Endoscopic Retrograde Cholangiopancreatography (ERCP) is commonly performed in patients after liver transplantation. The most common indications for ERCP include treatment of bile leaks and anastomotic and nonanastomotic biliary strictures. In this report we describe an unusual complication of ERCP in a liver transplant recipient with a bile leak two months after orthotopic liver transplantation (OLT). After confirming a bile leak, a hydrophilic guide wire was placed in the intrahepatic duct, an endoscopic sphincterotomy was performed, and a biliary plastic stent was successfully placed over the wire across the bile leak. Within the following 24 hours the patient developed a sharp right-sided upper quadrant pain and a drop in his hemoglobin level. An abdominal CT scan demonstrated a subcapsular hepatic hematoma that was successfully managed conservatively.
A 54-year-old man with a past history of decompensated cirrhosis secondary to hepatitis C and alcohol abuse underwent successful OLT on February 2008. The surgical procedure was uneventful and biliary reconstruction was performed with duct-to-duct choledocho-choledochostomy and T-tube placement. The patient was discharged home after 10 days on tacrolimus, sirolimus and prednisone. He was closely followed in the Liver Transplant clinic and was subsequently electively admitted for removal of the T-Tube 10 weeks post-liver transplantation. A T-tube cholangiogram prior to its removal showed a normal biliary tree with good drainage of contrast into the duodenum. One hour after its removal, the patient complained of sharp pain in the right upper quadrant and midabdomen. On exam the patient was in significant distress and developed abdominal guarding; however vital signs were normal. An abdominal ultrasound and CT scan showed a moderate amount moderate amount of free intraabdominal fluid. Blood work revealed a hemoglobin level of 12 g/dL, white cell count 5.8 X 109 /L, serum C-reactive protein 6.7 mg/dL (normal < 0.8 mg/L), platelet count 66 X 109 /L, AST 31 U/L, ALT 82 U/ L, serum bilirubin 1.7 mg/dL, alkaline phophatase 202 U/L, albumin 3.2 g/dL, prothrombin time 12 seconds, blood urea nitrogen 13 mg/dL and serum creatinine 0.8 mg/dL.
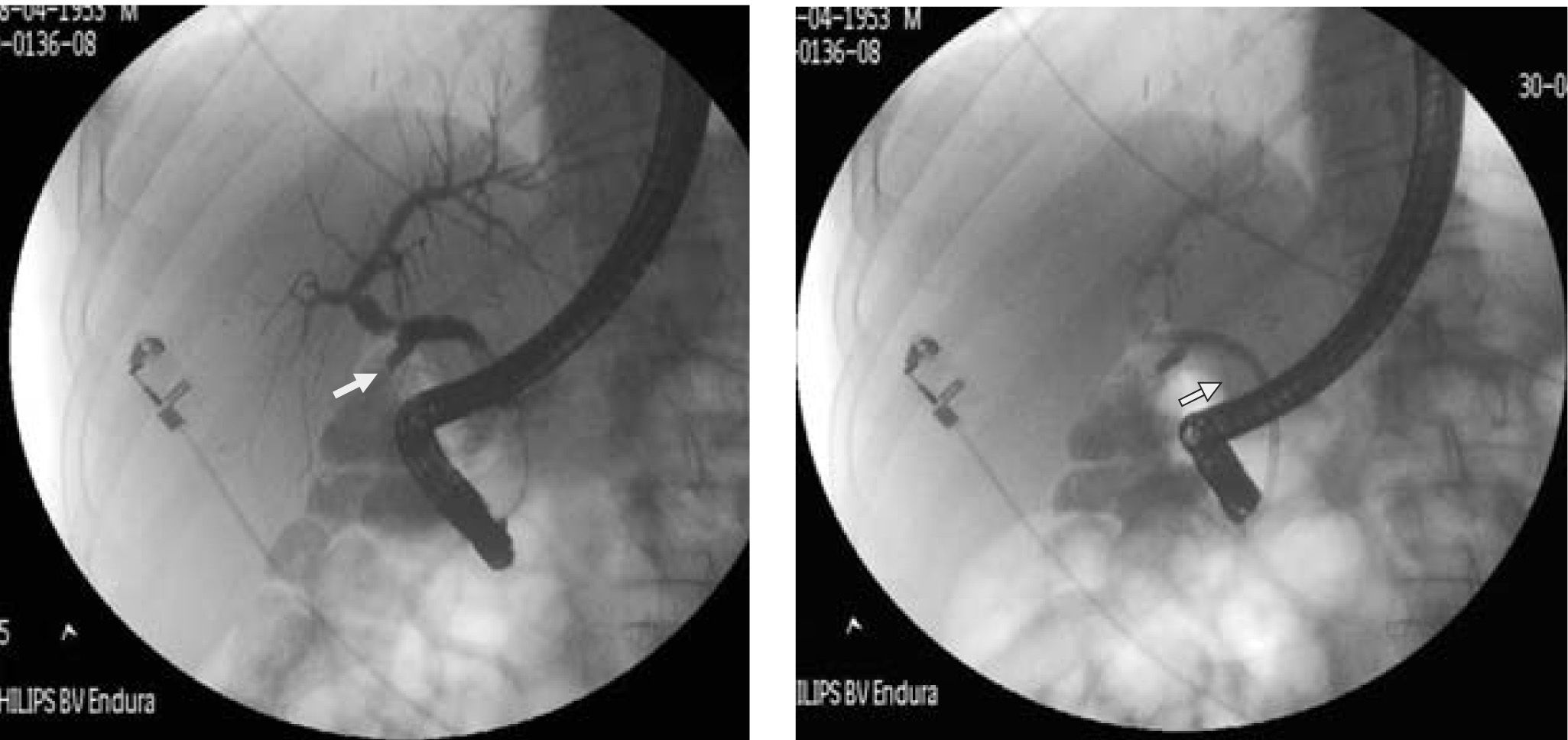
An ERCP was performed and a cholangiogram revealed a bile leak at the mid-common bile duct in the area where the T-Tube was previously located (Figure 1). A 0.035-inch diameter, 450-cm length straight-tip guidewire (Jagwire, Boston Scientific, Newton, USA) was advanced into the left biliary tree and an endoscopic biliary sphincterotomy performed over the guidewire; afterwards a plastic 10 French x 7cm biliary stent was successfully placed across the bile leak (Figure 1).
Over the following 24 hours the patient developed mild mid-abdominal pain without nausea, vomiting, or fever. The abdomen was soft, non-tender, non-distended with normal bowel sounds. His hemoglobin level dropped to 8.8 mg/dL, serum C-reactive protein rose to 27 mg/dl (normal <1 mg/L), and amylase and lipase levels were normal. White blood cell and platelet count, prothrombin time, liver tests and renal function remained stable. An abdominal CT scan showed a 9 x 2 cm subcapsular liver hematoma on the surface of the left lobe of liver (Figure 2).
The patient was treated conservatively with analgesia, intravenous antibiotics, and intravenous fluids. He did not require a blood transfusion. A follow-up ultrasound 4 weeks later did not reveal a hematoma. A follow up ERCP was performed for removal of the plastic stent 6 weeks later showing resolution of the bile leak.
DiscussionThe estimated incidence of biliary complications after liver transplantation ranges between 10 and 25 percent in various reports, although rates seem to decreasing in recent years.1 The majority of complications include biliary tract strictures, bile leaks, and bile duct stones. Most can be managed successfully with ERCP. ERCP is the treatment of choice for patients with bile leaks. A biliary sphincterotomy and placement of a plastic stent in the common bile duct is successful in treating 90 percent of bile leaks.1,2
This case describes an uncommon complication of ERCP that may occur in patients that undergo therapeutic ERCP with guidewire placement. Few cases of subcapsular hepatic hematoma after ERCP have been reported.3-11 However, to our knowledge this is the first case described in a liver transplant recipient. In this case, like in others, the hematoma likely developed as a result of guidewire trauma during the ERCP as there were no other procedures or trauma after the ERCP to explain the hematoma. Other plausible contributing factors in this particular case might include the presence of a low platelet count before the procedure and his immunosupression. In the reported literature management of hepatic hematoma after ERCP has varied from conservative therapy to percutaneous drainage or arterial embolization. In one case the hematoma got infected with Citrobacter freundii requiring CT drainage and antibiotics.3 In another case of a patient with obstructive jaundice due to metastasis, an ERCP for stent placement caused a very large hematoma that required selective embolization of the hepatic artery.4 In one case immediately following ERCP, the patient developed right upper abdominal pain and collapsed requiring intensive resuscitation; a CT scan revealed a large hematoma that required percutaneous drainage.5 In the other reports the hematoma was managed conservatively with intravenous fluids, antibiotics, and analgesia without surgery.6-11 In all the described cases the guidewire has been implicated as the cause of hematoma. Guidewire trauma can occur when the wire is advanced deep into the intrahepatic ducts causing rupture of small blood vessels in the hepatic parenchyma, thereby causing subcapsular hematoma formation. In cases of cholangitis or common bile duct obstruction, infection of the biliary tree can act as a nidus for infection and abscess formation. In this case there was no infection and the patient responded well with conservative management without requiring blood products or any other interventions.
The development of subcapsular hepatic hematoma may occur after therapeutic ERCP; however its occurrence seems to be rare. This is the first reported case of hepatic hematoma after ERCP in a liver transplant recipient. Physicians taking care of liver transplant recipients should be aware of this complication as its timely diagnosis and management with analgesia, intravenous fluids and antibiotics in selected cases are of critical importance in order to avoid the need for surgical re-intervention.