Background. Non-total liver resecting invasive treatment of polycystic liver disease has different recurrence rates. The aim of this study is to illustrate why the recurrence rates are different. We established a hypothesis that the cyst number is a constant in polycystic liver disease in a patient’s lifetime.
Material and methods. We selected 287 patients with polycystic liver, in which 35 patients had the record of liver volume, while other 252 patients had the record of length of right liver. Data were divided into 5 groups in terms of age. The intergroup comparison with different ages and clinical files of patients were analyzed.
Results. The mean difference was statistically insignificant when compared amongst groups in the lengths of right liver respectively. Symptom recurrence rates (q) were 19.05 and 17.65% respectively after cyst aspiration-sclerotherapy and non-cyst aspiration-sclerotherapy.
Conclusion. The cyst number is a constant in patients with non-massive or massive polycystic liver disease in their lifetime.
Polycystic liver disease (PLD) is a rare condition, frequently observed with autosomal dominant polycystic kidney disease (ADPKD).1–4 Current invasive management consists of aspiration-sclerotherapy of selected cysts, surgical approaches, the selective transcatheter arterial embolization (TAE) of hepatic arteries and non-invasive clinical trials.5–21 Non-invasive clinical trials have shown possible to reduce liver volume with octreotide or lanreotide.6 20% to 100% recurrence of cyst aspiration-sclerotherapy in patients with PLD is seen within a few months.1,8,17–18 The postoperative recurrence rate is usually high with a range from 13 to 71% in fenestrate with laparoscopy.1,7,9,12–13,15 Symptom recurrence for laparotomy with fenestration ranges from 11 to 26% in the largest case series.1,7,19 Symptoms are typically caused by massive enlargement of polycystic liver or by mass effect from a single or a limited number of dominant cysts.16 To avoid unnecessary therapy, we establish a hypothesis that the total cystic number is a constant in patients with non-massive or massive PLD in their lifetime. This hypothesis can evaluate the outcome of non-total liver resecting invasive treatment on PLD and recurrent PLD patients precisely.
Material and MethodsA simplified method of assessing hepatic size is measuring the length of the right lobe of liver (RLL), i.e. measuring from the top of right hemidiaphragm to the edge of the right lobe of liver capsule at the midclavicular line of right liver.22–25 Oblique diameter of right liver measuring standard section is from the top of right hemidiaphragm in right hepatic vein entrance to the inferior vena cava section, and to the edge of the right lobe of liver capsule at the line of division between anterior and posterior segments of the right lobe. The position is used as supine or left lateral position. The oblique diameter of a normal right lobe of liver should be ≤ 140 mm. Cai, et al.23 reported that the oblique diameter of the right lobe of liver and the RLL in right midclavicular line by ultrasonograghy are 10.37 ± 1.30 cm and 8.46 ± 1.10 cm respectively in normal human livers. To measure the oblique diameter of the right lobe of liver, it is common to measure the RLL at midclavicular line of the right lobe of liver, because the oblique diameter of right liver is very close to the RLL at midclavicular line of the right lobe of liver.22–25 Liver morphology changed dramatically in PLD, and the line of the oblique diameter of the right lobe of liver is not able to be confirmed clearly. So we measured the RLL instead of the oblique diameter of the right lobe of liver. Although the oblique diameters of the right lobe of liver are in our selected patients’ records, the oblique diameter of the right lobe of liver is the RLL in most cases actually.
Polycystic liver disease is defined when 20 cysts are present.5–6 van Keimpema, et al.8 defined PLD as > 15 liver cysts. We define multiple liver cysts as ≤ 10 liver cysts and PLD as > 10 liver cysts.26 Based on the research of Everson, et al.,22 and the classification of Gigot, et al.7 on the PLD, we define that a massive PLD must meet all of the following conditions:
- 1.
- 2.
The cyst-parenchyma volume ratio is larger than 1 by computed tomography.
- 3.
Liver size and cyst’s growth rate in massive PLD is faster than in non-massive PLD. Characteristics of massive PLD are progressive hepatomegaly with the RLL is larger than or equal to 18 cm (liver volume is ≥ 4,484 mL),9 if the patients were untreated. But it is categorized into nonmassive PLD if it is caused by a few large liver cysts (arbitrarily defined as > 8 cm) as these lead to a significantly better liver volume reduc-tion.8 Patients with massive hepatomegaly and highly symptomatic PLD (RLL > 18 cm) is at the end-stage of massive PLD.
- 4.
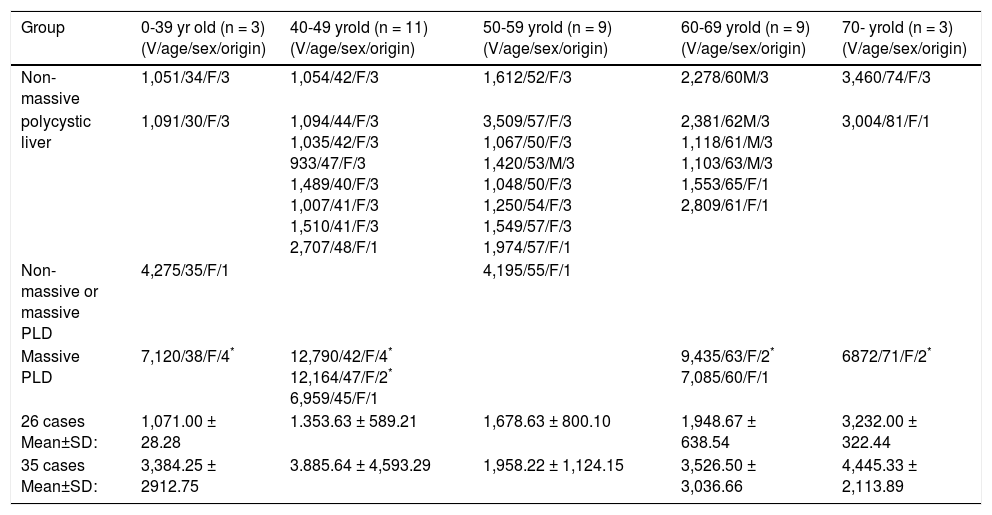
Liver size of non-massive PLD is < 3,509 mL and its RLL is < 18 cm. We define that a massive PLD according to liver volume must meet the condition 1, 2 and 3 above. The normal liver is wedge-shaped and liver morphology changes dramatically in PLD, so we cannot distinguish between non-massive and massive PLD on the liver volume from 3,509 to 4,484 mL such as 4,275 mL and 4,195 mL (Table 1) exactly. So the parameter of liver volume is not useful for identifying nonmassive and massive PLD in fact.
Table 1.Data of total liver volumes (mL) in 35 patients with liver cysts.
Group 0-39 yr old (n = 3) (V/age/sex/origin) 40-49 yrold (n = 11) (V/age/sex/origin) 50-59 yrold (n = 9) (V/age/sex/origin) 60-69 yrold (n = 9) (V/age/sex/origin) 70- yrold (n = 3) (V/age/sex/origin) Non-massive 1,051/34/F/3 1,054/42/F/3 1,612/52/F/3 2,278/60M/3 3,460/74/F/3 polycystic liver 1,091/30/F/3 1,094/44/F/3 1,035/42/F/3 933/47/F/3 1,489/40/F/3 1,007/41/F/3 1,510/41/F/3 2,707/48/F/1 3,509/57/F/3 1,067/50/F/3 1,420/53/M/3 1,048/50/F/3 1,250/54/F/3 1,549/57/F/3 1,974/57/F/1 2,381/62М/3 1,118/61/M/3 1,103/63/M/3 1,553/65/F/1 2,809/61/F/1 3,004/81/F/1 Non-massive or massive PLD 4,275/35/F/1 4,195/55/F/1 Massive PLD 7,120/38/F/4* 12,790/42/F/4* 12,164/47/F/2* 6,959/45/F/1 9,435/63/F/2* 7,085/60/F/1 6872/71/F/2* 26 cases Mean±SD: 1,071.00 ± 28.28 1.353.63 ± 589.21 1,678.63 ± 800.10 1,948.67 ± 638.54 3,232.00 ± 322.44 35 cases Mean±SD: 3,384.25 ± 2912.75 3.885.64 ± 4,593.29 1,958.22 ± 1,124.15 3,526.50 ± 3,036.66 4,445.33 ± 2,113.89 1. Reference 8. 2. Got from reference 11.3. The Second Affiliated Hospital of Harbin Medical University. 4. Reference 10. 26 cases = non-massive polycystic liver. 35 cases = non-massive PLD and massive PLD. V: volume.
This is a retrospective and qualitative study. All patients were untreated with partial hepatectomy in the right lobe previously. Based on our criteria of PLD, 275 PLD patients were diagnosed and managed at the 2nd Affiliated Hospital of Harbin Medical University from January 1990 to December 31, 2006. Among them 252 (67 male and 185 female) were measured the RLL initially by ultrasonography; Two female patients were excluded from the statistical analysis because the RLL were not measured initially. Based on characteristics of division above, 252 patients were categorized into 160 patients with multiple liver cysts, 84 patients with nonmassive polycystic liver and 8 patients with massive hepatomegaly and highly symptomatic PLD (Tables 2 and 3). Eighty six patients with multiple liver cysts, 56 patients with non-massive polycystic liver and 6 patients with massive hepatomegaly and highly symptomatic PLD were contacted. Among them some patients were rehospitalized. Twenty one outpatients (4 male and 17 female) were measured liver volume by computed tomography (CT). Among them one patient’s RLL was 16.5 cm and liver volume was 3,509 mL; another’s RLL was 15.1 cm and liver volume was 3,460 mL measured by CT. They did not have very obvious symptoms when RLL was < 16.5 cm (Table 1). Follow-ups were not done. Fourteen patients (a male and 13 female) with liver volume were obtained from three published articles.8,10–11 Among them 7 patients are from van Keimpema, et al.’s article,8 and they were categorized into non-massive and massive PLD (Table 1).
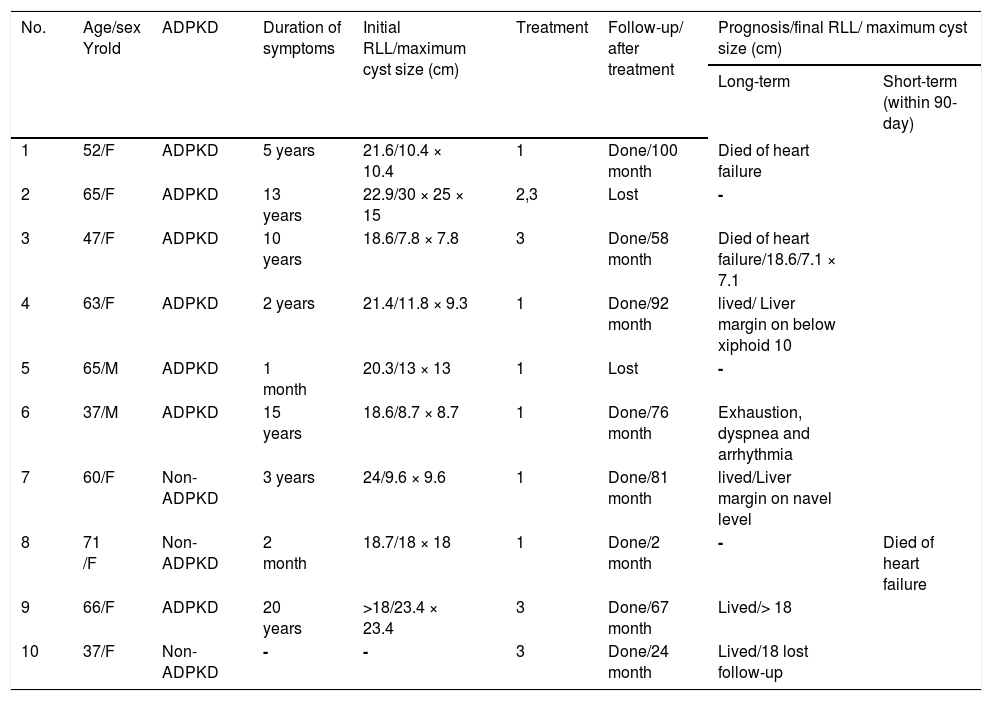
Characteristics of massive polycystic liver disease.
| No. | Age/sex Yrold | ADPKD | Duration of symptoms | Initial RLL/maximum cyst size (cm) | Treatment | Follow-up/ after treatment | Prognosis/final RLL/ maximum cyst size (cm) | |
|---|---|---|---|---|---|---|---|---|
| Long-term | Short-term (within 90-day) | |||||||
| 1 | 52/F | ADPKD | 5 years | 21.6/10.4 × 10.4 | 1 | Done/100 month | Died of heart failure | |
| 2 | 65/F | ADPKD | 13 years | 22.9/30 × 25 × 15 | 2,3 | Lost | - | |
| 3 | 47/F | ADPKD | 10 years | 18.6/7.8 × 7.8 | 3 | Done/58 month | Died of heart failure/18.6/7.1 × 7.1 | |
| 4 | 63/F | ADPKD | 2 years | 21.4/11.8 × 9.3 | 1 | Done/92 month | lived/ Liver margin on below xiphoid 10 | |
| 5 | 65/M | ADPKD | 1 month | 20.3/13 × 13 | 1 | Lost | - | |
| 6 | 37/M | ADPKD | 15 years | 18.6/8.7 × 8.7 | 1 | Done/76 month | Exhaustion, dyspnea and arrhythmia | |
| 7 | 60/F | Non-ADPKD | 3 years | 24/9.6 × 9.6 | 1 | Done/81 month | lived/Liver margin on navel level | |
| 8 | 71 /F | Non-ADPKD | 2 month | 18.7/18 × 18 | 1 | Done/2 month | - | Died of heart failure |
| 9 | 66/F | ADPKD | 20 years | >18/23.4 × 23.4 | 3 | Done/67 month | Lived/> 18 | |
| 10 | 37/F | Non-ADPKD | - | - | 3 | Done/24 month | Lived/18 lost follow-up | |
1. Cyst aspiration and alcohol sclerosis. 2. A combined partial hepatic cyst wall excision and Roux-en-Y hepatic cystojejunostomy with internal drainage. 3. Hepatic resection with fenestration. ADPKD: autosomal dominant polycystic kidney disease. RLL: length of right liver. F: female. M: male.
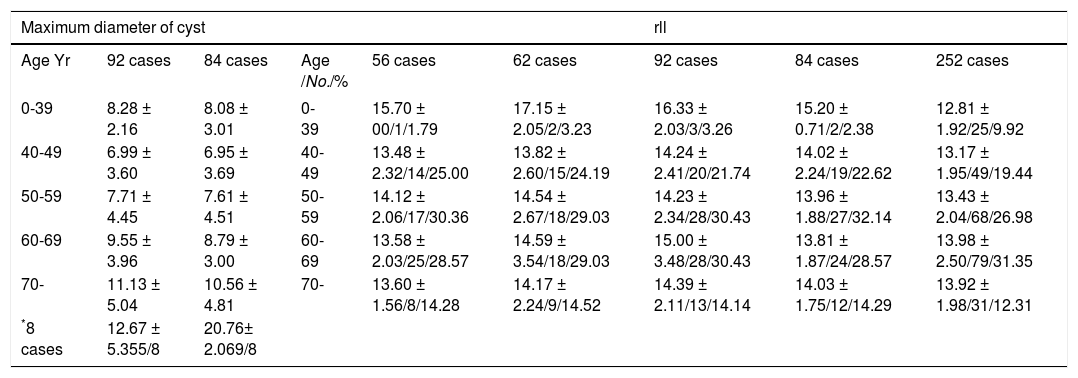
Maximum diameter of cyst (cm) and RLL in 252 cases.
| Maximum diameter of cyst | rll | |||||||
|---|---|---|---|---|---|---|---|---|
| Age Yr | 92 cases | 84 cases | Age /No./% | 56 cases | 62 cases | 92 cases | 84 cases | 252 cases |
| 0-39 | 8.28 ± 2.16 | 8.08 ± 3.01 | 0-39 | 15.70 ± 00/1/1.79 | 17.15 ± 2.05/2/3.23 | 16.33 ± 2.03/3/3.26 | 15.20 ± 0.71/2/2.38 | 12.81 ± 1.92/25/9.92 |
| 40-49 | 6.99 ± 3.60 | 6.95 ± 3.69 | 40-49 | 13.48 ± 2.32/14/25.00 | 13.82 ± 2.60/15/24.19 | 14.24 ± 2.41/20/21.74 | 14.02 ± 2.24/19/22.62 | 13.17 ± 1.95/49/19.44 |
| 50-59 | 7.71 ± 4.45 | 7.61 ± 4.51 | 50-59 | 14.12 ± 2.06/17/30.36 | 14.54 ± 2.67/18/29.03 | 14.23 ± 2.34/28/30.43 | 13.96 ± 1.88/27/32.14 | 13.43 ± 2.04/68/26.98 |
| 60-69 | 9.55 ± 3.96 | 8.79 ± 3.00 | 60-69 | 13.58 ± 2.03/25/28.57 | 14.59 ± 3.54/18/29.03 | 15.00 ± 3.48/28/30.43 | 13.81 ± 1.87/24/28.57 | 13.98 ± 2.50/79/31.35 |
| 70- | 11.13 ± 5.04 | 10.56 ± 4.81 | 70- | 13.60 ± 1.56/8/14.28 | 14.17 ± 2.24/9/14.52 | 14.39 ± 2.11/13/14.14 | 14.03 ± 1.75/12/14.29 | 13.92 ± 1.98/31/12.31 |
| *8 cases | 12.67 ± 5.355/8 | 20.76± 2.069/8 | ||||||
252 patients = 160 patients with multiple liver cysts and 92 patients with PLD. 92 patients with PLD = 84 patients with non-massive polycystic liver and
The subjects were divided into 5 groups in terms of age (Table 3). To provide appropriate evidence to substantiate this hypothesis, data mentioned above were analyzed. Variables as gender, age at diagnosis, patients with body mass index, symptoms, cyst diameter, cyst complications, the biochemical characteristics, comorbidity, extrahepatic cysts, various treatment complications, recurrence of symptoms, and outcome were analyzed. The present study was performed strictly under the guidelines of the declaration of Helsinki.
Statistical analysisStatistical Package for the Social Sciences (SPSS) 17.0 was used in the test. One-way analysis of variance (ANOVA) with Student-Newman-Keuls tests and post hoc multiple comparisons were used to assess significant differences amongst groups with different ages. Results were presented as means ± standard deviation (SD). The difference was considered to be significant if p < 0.05.
Results254 patients (67 male and 187 female) were associated with other diseases, including ADPKD in 36 cases, splenomegaly in one, dilatation of inner hepatic bile duct in two, pancreatic atrophy in one, multiple cholescystic polyposis in one, cholecystitis in 107, cholelithiasis in 10, multiple cysts of spleen in one, chronic pancreatitis in one, incomplete obstruction of outer hepatic duct in one and straitness of choledochoduodenal junction in one.
Thirty one patients (15 male and 16 female) were asymptomatic in pre-operation period. 223 patients were symptomatic. Specific symptoms included abdominal distention in 165 patients, early satiety in 25, intermittent chronic abdominal pain in 185, upper right quadrant of the abdominal non-tenderness mass in 95, supine dyspnea in 7, discontinuous low degree elevated fever related to superinfected cysts in 10, jaundice in 4, lumbago in one, weakness in 17 and intermittent nausea with vomiting in 18. Other examinations were within essentially normal range.
One hundred sixty multiple liver cysts patientsThirteen patients (3 male and 10 female, RLL ≤ 14.6 cm, cyst size ≤ 16 cm × 13 cm) were untreated initially. Among them a 57-year-old symptomatic and a 76-year-old asymptomatic female showed continuously enlarged preexisting cysts with 3.3 cm and 2 cm of maximum cyst in diameter respectively, and they survived well until the age of 63 and 82 respectively. A 70-year-old female survived to the age of 74. A 61-year-old female died of natural causes at the age of 75. Their liver size did not show continuously enlarged. Nine patients with a mean age of 45.7 yr (range from 28 to 78 yr old) were lost in follow-up, among whom one female was asymptomatic before treatment, another 39-year-old male performed cyst aspiration-sclerotherapy twice at the age of 47 (Table 3).
One hundred forty seven patients underwent initial treatmentOne hundred forty seven patients (43 male and 104 female), ranging from 19 to 84 (mean age = 54.4) yr, were hospitalized for the first time. The mean age of initial appearance of symptoms was 52.4 (range from 19-84) yr. The mean duration of symptoms was 23 mo (0 to 13 yr).
One hundred forty seven patients (RLL ≤ 17.6 cm, cyst size ≤ 20 cm × 30 cm) underwent initial treatment, including cyst aspiration-sclerotherapy in 81 cases; fenestration or partial hepatic resection with fenestration in 54; combined partial hepatic cyst wall excision and Roux-en-Y hepatic cystojejunostomy with internal drainage in 7, among which one patient had multiple treatment with cyst aspiration-sclerotherapy initially; left lobectomy in 4 and right lobectomy in 1.
Sixty-six patients (21 male and 45 female, RLL ≤ 17.5 cm, cyst size ≤ 20 cm × 13 cm) were lost in the follow-up. Among them 9 patients (4 male and 5 female) were asymptomatic in pre-operation period. Their treatment includes cyst aspiration-sclerotherapy in 33 cases, (among them a 48-year-old symptomatic patient with ADPKD induced to chronic nephropathy and then developing to renal failure performed cyst aspiration-sclerotherapy twice at the age of 56); fenestration or partial hepatic resection with fenestration in 27; combined partial hepatic cyst wall excision and Roux-en-Y hepatic cystojejunostomy with internal drainage in 4, (among which one patient had multiple treatment with cyst aspiration-sclerotherapy initially); and left lobectomy in 2.
During follow-up, 67 patients (16 male and 51 female, RLL ≤ 17.6 cm, cyst size ≤ 20 cm × 30 cm) did not show a continuously enlarged preexisting cyst and liver after treatment. Among them 10 patients (3 male and 7 female) were asymptomatic. They survived well until a mean age of 61.3 yr (range from 29 to 87 yr old). Among them a 58-year-old female was diagnosed with left breast cancer. She performed a modified radical mastectomy at the age of 63 and survived to 64.
Ten patients with multiple liver cysts (6 female and 4 male, aged from 31 to 84 with mean = 62.9, RLL ≤ 15.3 cm, cyst size ≤ 15 cm × 12 cm) died at a mean age of 68.2 yr (range from 32 to 86 yr old). Among them 2 male patients were asymptomatic. They died of causes unrelated to multiple liver cysts, including lung cancer in 2 at the age of 59 and 84 respectively, and myocardial infarction in 2 at the age of 48 and 70 respectively. One female died of unclear causes at the age of 32. Five patients died of natural causes at the age of 75, 75, 75, 86 and 78 respectively. During follow-up their liver size and preexisting cyst did not show enlarge respectively.
Four patients (2 male and 2 female, RLL ≤ 14 cm and cyst size ≤ 14.2 cm × 14.2 cm) showed enlarged preexisting cysts. A 65-year-old male showed a continuously enlarged preexisting cyst with 3.7 cm of cyst in diameter on the right lobe of liver after cyst aspiration-sclerotherapy. He was performed cyst aspiration-sclerotherapy again and survived well until the age of 81. A 47-year-old female patient showed a continuously enlarged preexisting cyst with 8.5 cm in diameter on the left lobe of liver after cyst aspiration-sclerotherapy. She was untreated and survived well until the age of 58. A 67-year-old male asymptomatic and a 38-year-old female asymptomatic patient showed a 6.0 and 12.3 cm in diameter of continuously enlarged preexisting cyst respectively after fenestration or partial hepatic resection with fenestration, and then they were untreated and survived well until the age of 73 and 44 respectively.
Symptom recurrence rate (q) was 4.17% (2/48) in 48 contacted multiple liver cysts patients after cyst aspiration-sclerotherapy. Symptom recurrence rate (q) was 0 (0/33) in 33 contacted multiple liver cysts patients after non-cyst aspiration-sclerotherapy.
Ninety four PLD patients (cyst number > 20)A 39-year-old female symptomatic patient with RLL with 18 cm was measured 2 years after partial hepatectomy with fenestration, and then she was lost in follow-up. A 66-year-old symptomatic female experienced cyst aspiration-sclerotherapy and drainage two months after initial fenestration. Their RLLs were not measured initially (Table 2; No. 9, 10). They had symptom recurrence.
In the 92 PLD patients (29 male and 63 female, aged from 30 to 79 with mean = 57.3 yr), the mean age of initial appearance of symptoms was 54.8 (range from 30 to 78) yr. The mean duration of symptoms was 28.8 mo (range from 0 to 20 yr).
Six patients (4 male and 2 female, RLL ≤ 15.5 cm, cyst size ≤ 6 cm × 6 cm) were untreated. Among them a 62-year-old and a 40-year-old male died of natural causes at the age of 63 and liver cancer at the age of 42 respectively. A 40-year-old female survived well until the age of 49. They did not show a continuously enlarged liver and preexisting cyst. A 58-year-old male asymptomatic, a 67-year-old male symptomatic and a 58-year-old female symptomatic patient were lost in follow-up.
Eighty-six patients with non-massive polycystic liver (RLL < 18 cm, cyst size ≤ 21.1 cm × 21.1 cm) and massive hepatomegaly and highly symptomatic PLD (18 cm ≤ RLL ≤ 24 cm, cyst size ≤ 30 cm × 25 cm) with a mean age of 57.5 yr (range from 30 to 79 yr old) underwent initial treatment, including cyst aspiration-sclerotherapy in 62 cases and fenestration or partial hepatic resection with fenestration in 23, among whom one patient had multiple treatments with the combined partial hepatic cyst wall excision and Roux-en-Y hepatic cystojejunostomy with internal drainage, and left lobectomy in one.
Nineteen patients with non-massive polycystic liver (7 male and 12 female, RLL ≤ 16.7 cm, cyst size ≤ 13 cm × 13 cm) and a 65-year-old male patient with massive hepatomegaly and highly symptomatic PLD (Table 2) were performed cyst aspiration-sclerotherapy. Six patients with non-massive polycystic liver (2 male and 4 female, RLL ≤ 17.2 cm, cyst size ≤ 15 cm × 15 cm) were performed fenestration or partial hepatic resection with fenestration. A 65-year-old female with massive hepatomegaly and highly symptomatic PLD had multiple treatments with the partial hepatic resection with fenestration and the combined partial hepatic cyst wall excision and Roux-en-Y hepatic cystojejunostomy with internal drainage. They were lost in follow-up. Among them 4 patients (3 male and a female) were asymptomatic in pre-operation period.
Twenty patients with non-massive polycystic liver (4 male and 16 female, RLL ≤ 17.4 cm, cyst size ≤ 19 cm × 19 cm) survived well until a mean age of 67.3 yr (range from 51 to 85 yr old) after initial cyst aspiration-sclerotherapy. Eight patients with non-massive polycystic liver (a male and 7 female, RLL × 16.7 cm, cyst size × 21.1 cm × 21.1 cm) survived well until a mean age of 58.9 yr (range from 51 to 73 yr old) after initial hepatic resection with fenestration. A 63-year-old female with non-massive polycystic liver with 8 cm x 8 cm of maximum cyst and 12.1 cm of RLL survived to 67-year-old after left lobectomy. They did not show a continuously enlarged liver and preexisting cyst respectively during follow-up. Among them a male was asymptomatic during pre-operation time.
Twelve symptomatic patients with non-massive polycystic liver (4 male and 8 female, RLL < 18 cm, cyst size < 17.6 cm x 11.3 cm) with a mean age of 62.7 yr (range from 44 to 74 yr old) were performed cyst aspiration-sclerotherapy and died at a mean age of 68.3 yr (range from 53 to 79 yr old) after initial cyst aspiration-sclerotherapy. They died of causes unrelated to PLD including liver cancer in one case at the age of 79 yr, lung cancer in 2 at the age of 53 and 58 respectively, kidney cancer in one at the age of 73, stomach cancer in one at the age of 53, cerebral hemorrhage in one at the age of 71, and ADPKD induced to chronic nephropathy and then developing to renal failure with secondary urethritis in one at the age of 76. Five patients died of natural causes at the age of 76, 78, 63, 66 and 73 respectively.
A 55-year-old male with symptomatic non-massive polycystic liver (RLL = 14.5 cm, cyst size = 8.0 cm x 8.0 cm) had recurrence with 2 cm in diameter of cyst after partial hepatic resection with fenestration and died of unclear causes at the age of 57.
A 47-year-old female with massive hepatomegaly and highly symptomatic PLD had symptom recurrence after partial hepatic resection with fenestration and died of heart failure induced by Budd-Chiari syndrome caused by the increased liver volume (Table 2).
Two female (aged 52 and 71 yr respectively) with massive hepatomegaly and highly symptomatic PLD had symptom recurrence after cyst aspiration-sclerotherapy and died of heart failure induced by Budd-Chiari syndrome caused by the increased liver volume (Table 2). Three female with massive hepatomegaly and highly symptomatic PLD had symptom recurrence after cyst aspiration-sclerotherapy and survived well until the age of 43, 71 and 66 respectively. Among them two patients were performed cyst aspiration-sclerotherapy again. They showed continuously and very slowly enlarged liver and preexisting cysts respectively (Table 2).
Five symptomatic patients with non-massive polycystic liver (3 male and 2 female) survived well after the second time of cyst aspiration-sclerotherapy. Among them a 54-year-old patient developed ADPKD induced to chronic nephropathy and then developed renal failure with secondary urethritis at the age of 67. One patient had non-symptom recurrence, showed a continuously enlarged preexisting cyst lying on the liver surface with 3.0 cm in diameter and 3 patients had symptom recurrence, they showed a continuously enlarged preexisting cyst lying on liver surface with 4.2 cm x 5.3 cm, 9.2 cm x 9 cm and 8.0 cm x 5.2 cm of maximum cyst respectively and were performed cyst aspiration-sclerotherapy twice. Among them a 69-year-old patient who developed secondary infection in hepatic cysts was treated by antibiotics. They survived well until the age of 51, 55, 76 and 80 respectively.
Six patients with non-massive polycystic liver (a male and 5 female, aged from 41 to 70 yr old with mean = 55 yr) had non-symptom recurrence after fenestration or partial hepatic resection with fenestration. They had continuously enlarged preexisting cysts number revised within 11 and a mean maximum cystic diameter of 3.3 cm (range, 2 to 7 cm) respectively. A 41-year-old female was performed cyst aspiration-sclerotherapy again. Five patients were untreated for enlarged preexisting cyst and their liver did not show enlargement, among whom a 53-year-old male developed secondary infection in hepatic cysts, and was treated with antibiotics successfully. They survived well until a mean age of 60.8 yr (range from 48 to 78 yr old) respectively.
The early postoperative morbidity rate was 4.05% (6/148), which was related to hemorrhage in 2 cases and infection in 4. Symptom recurrence rate (q) was 19.05% (8/42) in 42 contacted patients after cyst aspiration-sclerotherapy and 17.65% (3/17) in 17 contacted patients after fenestration, partial hepatic resection with fenestration and left lobectomy respectively. The long-term mortality rate (q) and short-term mortality rate (q) related to patients with massive hepatomegaly and highly symptomatic PLD were 28.6% (2/7) and 14.3% (1/7) respectively in 10 massive PLD patients (Table 2). The overall mortality rate related to PLD was 3.26% (3/92).
Statistical analysisThe mean level of the maximum diameter of cysts and the RLL increase respectively. The mean difference was statistically insignificant in RLL when compared amongst groups:
- 1.
In 148 contacted patients in 252 patients with multiple liver cysts, non-massive and massive PLD respectively (one-way ANOVA and the Student Newman-Keuls test, F = 0.934 df = [4,143], p = 0.446 > 0.05; F = 2.165 df = [4, 247], p = 0.073 > 0.05);
- 2.
In 92 patients with non-massive and massive PLD, (F = 0.683 df = [4, 87], p = 0.606);
- 3.
In 84 patients with non-massive polycystic liver (F = 0.247 df = [4, 79], p = 0.901).
- 4.
In 62 contacted patients with non-massive and massive PLD (F = 0.654 df = [4, 57], p = 0.626);
- 5.
In 56 contacted patients with non-massive polycystic liver (F = 0.461 df = [4, 51], p = 0.764).
The livers of neonates and young children PLD are usually normal in microscopy.27–29 Massive polycystic liver disease is associated with female sex, pregnancy, and exposures to exogenous use of female steroid hormones.1,3–4,14–16,27 However, positive correlation between estrogen level and prevalence of hepatic cysts are not proven yet.14 Biliary microhamartomas may also develop as postnatally acquired lesions after exposure to certain toxins, as shown by studies in human and experimental animals.3 It is consistent with our current data of patients with massive hepatomegaly and highly symptomatic PLD (Table 2). The effect of the natural female gonadal steroid hormones in the increase of cyst number with age declined after the age of 45-50 yr old.30 In terms of chromosomal defect risks, the optimal age of pregnancies in women is below 35 yr old.31–32 93.93% of patients with cysts are older than 40 yr old,15,27 which was similar to the dominant distributive number of patients with age in our current study: 96.74% (89/92) in 92 patients and 96.77% (60/ 62) in 62 contacted patients with non-massive and massive PLD respectively (Table 3).
Everson, et al.22 reported the relationship between hepatic lengths by ultrasonography and total hepatic volume by CT. Total liver volume measured by CT (y-axis) is compared to liver length measured in the right midclavicular line by US (x-axis). Total liver volume was not correlated to hepatic parenchyma volume, but was correlated strongly with hepatic cyst volume (r = 0.994, p < 0.001). Liver volume was correlated with hepatic length although the slope was small when hepatic length was within the 18 cm range.22–25 The slope of the line relating the total liver volume to the hepatic cyst volume was 1.02 ± 0.05.22 Beyond a hepatic length of 18 cm, small increases in hepatic length were associated with large increase in liver volume.22 The cysts not only increase in number with age, but also in size.15,27 But Que, et al. observed the pattern of growth of polycystic liver disease. They suggested that the enlargement of preexisting cysts is more important than the development of new cysts.4 The newly developed hepatic cysts after the age of 40 yr old can be eliminated because it needs at least 29 years for a cyst to dilate into symptomatic cyst size.4 The results above indicate that the increase of RLL and total liver volume was mainly related to the continuously enlarged preexisting cyst in patients with PLD.22 The above cited previous research results confirm this hypothesis.
Twenty-six cases of non-massive polycystic liver with liver volume and 35 cases of non-massive and massive PLD with liver volume were limited samples, and the age distribution did not exist in the natural range. And the parameter of liver volume cannot distinguish between non-massive and massive PLD in fact. So the parameter of liver volume is not performed with statistical analysis. The mean difference was statistically insignificant when compared amongst groups in RLL respectively.
ConclusionThe cyst number is a constant in patient with nonmassive or massive PLD in their lifetime. This hypothesis could explain why the recurrence rates are varied in PLD. Aspiration with sclerotherapy only treats a dominant cyst or few dominant cysts lying on the liver surface, and the other enlarged deeply seated cysts are rarely treated,1,8,17–18 therefore symptom recurrence rate was higher than other therapies. In patients with the majority of cysts in segments VI, VII, VIII and in deeply seated cysts, it is difficult to visualize and fenestrate with laparoscopy.1,7,13 Fenestration relies on the deroofing of both superficial and deep-sited hepatic cysts with internal drainage into the peritoneal cavity.1,7,19,24,33 The same result of above has also been documented in our study. The growth feature is similar to malignant tumor in massive PLD patients. Eight patients with massive hepatomegaly and highly symptomatic PLD had active therapy, so their life prolonged. Any active therapy reduces liver volume can prolong life of the massive PLD patients.
Author ContributionsLong-Xian Zheng and Ai-Wu Liu contributed equally to this work.
Zheng LX, Liu AW, Cui J and Jiang HJ designed the research. Qin HD, Jia HB, Zheng LX, Liu AW performed the operation. Zheng LX, Cui J and Liu AW collected the data and the literature back-ground. Zheng LX and Liu AW wrote the paper. Zheng LX reviewed the paper.
AcknowledgementWe are grateful to Li Kang, professor of Dept. of Biostatistics and Wu Li-Jie, professor of Dept. of Children’s and Adolescent Health, College of Public Health, Harbin Medical University for their helps with the statistical analysis and their many comments.