Introduction. Recurrent biliary obstruction necessitating premature repeat endoscopic retrograde pancreatography (ERCP) remains a costly and morbid problem in patients undergoing treatment of post-or-thotopic liver transplantation (OLT) biliary strictures. We evaluated the relationship between prednisone or sirolimus use and early recurrence of biliary obstruction given their negative effects on collagen production and cholangiocyte regeneration.
Methods. Medical records of adult patients who underwent OLT from 1998-2008 and developed anastomotic (ABS) and/or nonanastomotic (NABS) biliary strictures requiring endoscopic plastic stent therapy were reviewed. Outcome was early recurrence of biliary obstruction requiring repeat ERCP. Univariate and multivariable logistic regression analysis, adjusting for age, sex, and time from OLT to ERCP, were performed.
Results. 35 patients with ABS and 9 patients with NABS underwent a total of 157 ERCPs. Median patient age was 56 years, 68% were male, and hepatitis C was the most common OLT indication (52%). Early recurrence of biliary obstruction ocurred following 17.1% of ERCPs. In univariate analysis, neither prednisone nor sirolimus was associated with early recurrence of biliary obstruction. In multivariate analysis, however, sirolimus use was associated with increased incidence of early recurrent biliary obstruction (OR = 2.53; 95% CI: 0.77-8.32; p = 0.12); this was more pronounced at doses > 3 (OR = 4.27; 95% CI: 0.62-29.3; p = 0.14) than at ≤ 3 mg/day (OR = 2.24; 95% CI: 0.62-8.13; p = 0.22) and statistically significant in patients with ABS only (OR = 1.44 per mg increase in sirolimus dose; 95% CI 1.02-2.03; p = 0.037).
Conclusions. Sirolimus use, particularly at higher doses and patients with ABS, may be associated with an increased risk of early recurrence of biliary obstruction requiring repeat ERCP for post-OLT biliary strictures. Additional studies are needed to further investigate these findings and elucidate other risk factors.
Biliary strictures are a common complication after orthotopic liver transplantation (OLT), occurring in up to 17% of brain dead and 50% of donation after cardiac death (DCD) donor liver recipients despite improvements in organ procurement, preservation, and transplantation.1-3 In addition, they may be associated with substantial morbidity and costs in spite of considerable progress in therapeutic endoscopic techniques.2,4-10 While previous work has examined predictors of biliary stricture formation and of final endoscopic treatment outcome,2,3,7,8,11-15 to our knowledge no study has examined which variables may predispose to early recurrence of biliary obstruction and need for repeat endoscopic retrograde pancreatography (ERCP) in patients being treated for post-OLT biliary strictures.10
One such variable may be the immunosuppressive regimen. Two commonly used immunosuppressants in post-OLT patients are prednisone and sirolimus, both of which have negative effects on collagen production, angiogenesis, and/or cholangiocyte regeneration.16-19 These, in turn, may affect anastomotic healing as well as stricture remodeling and biliary flow. We performed an exploratory study of the relationships between prednisone or sirolimus use and the time to repeat ERCP due to recurrence of biliary obstruction in patients undergoing endoscopic treatment for post-OLT anastomotic (ABS) and nonanas-tomotic (NABS) biliary strictures.
MethodsThis study was approved by the Johns Hopkins School of Medicine institutional review board.
PatientsThe electronic medical records of the 461 adult patients who underwent OLT at Johns Hopkins Hospital between January 1998 and December 2008 were retrospectively reviewed for clinical, laboratory, and radiographic data, and patients with post-OLT ABS or NABS treated with endoscopically-placed plastic biliary stents were identified. Patients who received a livingdonor liver, Rouxen-Y choledochojejunostomy or hepaticojejunostomy, percutaneous instead of endoscopic stenting of biliary stricture, endoscopic therapy for reasons other than biliary stricture (i.e. biliary leaks), or endoscopic therapy without stenting were excluded.
All patients were initially on a triple-drug post-OLT immunosuppressive regimen consisting of tacrolimus or sirolimus, corticosteroid, and mycophenolate mofetil. The latter two medications were tapered off at approximately 3 months and 1 year after OLT, respectively. Patients were routinely followed with liver tests and/or clinic visits.
Post-OLT stricture diagnosis and managementPatients with abnormal liver biochemical tests and/or imaging demonstrating dilated intra- or extra-hepatic bile ducts with no alternative diagnosis (e.g. recurrent viral infection, allograft rejection, etc.) by clinical, laboratory, imaging and/or histological assessment underwent ERCP for evaluation. ABS was defined as a dominant narrowing at the anastomotic site without effective passage of contrast material, as defined by cholangiography.14 NABS was defined as an abrupt luminal narrowing or tapering of the intra and/or extrahepatic graft ducts proximal to the choledochocholedochal anastomosis with significant impairment of contrast flow.15 Ductal narrowing without proximal biliary dilatation or bile flow impairment was not sufficient for the diagnosis of ABS or NABS.
ERCPs were performed with a therapeutic side-viewing endoscope (TJF 160, Olympus America, Inc., Center Valley, PA) with patients in either the prone or supine position by one of eight staff endoscopists. Antibiotics were administered in the peri-procedural period in patients with suspected cholangitis.
A dome tip Tri-Tome PC with 30 mm cutting wire (Cook, Winston-Salem, NC) preloaded with a 0.035 inch, 450 cm guidewire (Jagwire, Boston Scientific, Natick, MA) was used to achieve biliary cannulation. Biliary sphincterotomy was performed using standard technique. Biliary balloon dilation as well as the size, length, and number of biliary stents inserted were at the discretion of the attending endoscopist. Balloon dilation was performed using a 4 mm, 6 mm, or 8 mm polyethylene terephthalate biliary balloon dilator (Conmed, Billerica, MA). The type of stent used was the Cotton-Huibregtse biliary stent (Cook, Winston-Salem, NC), 90% of which were 10 French (remainder 7 and 8.5 French). All but 4 patients had ≤ 2 stents placed at any given ERCP. Stent exchanges were routinely performed approximately every 3 months for up to one year or until the cholangiographic appearance of the strictures was improved over baseline with accompanying improvements in proximal ductal dilation and/or biochemical liver test abnormalities.
Outcome and variablesThe outcome of interest was incidence of early recurrence of biliary obstruction requiring premature repeat ERCP (hereinafter “early recurrent biliary obstruction”). This was defined as an unscheduled or emergent stent removal or exchange accompanied by any one of the following in the absence of an alternative diagnosis: fever, abdominal pain, new-onset jaundice, cholangitis, bile duct dilatation on ultrasound, computed tomography, or magnetic retrograde cholangiopancreatography, or elevated alkaline phosphatase (≥ 2x upper limit of normal or ≥ 1.5x value prior to stent insertion if that value was > 120 mg/dL).10
Variables evaluated as potential predictors of outcome were: prednisone use (any dose) at the time of ERCP, prednisone dose at the time of ERCP, sirolimus use (any dose) at the time of ERCP, and sirolimus dose at the time of ERCP. Age, sex, and time interval from OLT to ERCP were included as covariables in multivariate analysis. If the dose of immunosuppressant on the day of ERCP was not available, the dose used within 1 month prior to the ERCP was used.
Data analysisPatient and clinical characteristics were described as median (range) or proportions. Patient level clustering was taken into account in univariate and multivariable logistic regressions exploring the associations between prednisone or sirolimus and early recurrent biliary obstruction. Tests of significance were 2-tailed, with an alpha level of 0.05. Statistical analysis was performed using STATA 11.0 (Stata-Corp LP, College Station, Texas).
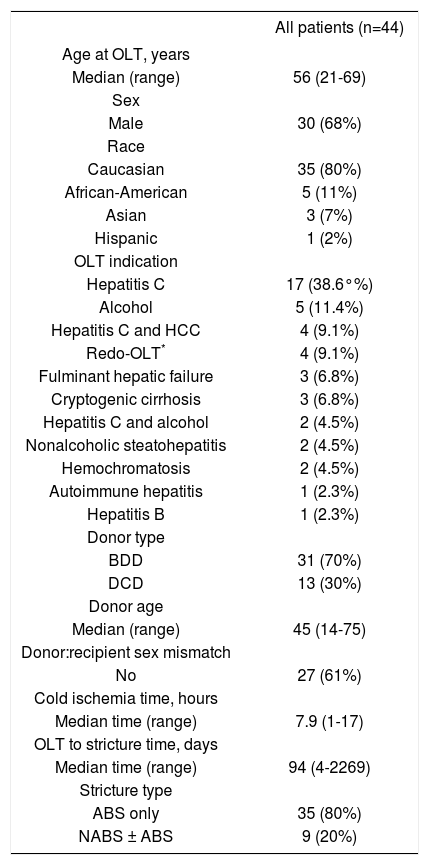
ResultsOf the 44 patients meeting inclusion criteria, 30 (68%) were male, and the median age was 56 years (range 21-69). The most common indication for OLT was hepatitis C infection (38.6%). Clinical characteristics are further summarized in table 1.
Clinical characteristics of sample.
| All patients (n=44) | |
|---|---|
| Age at OLT, years | |
| Median (range) | 56 (21-69) |
| Sex | |
| Male | 30 (68%) |
| Race | |
| Caucasian | 35 (80%) |
| African-American | 5 (11%) |
| Asian | 3 (7%) |
| Hispanic | 1 (2%) |
| OLT indication | |
| Hepatitis C | 17 (38.6°%) |
| Alcohol | 5 (11.4%) |
| Hepatitis C and HCC | 4 (9.1%) |
| Redo-OLT* | 4 (9.1%) |
| Fulminant hepatic failure | 3 (6.8%) |
| Cryptogenic cirrhosis | 3 (6.8%) |
| Hepatitis C and alcohol | 2 (4.5%) |
| Nonalcoholic steatohepatitis | 2 (4.5%) |
| Hemochromatosis | 2 (4.5%) |
| Autoimmune hepatitis | 1 (2.3%) |
| Hepatitis B | 1 (2.3%) |
| Donor type | |
| BDD | 31 (70%) |
| DCD | 13 (30%) |
| Donor age | |
| Median (range) | 45 (14-75) |
| Donor:recipient sex mismatch | |
| No | 27 (61%) |
| Cold ischemia time, hours | |
| Median time (range) | 7.9 (1-17) |
| OLT to stricture time, days | |
| Median time (range) | 94 (4-2269) |
| Stricture type | |
| ABS only | 35 (80%) |
| NABS ± ABS | 9 (20%) |
ABS: Anastomotic biliary stricture. BDD: Brain dead donor. DCD: Donation after cardiac death. HCC: Hepatocellular carcinoma. NABS: Nonanastomotic biliary stricture. OLT: Orthotopic liver transplantation.
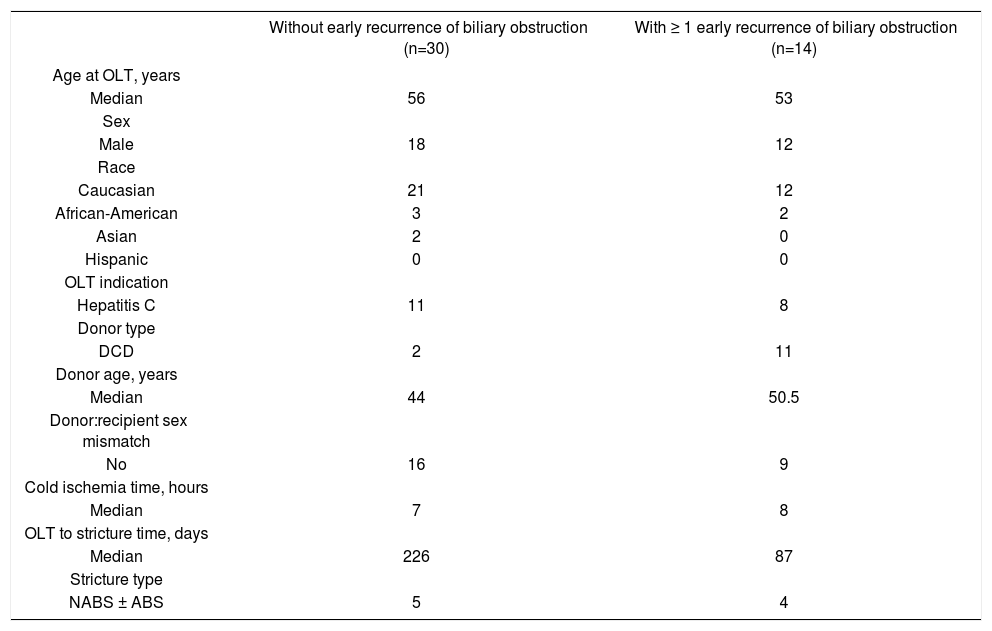
There were a total of 157 ERCPs with a median of 1 plastic biliary stent (range 1-4) inserted at each ERCP. Five ERCPs were excluded due to insufficient data on outcome. Of the remaining 152 ERCPs, 26 (17.1%) resulted in early recurrence of biliary obstruction (in a total of 14 patients) at a median of 49 days (inter-quartile range: 21-72 days). Clinical characteristics of patients with and without early recurrence of biliary obstruction are shown in table 2.
Characteristics of patients with and without early recurrence of biliary obstruction.
| Without early recurrence of biliary obstruction (n=30) | With ≥ 1 early recurrence of biliary obstruction (n=14) | |
|---|---|---|
| Age at OLT, years | ||
| Median | 56 | 53 |
| Sex | ||
| Male | 18 | 12 |
| Race | ||
| Caucasian | 21 | 12 |
| African-American | 3 | 2 |
| Asian | 2 | 0 |
| Hispanic | 0 | 0 |
| OLT indication | ||
| Hepatitis C | 11 | 8 |
| Donor type | ||
| DCD | 2 | 11 |
| Donor age, years | ||
| Median | 44 | 50.5 |
| Donor:recipient sex mismatch | ||
| No | 16 | 9 |
| Cold ischemia time, hours | ||
| Median | 7 | 8 |
| OLT to stricture time, days | ||
| Median | 226 | 87 |
| Stricture type | ||
| NABS ± ABS | 5 | 4 |
ABS: Anastomotic biliary stricture. DCD: Donation after cardiac death. NABS: Nonanastomotic biliary stricture. OLT: Orthotopic liver transplantation. *p<0.05 for difference between groups, Fisher’s exact test.
Seventy nine ERCPs were performed during prednisone use. Early recurrent biliary obstruction occurred in 20 (25%) of these, compared to 6 (8%) that were performed not during prednisone use. After considering patient level clustering, the unadjusted odds ratio (OR) for early recurrent biliary obstruction following ERCPs performed during prednisone use was 2.2 (95% confidence interval [CI]: 0.80 to 6.19; p = 0.13).
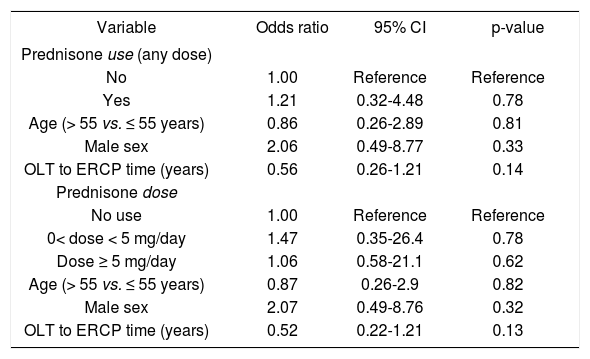
In the multivariable logistic regression model, we found that prednisone use was not statistically associated with early recurrent biliary obstruction (OR = 1.21; 95% CI: 0.32 to 4.48; p = 0.78). Higher pre-dnisone dose (≥ 5 mg/day)1 was also not associated with increased odds of early recurrent biliary obstruction (p for trend = 0.20).Table 3 shows these results in greater detail.
Multivariate analysis of association between prednisone and early recurrent biliary obstruction.
| Variable | Odds ratio | 95% CI | p-value |
|---|---|---|---|
| Prednisone use (any dose) | |||
| No | 1.00 | Reference | Reference |
| Yes | 1.21 | 0.32-4.48 | 0.78 |
| Age (> 55 vs. ≤ 55 years) | 0.86 | 0.26-2.89 | 0.81 |
| Male sex | 2.06 | 0.49-8.77 | 0.33 |
| OLT to ERCP time (years) | 0.56 | 0.26-1.21 | 0.14 |
| Prednisone dose | |||
| No use | 1.00 | Reference | Reference |
| 0< dose < 5 mg/day | 1.47 | 0.35-26.4 | 0.78 |
| Dose ≥ 5 mg/day | 1.06 | 0.58-21.1 | 0.62 |
| Age (> 55 vs. ≤ 55 years) | 0.87 | 0.26-2.9 | 0.82 |
| Male sex | 2.07 | 0.49-8.76 | 0.32 |
| OLT to ERCP time (years) | 0.52 | 0.22-1.21 | 0.13 |
CI: Confidence interval. ERCP: Endoscopic retrograde cholangiopancreatography. OLT: Orthotopic liver transplantation.
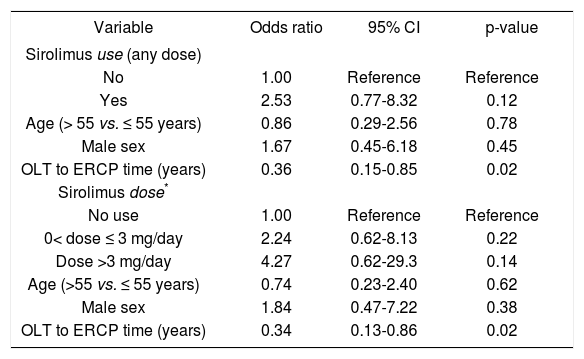
Fifty two ERCPs were performed during sirolimus use. Early recurrence of biliary obstruction occurred in 11 (21%) of these, compared to 15 (15%) that were performed not during sirolimus use. After considering patient level clustering, the unadjusted OR for early recurrent biliary obstruction following ERCPs performed during sirolimus use was 1.38 (95% CI: 0.48-3.99; p = 0.55).
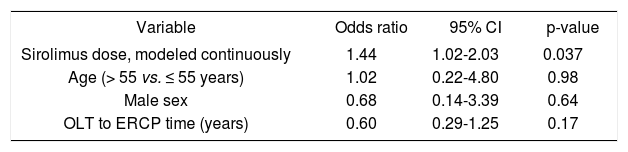
In the multivariable logistic regression model, we found that sirolimus use was associated with increased likelihood of early recurrent biliary obstruction, although this did not reach statistical significance. With respect to sirolimus dose (median = 3 mg/day, range 0.5-6), doses of ≤ 3 mg/day and > 3 mg/day were associated with ORs of 2.24 and 4.27, respectively (p for trend = 0.16), compared to no sirolimus use (Table 4). When dose was modeled continuously, the OR of early recurrent biliary obstruction was 1.34 per mg/day increase in sirolimus dose (95% CI 0.94-1.9; p = 0.10). Furthermore, after restricting analysis to only patients with ABS (35 patients, 127 ERCPs), this relationship was statistically significant, with an OR of 1.44 per mg/day increase in sirolimus dose (95% CI 1.02-2.03; p = 0.037), as shown in table 5.
Multivariate analysis of association between sirolimus and early recurrent biliary obstruction.
| Variable | Odds ratio | 95% CI | p-value |
|---|---|---|---|
| Sirolimus use (any dose) | |||
| No | 1.00 | Reference | Reference |
| Yes | 2.53 | 0.77-8.32 | 0.12 |
| Age (> 55 vs. ≤ 55 years) | 0.86 | 0.29-2.56 | 0.78 |
| Male sex | 1.67 | 0.45-6.18 | 0.45 |
| OLT to ERCP time (years) | 0.36 | 0.15-0.85 | 0.02 |
| Sirolimus dose* | |||
| No use | 1.00 | Reference | Reference |
| 0< dose ≤ 3 mg/day | 2.24 | 0.62-8.13 | 0.22 |
| Dose >3 mg/day | 4.27 | 0.62-29.3 | 0.14 |
| Age (>55 vs. ≤ 55 years) | 0.74 | 0.23-2.40 | 0.62 |
| Male sex | 1.84 | 0.47-7.22 | 0.38 |
| OLT to ERCP time (years) | 0.34 | 0.13-0.86 | 0.02 |
CI: Confidence interval. ERCP: Endoscopic retrograde cholangiopancreatography. OLT: Orthotopic liver transplantation.
Multivariate analysis of association between sirolimus dose and early recurrent biliary obstruction, anastomotic biliary stricture only.
| Variable | Odds ratio | 95% CI | p-value |
|---|---|---|---|
| Sirolimus dose, modeled continuously | 1.44 | 1.02-2.03 | 0.037 |
| Age (> 55 vs. ≤ 55 years) | 1.02 | 0.22-4.80 | 0.98 |
| Male sex | 0.68 | 0.14-3.39 | 0.64 |
| OLT to ERCP time (years) | 0.60 | 0.29-1.25 | 0.17 |
CI: Confidence interval. ERCP: Endoscopic retrograde cholangiopancreatography. OLT: Orthotopic liver transplantation.
The development and treatment of ABS and NABS continue to be a challenging long-term problem in OLT patients. Previous studies have examined factors associated with biliary stricture formation or with the ultimate endoscopic treatment outcome. However, little is known about which variables may affect the interval to development of recurrent biliary obstruction and need for repeat ERCP in this vulnerable population. This is particularly the case with regard to the role of immuno-suppressive regimens in such outcomes. In the present study, we explored this relationship and found that, after adjusting for other variables, sirolimus use showed a dose-dependent trend toward increased risk for early recurrent biliary obstruction and need for repeat ERCP, particularly in patients with ABS only. There may be several reasons for this association: sirolimus use may delay healing and increase or prolong the fragility of the choledo-chocholedochal anastomosis, as supported by the observation that the aforementioned trend persisted even after controlling for time from OLT to ERCP. This would render the anastomosis susceptible to traumatic injury and inflammation from manipulation during endoscopic treatment.
In turn, this may lead to biliary obstruction via impaired bile flow around the stent as a result of anastomotic edema. There may also be impaired bile flow through the stent as a result of changes in biliary fluid composition (e.g. more sludging, possibly altered bacterial flora with increased biofilm formation) related to the inflammatory milieu20 or in cases where there is distal migration of stent beyond the site of stricture. With the use of sirolimus becoming increasingly common in the evolving pharmacoscape of transplantation, its putative effects on biliary outcomes, as well as those of emerging drugs, merit additional research.
We found prednisone use to have a trend toward an association with early recurrent biliary obstruction in univariate analysis, but this association was not sustained after adjusting for age, sex, and time from OLT to ERCP. It has been hypothesized that in patients taking greater than 5 mg of prednisone per day, there may be a higher risk of anastomotic disruption as a result of endoscopic therapy, particularly balloon dilation;1 our findings may suggest that this increased risk could be a reflection of less time for anastomotic healing after OLT rather than the deleterious properties of prednisone. However, given the known effects of prednisone on wound healing, further investigation is warranted.
This study has several limitations. Sample size was small; this may have precluded certain variables from reaching statistical significance. In addition, it limited our ability to perform multivariate analysis for NABS, which may respond differently to immunosuppression and to endoscopic stenting than ABS. Loosening our exclusion criteria may have yielded a larger sample, although at the expense of having substantial sample heterogeneity. Our study design was retrospective and thus cannot establish causal relationships. We did not incorporate surgical or endoscopic variables into the statistical analysis, although we recognize that these are important and merit further research, which we are currently undertaking. We did not specifically investigate the role of tacrolimus or mycophenolate mofetil, among other immunosuppressants, since they are not known to significantly inhibit wound healing or cholangiocyte regeneration. There was no single endoscopic treatment protocol in existence at our institution, thus some aspects of endoscopic treatment may have varied over time and between endoscopists; while this may introduce variables that are unaccounted for, it may also increase the generalizability of these findings as compared to data from a specific treatment protocol or a single endoscopist.
In summary, the findings of this exploratory study suggest that sirolimus, particularly at higher doses, may be associated with early recurrent biliary obstruction and premature need for repeat ERCP in patients undergoing endoscopic treatment of biliary strictures, especially ABS. Given the costs and morbidity associated with biliary strictures and additional ERCPs, these findings should fuel larger, prospective studies evaluating pharmacologic as well as clinical, operative, and endoscopic predictors of early recurrence of biliary obstruction in the OLT patient population.
Abbreviations- •
OLT: Orthotopic liver transplantation.
- •
DCD: Donation after cardiac death.
- •
ERCP: Endoscopic retrograde pancreatography.
- •
ABS: Anastomotic biliary stricture.
- •
NABS: Nonanastomotic biliary stricture.
- •
CI: Confidence interval.
- •
OR: Odds ratio.
None.