Hepatitis C is, at present, a worldwide health problem and is the most common cause of liver transplantation. Its prevalence in pregnant women is similar to that of the general population. In the absence of cirrhosis and portal hypertension, most HCV-infected pregnant women do not have obstetric complications. Screening of pregnant women that are asymptomatic and do not have risk factors is not cost effective. A high hepatitis C viral load reportedly increases vertical transmission and is higher in women who are coin-fected with HIV or who are intravenous drug users. Prolonged rupture of the membrane for more than 6 h, amniocentesis, and perineal lacerations increase the potential risk of perinatal transmission. Although the hepatitis C virus can be transmitted intrapartum, prevention by caesarean delivery is not generally indicated. The HCV virus can be found in maternal milk; however, breast feeding is not contraindicated. In conclusion, there are no antiviral treatment recommendations for HCV-infected women during pregnancy, or guidelines for the prevention of vertical transmission.
Chronic infection with hepatitis C has become a worldwide health problem and is currently one of the most frequent causes of liver transplantation. There is a particular concern regarding the relative immunosuppression during pregnancy, which could theoretically alter the clinical course of the infection, resulting in vertical transmission to the newborn and a possible chronic infection outcome.1,2
EpidemiologyPregnant women have a prevalence of anti-HCV antibodies similar to that of the general population. Anti-HCV antibodies are detected in 1-2% of people residing in Europe, USA, Taiwan, and Australia. Its frequency is higher in North Africa, where it fluctuates between 15 and 17%.3-5 In 75% of pregnant women with detectable anti-HCV antibodies, the HCV RNA is also present in the serum, indicating active infection. The prevalence increases in pregnant women with significant risk factors, in particular intravenous drug addiction and HIV coinfection. In the latter group, the seroprevalence is reported as 17.1-54%.6,7
Clinical CourseIn the great majority of women, pregnancy does not seem to affect the clinical course of acute or chronic hepatitis C. In an Irish study of women inadvertently infected with HCV-contaminated immu-noglobulin anti-D, an increase in fetal or obstetrical complications was not observed during a follow-up of 20 years in 100 pregnant women compared with controls, despite the presence of biochemical abnormalities in 55% and hepatic fibrosis in 42% of them.8 Nevertheless, a recent study by Pergam found that pregnant women with HCV may have a higher risk of premature rupture of the membrane and that those with excessive weight gain during pregnancy may develop gestational diabetes. In addition, infants born to HCV-infected women are more likely to have low birth weight (< 2,500 g), be small for the gestational age, be premature (< 37 weeks), have neonatal jaundice, have a low Apgar score (< 7 at 5 min), be admitted to a neonatal intensive care unit, and to have a need for assisted ventilation.9
Several studies showed improvement in transami-nases during pregnancy. This may be explained by hemodilution or diminished immunoresponse. In contrast with the decrease in the levels of liver enzymes, an increase in HCV viremia of almost 50% was observed during pregnancy, returning to baseline levels after delivery.10,11
Berkley studied a group of HCV-infected pregnant women undergoing methadone treatment for heroin dependency and observed a greater incidence of low-weight microcephalic newborns from these women compared with the HCV-negative pregnant women recruited into the same program. The authors also observed a higher incidence of cholestasis of pregnancy, especially in Hispanic women, which confirmed the findings of previous reports.12
Conception is infrequent in HCV-cirrhotic women; however, when they become pregnant, these women require special care because of the possibility of decompensation with worsening of portal hypertension (because of increased abdominal pressure and/or plasmatic volume expansion) and secondary coagulopathy, which may produce severe hemorrhage at delivery.13-15
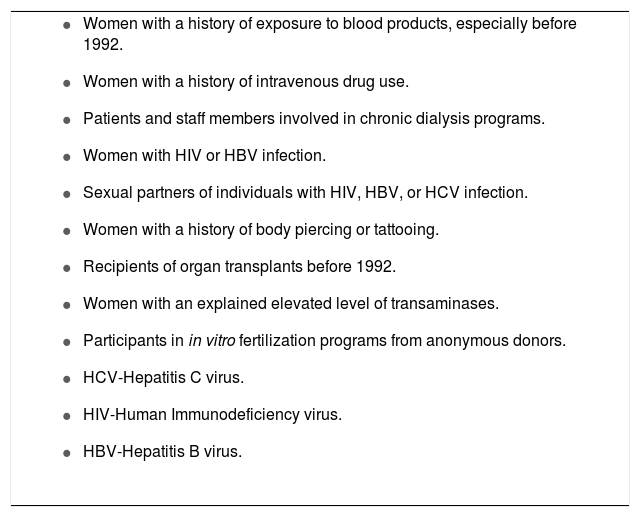
Screening for Hcv in Pregnant WomenHCV screening during pregnancy remains controversial. The fact that about 50% of infected women do not have a clearly defined risk factor argues in favor of this practice. Furthermore, awareness of in fection status may prompt women to modify their life habits, such as limiting alcohol intake or preventing excessive weight gain. The arguments against screening include the fact that there is not an effective therapy for HCV infection during pregnancy, or recommendations to avoid vertical transmission to the newborns. Currently, screening is recommended in high-risk pregnancies or when abnormal transaminase levels are observed (Table 1).7,16
Indications for HCV screening during pregnancy.
|
Many infants born to HCV-infected mothers acquired transplacental immunoglobulin G antibodies passively up to 18 months of life, which renders antibody testing (anti-HCV) of the newborn of little va-lue.17 Cord-blood HCV RNA testing can yield false-positive and false-negative results.9 Viremia can be found in approximately 70% of vertically infected infants by age one; in addition, 90% will have detectable HCV RNA levels at three months of age. A few smaller studies showed “negativization” of the HCV RNA later in infancy after a positive test result in the neonatal period, suggesting that in some infants, postnatal viremia may be transient or that po-lymerase chain reaction assays to detect HCV RNA are not completely reliable.19,20 Therefore, the diagnosis of vertical infection is established by the presence of detectable serum HCV RNA on two occasions, assessed three to four months apart, after the infant is at least two months old and/or by the detection of anti-HCV antibodies at 18 months of age.17,21 Glutamic piruvic transaminase (GPT) and anti-HCV antibodies should be investigated at 18-24 months of life in children born to anti-HCV-positive, HCV-RNA-negative mothers. Follow-up is not necessary if GPT is normal and anti-HCV antibodies are undetectable. HCV-RNA-negative children with abnormal GPT born to HCV-RNA-positive mothers should be tested again for viremia at 6-12 months of age and for anti-HCV antibodies at 18 months of age. HCV-RNA-negative children with normal GPT should be tested for anti-HCV antibodies and GPT at 18-24 months of age and should be considered as noninfected if GPT is normal and anti-HCV antibodies are undetectable. Anti-HCV seropositivity beyond the 18th month in a never-viremic child with normal GPT is likely consistent with past hepatitis virus infection.22
Limited data indicate that less than 10% of infected children develop chronic hepatitis, of which less than 5% evolve to cirrhosis. Infection acquired vertically seems to be mild over the first five years and the proportion of these children with resolved infections is higher than that of infants infected at older ages, for which long-term follow-up is necessary to determine whether the infection has resolved or pro-gressed.23 Yeung found a vertical transmission of 1.7% in mothers who were anti-HCV-positive but HCV-RNA-negative, and that vertical transmission increased to 4.3% if the mother was HCV-RNA-posi-tive. A similar finding was reported by a European multicentric prospective study.20,24
Risk Factors for Mother-To-Child TransmissionViral loadVertical transmission of hepatitis C is directly correlated with viral load. In general’ a higher concentration of serum HCV RNA implies an increased likelihood of vertical transmission, especially if vire-mia is high at the time of delivery.25-27 Transmission is low (~1-3%) in mothers who are anti-HCV-positi-ve but have no detectable HCV RNA.7
HIV coinfectionSeveral studies showed that HIV coinfection favors mother-to-child HCV transmission, as the im-munosuppression produced by the HIV virus causes a high level of viremia in the mother.6,19,28-30 Blac-kard demonstrated that HIV infection facilitates HCV entry and replication in blood cells’ which is a risk factor for perinatal transmission.31 Most of the coinfected mothers had used illicit drugs. The risk of vertical transmission is considered as ~19%,24 although this number seems to decrease (8.7%) when the patients receive high-activity antiretroviral treatment (HAART).20 These results suggest that coinfected pregnant women should be treated with HAART to reduce the risk of perinatal transmission of HIV and HCV.
Intravenous drug addictionSeveral well-performed studies showed that maternal intravenous drug addiction increases the risk of perinatal transmission of HCV.29,32,33 Infection of peripheral blood mononuclear cells with HCV occurs more frequently in these women compared with women without a history of intravenous drug use, which may favor the infection of the newborn.
Infection of the fatherIn a recent study’ Indolfi found that HCV infection of the fathers, who were also the sexual partners of the HCV-infected mothers’ was predictive of HCV vertical transmission and correlated with the history of maternal intravenous drug abuse.34
Level of tansaminasesAlthough the relationship between the histolo-gical degree of HCV in the mother and the likelihood of transmission of HCV infection to the infant has not been explored sufficiently, two recent studies showed that abnormal GPT in the year before pregnancy and at delivery is associated significantly with perinatal transmission of HCV. It is probable that mothers with higher GPT have a more severe disease, which may also mean the presence of a higher viral load. In addition, transaminase abnormalities are associated with higher viral heterogeneity, which is a factor that favors perinatal transmission of both HCV and HIV.35,36
Role of peripheral blood mononuclear cell infectionThere is evidence that maternal peripheral blood mononuclear cell infection by HCV and viral repli-cative activity in these cells are closely related to perinatal transmission, and that this phenomenon was more significant in mothers with defined risk factors. These cells may act as vectors of HCV in the fetus and interact with immunological cells of the placental barrier.31-33
Obstetrical factorsPremature rupture of the membrane, occurring more than 6 h before delivery, is associated with an increased risk of perinatal transmission of HCV.20,37,38 Amniocentesis is a potential risk for the spread of HCV infection to the infant, although HCV was found in the amniotic fluid of only 6.3% of viremic mothers who underwent am-niocentesis during the fourth month of pregnan-cy.39 Invasive monitoring of the fetus in labor with a scalp electrode or exposure of the infant to maternal blood infected by HCV because of the occurrence of vaginal or perineal laceration during vaginal delivery increase the risk of perineal transmission of HCV.40
Gender of the infantPrevious studies do not demonstrate an association between perinatal transmission of HCV and the gender of the infant;29,41 however, a recent study revealed that females were twice as likely to be infected as males. This may be because of a greater female biological susceptibility to the infection.42
Factors not Associated With Perinatal TransmissionMode of deliverySeveral observational studies did not show evidence that the mode of delivery (caesarean section vs. vaginal) influences the risk of HCV perinatal transmission.43,44 Currently, there are no randomized controlled trials aimed at evaluating whether caesa-rean section, rather than vaginal labor, reduces HCV perinatal transmission.45 In contrast, an initial study conducted by the European Paediatric Hepatitis C network reported that caesarean section in patients coinfected with HIV protected against HCV transmis-sion.30 A later study of this same group did not confirm these findings, probably because the HCV/HIV coinfected patients received HAART.20
Breast feedingHCV can be found in low levels in maternal milk and in colostrums; however, these levels were not sufficient to transmit the infection, as the virus can be inactivated easily by the gastric juices and/or anti-infectious components of the maternal milk. Therefore, breast feeding is not prohibited in the absence of damaged, cracked, or bleeding nipples. In cases of HCV/HIV coinfection, breast feeding is based on current recommendations for HIV virus.46-48
Viral genotypeViral transmission takes place with all known HCV genotypes. To date, no correlation was demonstrated between perinatal transmission and genotype. Mast showed that type 1a was the most prevalent, but not the most virulent genotype.21
Recommendations to Pregnant Women With Hepatitis CIn addition to general preventive measures to avoid the transmission of this virus, all HCV-infected patients must be advised to stop alcohol inges-tion and to avoid potentially hepatototoxic drugs, including herbal medicines. Moreover, they should be immunized against hepatitis A and B if they have no protection against these viruses.7
TreatmentThe state-of-the-art treatment for hepatitis C, which is based on pegylated interferon and ribavi-rin, is currently contraindicated during and immediately before pregnancy, because ribavirin poses a high risk of teratogenicity49 and alpha interferon is considered as contraindicated in pregnancy and in children less than two years of age because of potential neurotoxicity. Antiviral therapy is not recommended for the prevention of perinatal transmission. Currently, no HCV vaccine is available and its development will probably take a long time because of the multiple viral genotypes and the fast rate of virus mutation.50
Future DirectionsAdditional research is needed to establish whether a nondetectable viral load in hepatitis C bears the same significance for the transmission rate of HCV as it does in HIV infection. Furthermore, it is necessary to determine the level of viremia that may result in perinatal transmission, and whether the use of interferon and ribavirin treatment prior to delivery in patients with a high viral load diminishes or eliminates HCV vertical transmission, as Lami-vudine does in pregnant women infected with hepatitis B virus.51,52
Conclusions- 1.
The prevalence of HCV in pregnant women is similar to that of the general population.
- 2.
In general, the infection does not impact the clinical course of pregnancy in the absence of cirrhosis; however, there are reports of prematurity, low birth weight, and microcephaly.
- 3.
The risk of vertical transmission is low (~4%) and correlates with high viral load, the use of illicit drugs, and HIV coinfection.
- 4.
Mode of delivery, breast feeding, and viral genotype do not correlate with vertical transmission.
- 5.
At present, there are no recommendations for the treatment of HCV infection during pregnancy, or effective measures to decrease vertical transmission.