Due to time constraints, fewer physicians are performing large volume paracentesis (LVP) resulting in a longer wait time and more emergency department (ED) and hospital admissions. At our institution, after initial supervision, a certified nurse practitioner (NP) has independently performed LVP in a dedicated cirrhosis clinic. The purpose of our study was to evaluate the feasibility and safety of LVP performed by a NP. A retrospective review of patients undergoing LVP between January 2003 and May 2007 was performed. Baseline patient information and the practitioner performing LVP (physician or NP) were recorded. Complications including post paracentesis hypotension, bleeding, local leakage of ascitic fluid, infection, perforation, and death were compared between the two groups. A total of 245 procedures in 41 patients were performed by a single NP, and 244 in 43 patients by physicians. Baseline characteristics of patients undergoing LVP were similar in two groups. Alcohol was the most common etiology of cirrhosis (46% in NP and 51% in physician group) followed by a combination of alcohol plus HCV (37% in NP and 28% in physician group). There was similar distribution of Childs class B and C patients in the two groups, as well as average MELD score. Total volume of ascites removed, number of needle attempts, and complications including post paracentesis hypotension, local leakage of ascitic fluid, bleeding, infection, and death were not statistically different between the two groups. Our study shows no difference between physician and NP performance of LVP and complication rates. LVP performed by a NP is feasible and has acceptable rate of complications.
Recently released final data for U.S. deaths in 2006 from the National Vital Statistics Reports classifies cirrhosis as the 12th leading cause of death.1 Patients with cirrhosis are also at risk for substantial morbidity. As portal hypertension worsens, patients with cirrhosis may develop complications including ascites, hepatic encephalopathy, and variceal hemorrhage.2 First line therapy for ascites includes dietary sodium restriction and diuretics.3 At times, patients may require large volume paracentesis (LVP) for treatment of tense ascites causing abdominal pain, early satiety, nausea, vomiting, or respiratory compromise. LVP may be required on as needed basis for some patients because of sodium non-adherence, or sub-optimal diuresis. However, a subset of patients with refractory ascites or diuretic intolerance will require LVP more frequently.4 LVP in the outpatient setting is often time consuming and being performed by fewer physicians. Thus, patients will visit the emergency department or get admitted to the hospital for LVP resulting in increased use of resources and health care spending.
Nurse practitioners (NPs) may provide a solution to this dilemma. NPs have undergone graduate level training to work and make independent diagnostic and treatment decisions regarding patient care. The role of NPs in the field of gastroenterology, particularly in performing flexible sigmoidoscopy has previously been described both in the United States,5,6 and in the United Kingdom.7-9 At our institution, after initial supervision, a certified NP has independently performed LVP in a dedicated cirrhosis clinic. The purpose of our study was to evaluate the feasibility and safety of LVP performed by a NP trained to perform paracentesis.
MethodsA retrospective analysis of patients undergoing an outpatient LVP at our institution was performed between January 2003 and May 2007. Procedure details had previously been entered in an electronic database in a prospective manner on the day of procedure. Baseline information included age, gender, race, etiology of cirrhosis, and biochemical profile performed at a date closest to LVP to calculate the Childs Pugh Class and MELD score. Information on the practitioner performing LVP (physician or NP), number of attempts, and volume of ascites removed were recorded. Complications including post paracentesis hypotension, bleeding, local leakage of ascitic fluid, local site infection, secondary bacterial peritonitis, perforation, and death were compared between the two groups. Post paracentesis hypotension was defined as a decrease in systolic blood pressure ≥ 20 mmHg after paracentesis. In the two groups analyzed, paracentesis was performed either by a single gastroenterology (GI) NP, or by a first or second year GI fellow. The GI NP completed 10 supervised paracentesis prior to performing them independently. The gastroenterology fellows, who had previously completed 3 years of internal medicine training, had prior experience in large volume paracentesis in their respective residency programs. The project was approved by the local IRB.
Informed consent was obtained prior to each paracentesis. The Safe-T Centesis 6 Fr Catheter Drainage Tray (Cardinal Health Inc., Dublin, OH) was the kit routinely used for procedures. A standard technique for paracentesis was used.10 Patients were positioned comfortably in the supine position with the head of bed elevated to 20-30 degrees. Ultrasound guidance was not used either by the NP or the fellows. Physical examination was used to choose either a right lower quadrant (RLQ) or left lower quadrant (LLQ) site. The abdominal wall was percussed to determine the level of dullness. An optimal site 2 to 4 cm medial and cephalad to the anterior superior iliac spine in the RLQ or LLQ was always chosen. Care was taken to avoid far lateral sites, areas of superficial infection or previous scarring, and engorged veins. Universal precautions with regard to handling of needles and body fluids was observed. A clean gown and sterile gloves was always used. The skin around the site selected for puncture was prepared with 3 povidone iodine swab sticks. The fenestrated drape accompanying the kit was used to form a sterile field. Local anesthetic in the form of 1% lidocaine hydrochloride USP was drawn up into a 10 mL syringe and administered subcutaneously using a 25-G x 1 ½” needle to form a wheal. The wheal site was punctured with a 22-G x 1 ½” needle, injecting and aspirating while advancing the needle deeper into the soft tissue. Upon entering the peritoneal cavity, and aspirating ascites, injection of lidocaine was discontinued. A small stab wound was made with the scalpel provided in the kit. The 6 Fr 20 cm Safe-T Centesis catheter with multiple side holes, over a metal introducer needle, was then inserted in the same tract until ascitic fluid was aspirated. The introducer needle was removed leaving the catheter (pig tail shape) in the peritoneal cavity. The drainage tubing with needle was connected for attachment to 1 liter vacuum bottles. After the desired amount of fluid was obtained, the catheter was removed, and pressure was applied to the puncture site for a short period prior to application of a bandage. Intravenous albumin 25% solution at 8 g/L was replaced for ascites greater than or equal to 5 L removed.
All patients were followed in both the NP continuity clinic and physician (GI fellow or attending) continuity clinic. All GI fellow clinics are staffed by an attending GI physician. The typical paradigm is that patients are followed more frequently in the NP clinic with follow-up every one to two months, while being seen in the physician clinic every three to four months. Details of the visit and changes in treatment plan by the NP are always sent to the physician through electronic medical records.
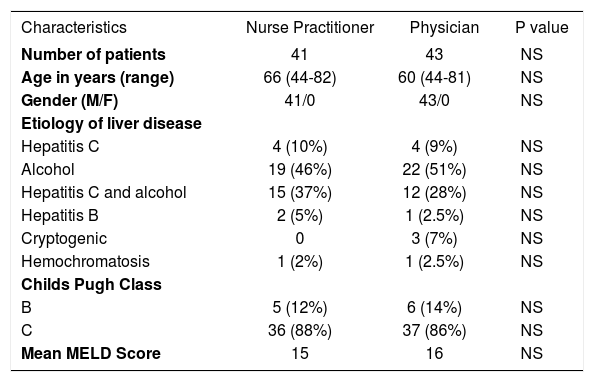
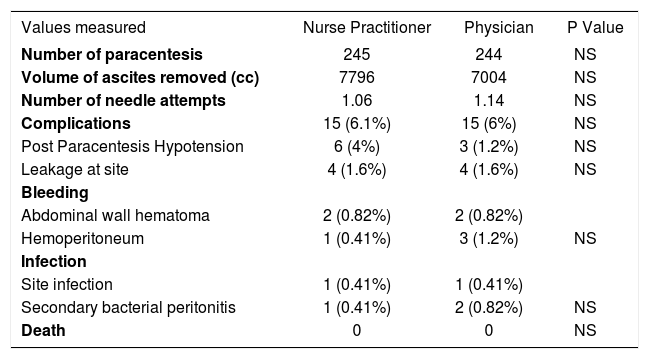
ResultsA total of 489 procedures (245 by NP and 244 by physicians) were recorded in 84 patients. Baseline characteristics of patients undergoing LVP were similar in both groups including age, gender, etiology of liver disease, Childs Pugh Class, and MELD Score (Table 1). In terms of complications, there was no statistical difference whether LVP was performed by the NP or by a physician (Table 2). Five procedures were complicated with bleeding in LVP performed by physicians (2 localized hematomas, and 3 with hemoperitoneum requiring blood transfusion) compared to three procedures (2 local hematoma, 1 hemoperitoneum requiring blood transfusion) in the NP group. Three procedures in the physician group were complicated by infection (2 secondary bacterial peritonitis, 1 local site infection) compared with two (1 secondary bacterial peritonitis, 1 local site infection) in the NP group. There were no deaths, and rates of post paracentesis hypotension, leakage at the site, bleeding, and infections were not statistically different.
Baseline characteristics of patients undergoing LVP.
| Characteristics | Nurse Practitioner | Physician | P value |
|---|---|---|---|
| Number of patients | 41 | 43 | NS |
| Age in years (range) | 66 (44-82) | 60 (44-81) | NS |
| Gender (M/F) | 41/0 | 43/0 | NS |
| Etiology of liver disease | |||
| Hepatitis C | 4 (10%) | 4 (9%) | NS |
| Alcohol | 19 (46%) | 22 (51%) | NS |
| Hepatitis C and alcohol | 15 (37%) | 12 (28%) | NS |
| Hepatitis B | 2 (5%) | 1 (2.5%) | NS |
| Cryptogenic | 0 | 3 (7%) | NS |
| Hemochromatosis | 1 (2%) | 1 (2.5%) | NS |
| Childs Pugh Class | |||
| B | 5 (12%) | 6 (14%) | NS |
| C | 36 (88%) | 37 (86%) | NS |
| Mean MELD Score | 15 | 16 | NS |
Results and complications of large volume paracentesis whether performed by the nurse practitioner or a physician.
| Values measured | Nurse Practitioner | Physician | P Value |
|---|---|---|---|
| Number of paracentesis | 245 | 244 | NS |
| Volume of ascites removed (cc) | 7796 | 7004 | NS |
| Number of needle attempts | 1.06 | 1.14 | NS |
| Complications | 15 (6.1%) | 15 (6%) | NS |
| Post Paracentesis Hypotension | 6 (4%) | 3 (1.2%) | NS |
| Leakage at site | 4 (1.6%) | 4 (1.6%) | NS |
| Bleeding | |||
| Abdominal wall hematoma | 2 (0.82%) | 2 (0.82%) | |
| Hemoperitoneum | 1 (0.41%) | 3 (1.2%) | NS |
| Infection | |||
| Site infection | 1 (0.41%) | 1 (0.41%) | |
| Secondary bacterial peritonitis | 1 (0.41%) | 2 (0.82%) | NS |
| Death | 0 | 0 | NS |
Paracentesis performed by an experienced NP when compared to physicians showed no significant difference in volume of fluid removed per procedure, number of needle attempts, or complications. To date, there is not literature available analyzing the role of NPs in performing paracentesis. A study from Mayo Clinic, Rochester, MN11 showed that gastrointestinal endoscopy assistants can safely perform paracentesis with adequate training. They recommend an optimal number of 10 supervised procedures for an operator to learn paracentesis. Authors concluded that ultrasound is rarely required, routine correction of coagulopathy and thrombocytopenia is not required, and that there is a significant saving in physician time without any increased patient risk.
When performing any procedure, the diagnostic accuracy and safety must be considered. The role of NPs in performing flexible sigmoidoscopy has been extensively studied, including accuracy and safety. In a study from the UK, Goodfellow, et al. showed that an experienced NP, trained in flexible sigmoidoscopy had a 99% procedure completion rate.7 Training before performing independent procedures is of paramount importance. This NP initially had observed 35 procedures, then had withdrawn the endoscope in next 35, and finally performed 35 supervised procedures before performing them independently. Similarly, in a study assessing accuracy of polyp detection,5 the three nurse endoscopists involved in the study completed 100 supervised flexible sigmoidoscopies in a standard training program. In this study, there was no difference found in detection of adenomatous polyps or frequency of complications.
In an already financially scrutinized healthcare system, the use of NPs may also be cost effective. Wallace, et al. showed that the cost per flexible sigmoidoscopy, including the training cost, was lower for NPs compared to physicians.6 Another study by Niv, et al.12 in which an experienced gastroenterology nurse reviewed capsule endoscopy and thumbnailed abnormalities for the physician to review, also showed a savings in cost per examination. In this study, the accuracy of detecting abnormalities was also high with 96.9% interobserver agreement for lesions categorized as “significant” by the physician. In the cost analysis, a potential savings of 57% of the cost of examination was calculated, mainly from less time the physician spends reading the study. Additionally, studies of NPs working in primary care13 and performing hysteroscopy14 show high levels of patient satisfaction for the care they are receiving.
Paracentesis is a procedure in the armamentarium of physicians trained in internal medicine. As patients with cirrhosis decompensate, they may need more frequent LVP to alleviate symptoms. Patients needing paracentesis however may have a difficult time finding a provider to perform this procedure, and are often admitted to the hospital for this routine procedure. Time constraints in outpatient medicine make it difficult for physicians to find a substantial amount of time to perform paracentesis.
Complications in our study are comparable to the reported literature with similar rates of bleeding, leakage, and peritonitis. Significant bleeding after paracentesis in prior studies, defined as either requiring blood transfusion, or a hemoglobin decrease greater than 2 g/dL, was between 0% and 2.7%.11,15,16 Abdominal wall hematoma requiring transfusion was 0.9%, and hematoma not requiring transfusion was also 0.9% in a study by Runyon.16 The incidence of ascitic fluid leakage after paracentesis is between 0.36% and 2.35%,11,17 and in one study, peritonitis or abscess complicating paracentesis was 0.83%.18
We have a dedicated cirrhosis clinic managed by a NP experienced in both liver disease and paracentesis. After initial training and supervision of paracentesis, our NP has performed more than 200 independent procedures, most without complications. Our study shows no difference between physician and NP performance of LVP. Both groups had a similar volume of ascitic fluid removed, and number of needle attempts. Additionally, complications observed were similar among paracentesis performed by NP and physician. We found that LVP performed by a trained NP is feasible and has an acceptable rate of complications. Studies of patient satisfaction and the cost-effectiveness of this model need to be further evaluated.
Abbreviations- •
NP: Nurse Practitioner
- •
LVP: Large volume paracentesis
- •
SBP: Spontaneous bacterial peritonitis
None