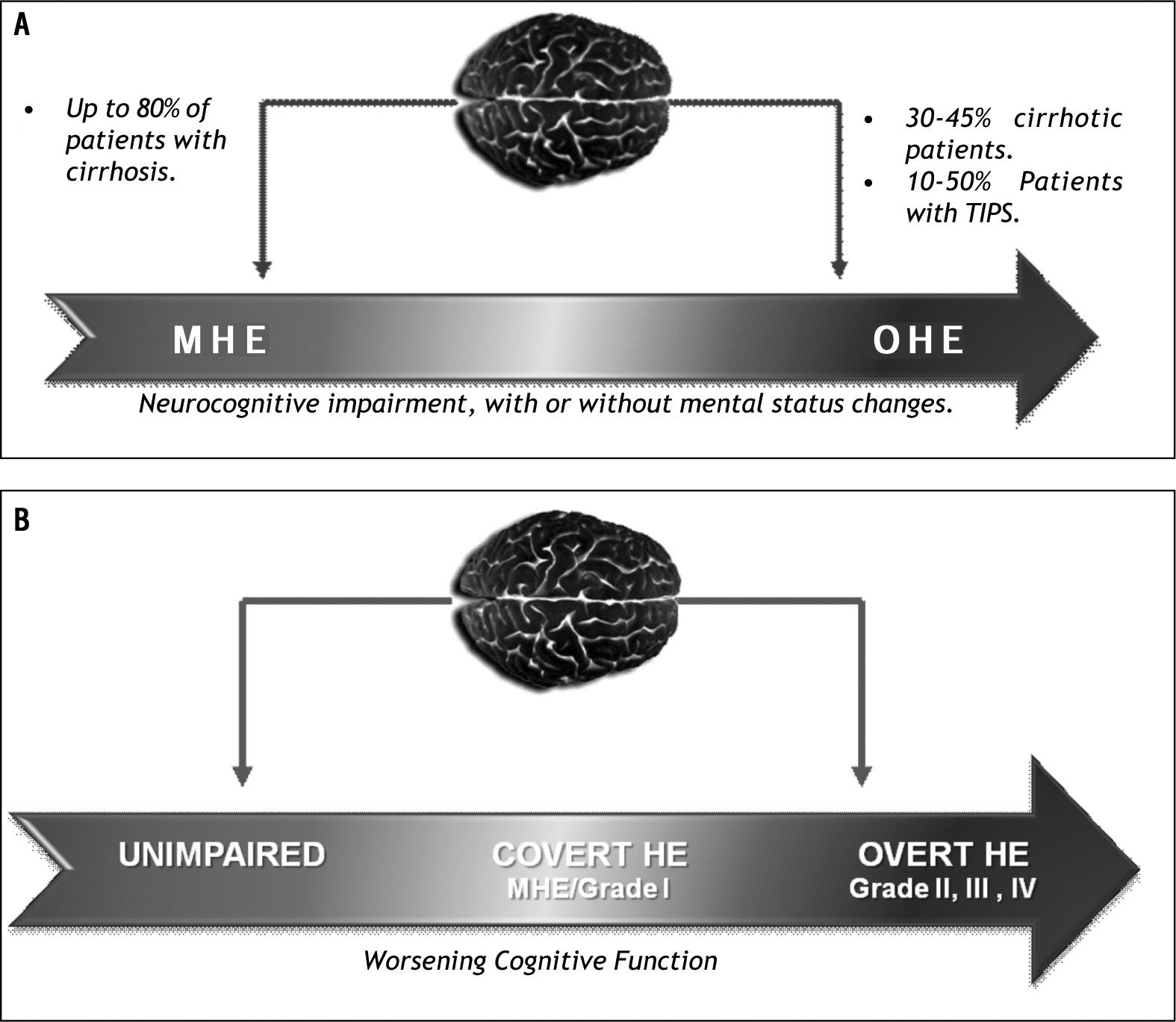
HE causes various neuropsychiatric disturbances, ranging from a spectrum of subtle abnormalities apparent only as impaired mental status to coma. It develops in patients with cirrhosis, acute hepatic failure and portacaval shunts, and is reversible, provided that other cerebral effects have been excluded. It is important to note that the changes observed in HE constitute a continuum known as the spectrum of neurocognitive impairment in cirrhosis (SONIC)2,7,8 (Figure 1).
Spectrum of neurocognitive abnormalities in cirrhosis. MHE: Minimal hepatic encephalopathy. OHE: Overt hepatic encephalopathy. Source: Adapted from Butterworth, RF.(34)B. Spectrum of neuro-cognitive impairment in cirrhosis (SONIC). Adapted from Bajaj JS, Cordoba J, Mullen KD, Amodio P, Shawcross DL, Butterworth RF, Morgan MY. Review article: the design of clinical trials in hepatic encephalopathy-an International Society for Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN) consensus statement. Aliment Pharmacol Ther 2011; 33: 739-47.(35)
The various neuropsychiatric abnormalities associated with hepatic cirrhosis may be present even in the absence of clinical data. Therefore, neuropsychological assessment is necessary for the diagnosis of the early and mildest form of HE, known as minimal hepatic encephalopathy (MHE).9
MHE is considered as neuropsychiatric syndrome with a wide range of cognitive and psychomotor deficits coexistent with hepatic function impairment and portal-systemic shunting. If patients with MHE have no recognizable clinical symptoms of HE, neuropsychometric methods or neurophysiological variables are needed for its diagnosis.10-12
MHE was previously described using terms such as “subclinical”, “latent”, “early”, “low-grade” and “grade 0”; however, these terms lead clinicians to imply a lack of clinical significance for its diagnosis. Hence, recent studies favor the term “minimal hepatic encephalopathy”, coined by the Working Party of the World Gastroenterology Organization at the 11th World Congress of Gastroenterology in Vienna.10
DiagnosisSeveral studies have tried to characterize MHE. However, data on the involvement of subcortical circuits are conflicting, because neurocognitive abnormalities primarily affect attention, speed of information processing, hearing capacity, motor abilities and coordination, even though intellectual processing is preserved.13
Traditionally the West Haven Criteria is used by the classification of overt HE, but are not subtle enough to diagnose MHE. Therefore, the MHE population would benefit from a diagnostic approach that is broader and more precise than neuropsychiatric status assessment, and that includes the following:8,14,15
- •
Inquiries about changes in activities of daily living such as appetite, sleep, energy, activities and quality of life.
- •
Inquiries about changes in mental status, such as memory, concentration, cognition and consciousness.
- •
Evaluation of mental status using the Mini Mental Test.
- •
A neurological examination with a specific focus on subtle motor abnormalities, such as hypomimia, speech disturbances, increased muscle tone, dysdiadochokinetic movements, ataxic gait, increased tendon reflexes and postural reflexes, and motor disorders such as flapping tremor, specifically asterixis (the presence of sensorial findings or focal abnormalities may suggest another diagnosis)
- •
Exclusion of other neurological abnormalities such as subdural hematoma and Wernicke’s encephalopathy, and metabolic disturbances such as diabetes, renal insufficiency and acute intoxication with drugs or alcohol.
Currently, there is no consensus on how to diagnose MHE. However, the following requisites are needed to establish the diagnosis:
- •
Presence of a disease that can cause MHE, such as cirrhosis or portosystemic shunts.
- •
Normal mental status on clinical examination.
- •
Demonstration of cognitive abnormalities, assessed using any of the following methods (Table 1):
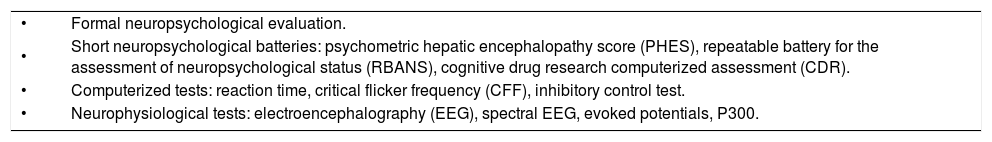
Table 1.Diagnostic methods for MHE.
• Formal neuropsychological evaluation. • Short neuropsychological batteries: psychometric hepatic encephalopathy score (PHES), repeatable battery for the assessment of neuropsychological status (RBANS), cognitive drug research computerized assessment (CDR). • Computerized tests: reaction time, critical flicker frequency (CFF), inhibitory control test. • Neurophysiological tests: electroencephalography (EEG), spectral EEG, evoked potentials, P300. Abnormal functional or structural images of the central nervous system obtained by PET scanning, magnetic resonance imaging or magnetic resonance spec- troscopy are not considered diagnostic of MHE.
Adapted from Ortiz M, Jacas C, Córdoba J. Minimal hepatic encephalopathy: diagnosis, clinical significance and recommendations. J Hepatol 2005; 42: S45-S53.
- °
Formal neuropsychological evaluation.
- °
Short neuropsychological batteries.
- °
Computerized tests.
- °
Neurophysiological tests.
- •
Exclusion of concomitant neurological disorders.
Formal neuropsychological evaluation demonstrates cognitive deficits and enables the diagnosis of MHE. However, this tool cannot be widely used because it is expensive, time consuming and subjective, and must be conducted by an expert examiner.
Among the short neuropsychological batteries, the psychometric hepatic encephalopathy score (PHES) is the best typified and the only battery specifically developed for diagnosis of MHE.16 The PHES combines five paper-pencil tests that assess motor speed and accuracy, visuospatial orientation, visual perception, concentration, attention and memory. The test takes about 20 min to complete, and has a sensibility and specificity of 96 and 100%, respectively,17 for differentiating patients with HE. The tests included in this battery are the digit symbol test, number connection tests A and B, the serial dotting test and the line tracing test.
At the 11th World Congress of Gastroenterology in 1998, the use of at least two of these tests was recommended for the diagnosis of MHE.
The vast majority of computerized tests assess speed of mental processing (reaction time), accuracy and various cognitive domains. Examples of these tests are the CFF test, the inhibitory control test and reaction time. These tests are reproducible, easy to apply, objective and not operator dependent.
Several clinical studies have assessed CFF as a diagnostic tool for MHE and compared it with psychometric (PHES) and neuropsychological tests. The studies found concordance in MHE diagnosis and that the CFF has a sensibility of 55-96% and a specificity of 77-100%.18-20
The psychopathological basis for the use of CFF for cirrhotic patients is that similar changes to those observed in astrocytes during HE occur in the retina, called hepatic retinopathy, in which retinal glial Müller cells mimic changes similar to those in Alzheimer type II astrocytes. Retinal gliopathy is therefore considered a marker of cerebral gliopathy in MHE.
Neurophysiological tests assess cerebral electrical activity as manifested in brain waves (electroencephalography) or the discrete firing patterns of neuronal activation (evoked potential techniques, transcranial magnetic stimulation). The main advantage of these types of tests is that they are objective, reproducible and independent of age, sex or education. These tests include electroencephalography (EEG), spectral EEG, evoked visual potentials and cognitive potentials (P300).14-17
According to the recommendations of the International Society on Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN), the neuropsychological batteries, PHES and RBANS, have been proposed for consideration as gold standards for the diagnosis of MHE because they are used as assessing tools and diagnostic methods. They enable evaluation of cognitive function and neuropsychological abnormalities in a simple, fast and economic way, and do not require special expertise to perform. However, as with formal neuropsychological evaluation, the results are subjective and dependent on sociodemographic variables (age, education, nationality), making the standardization of these tests necessary, as has been done in Germany, Spain, Italy, the UK, India and Mexico.16,21-26
PrevalenceAs the prevalence of MHE among cirrhotic patients ranges from 20% to 84%,27,28 some authors consider it an “epidemic" pathology.29 This wide range in MHE prevalence is because of differences in definition, lack of standardized diagnostic criteria, differences in diagnostic methods (type of test used), the clinical-pathological-comorbid spectrum and sociodemographic variables.
MHE has been associated with hepatic cirrhosis for more than 30 years, and it was observed recently observed that neurocognitive abnormalities similar to those observed in hepatic disease are present in the context of portal hypertension without hepatic function impairment.30
Although there is a low prevalence of MHE in cirrhotic patients with Child-Pugh A scores (less than 15%), the prevalence is 50% in patients with Child-Pugh B/C scores; however, these figures are derived from studies in which Child-Pugh classifications were not correlated with MHE.18,27,32
Other factors that have been associated with MHE are age, alcohol etiology, surgical or transjugular portosystemic shunting, previous episodes of HE and esophageal varices.
There are few reports of the prevalence of MHE in Mexico. In one study, conducted in patients with primary biliary cirrhosis (PBC), the prevalence of MHE was 22%.33