The development of pancreatic metastases in renal carcinoma is very uncommon.
The aim of the paper is to present a clinical case of this disease and review the clinical presentation, diagnosis, and treatment.
Clinical caseA case is presented of a 72-year-old female, with a history of renal carcinoma in the right kidney treated by total nephrectomy. At follow-up, in a radiological control, a suspicious metastatic pancreatic lesion was detected. A distal pancreatectomy with splenectomy was performed, and histopathology confirmed the origin as metastatic renal cancer.
ConclusionsPancreatic metastases from renal cancer are very rare, and are usually diagnosed in the monitoring the primary cancer (because most of them are asymptomatic). The treatment for isolated resectable pancreatic metastases without extra-pancreatic extension is surgical resection.
El desarrollo de metástasis pancreáticas de un cáncer de células renales es muy infrecuente.
El objetivo del trabajo es presentar un caso clínico de esta enfermedad y realizar una revisión de la presentación clínica, del diagnóstico y tratamiento.
Caso clínicoPaciente mujer de 72 años, con antecedentes de carcinoma renal derecho, tratado mediante nefrectomía total. En el seguimiento se detectó en un control radiológico una lesión pancreática, sospechosa de metástasis. Se realizó una pancreatectomía distal con esplenectomía. A través del estudio histopatológico se confirmó el origen metastásico del cáncer renal.
ConclusionesLa metástasis pancreática de un cáncer de riñón es muy rara y suele diagnosticarse en el seguimiento de la neoplasia primaria (ya que la mayoría son asintomáticos). El tratamiento de elección de una metástasis pancreática solitaria, resecable sin extensión extrapancreática, es la resección quirúrgica.
Isolated pancreatic metastasis is exceptional and may be caused by several primary tumours.1–3
The mechanism causing the production of isolated pancreatic metastases of renal carcinoma may be haematogenic or lymphatic.4 Clinical signs will depend on the site and are similar to those produced by a primary pancreatic tumour (obstructive jaundice, intestinal bleeding, abdominal pain, weight loss, pancreatitis, diabetes mellitus, etc.).2 They are asymptomatic in up to 50% of cases and are usually diagnosed in the follow-up of primary neoplasia.1,5–10
In computed tomography and magnetic resonance they present as highly vascularised lesions, usually very large in size, with well defined margins,1,2 which may be confused with a primary neuroendocrine tumour of the pancreas,1–3 and complementary tests are therefore undertaken to establish a differential diagnosis.
The treatment of choice for isolated resectable pancreatic metastases without extra-pancreatic extension is resection. Site conditions the technique to employ, with corresponding oncological criteria, to obtain a safety margin.1,2,4
There follows the clinical case of this rare entity and a review of the literature.
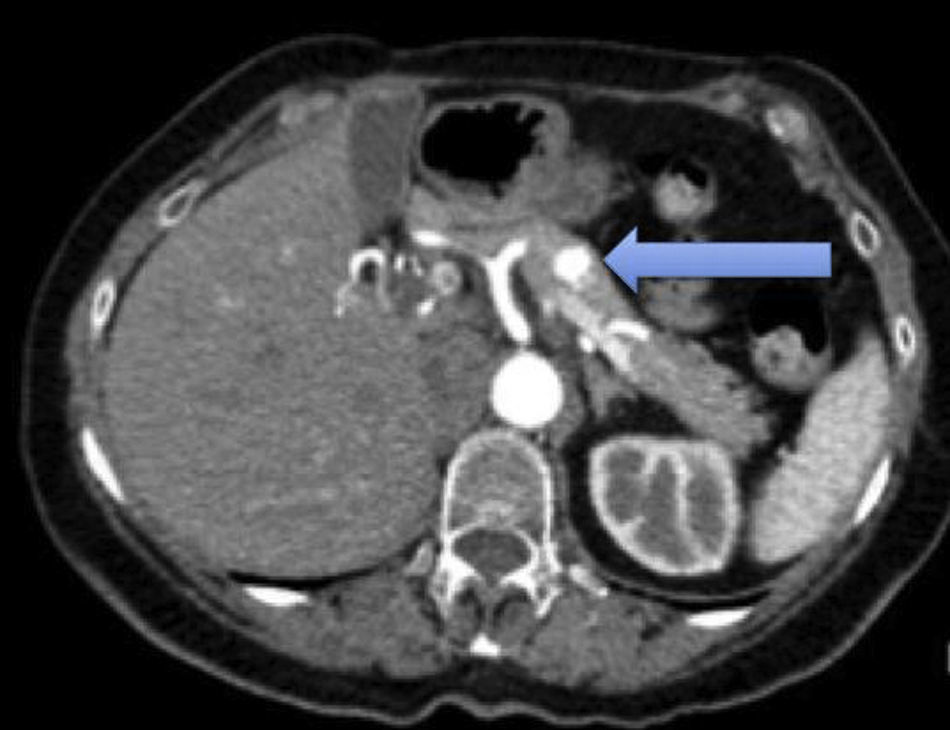
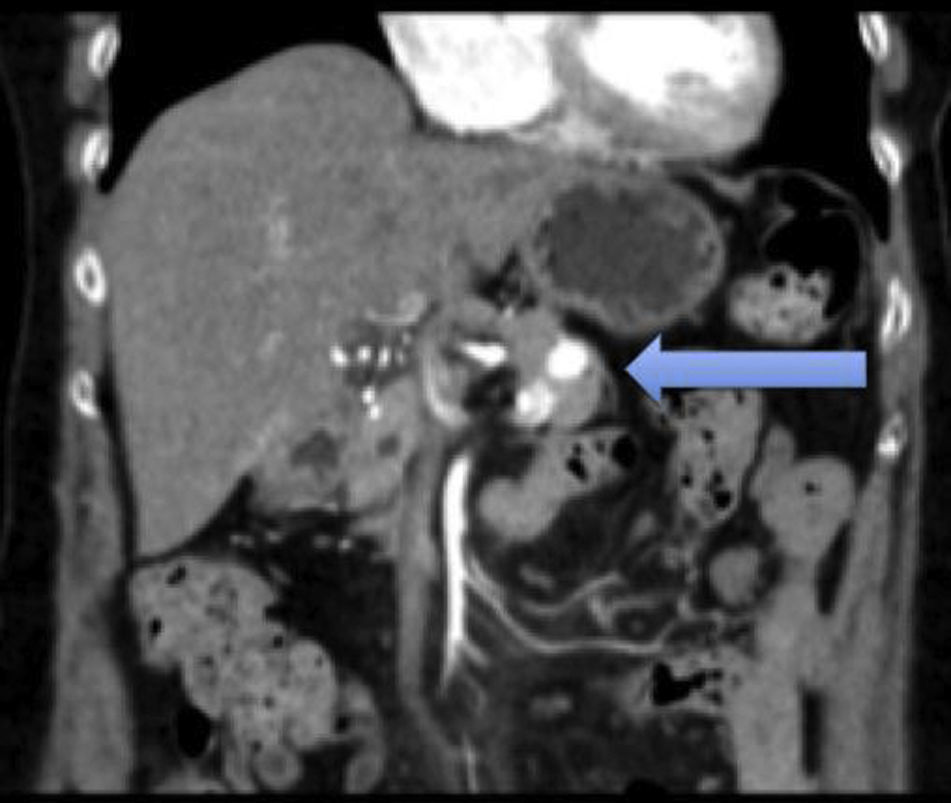
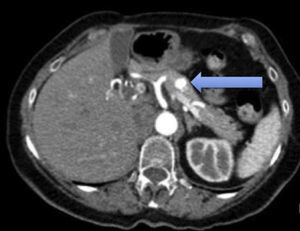
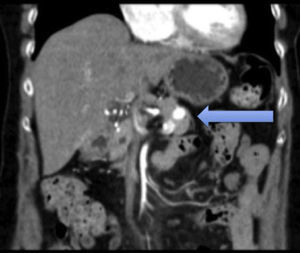
Clinical caseA case is presented of a 72-year-old female, with a history of high blood pressure and gynaeco-obstetric treatment for ovarian bleeding, 45 years ago, for which laparotomy was performed through appendectomy. She was operated on for clear cell renal cancer in the right kidney and was treated by total nephrectomy. Successive computed tomography controls were carried out, initially 6 months after surgery and subsequently each year. Three years after the right nephrectomy a hypervascular nodule was detected in the pancreatic body, which suggested the differential diagnosis between a metastasis and a primary pancreatic neuroendocrine tumour (Figs. 1 and 2).
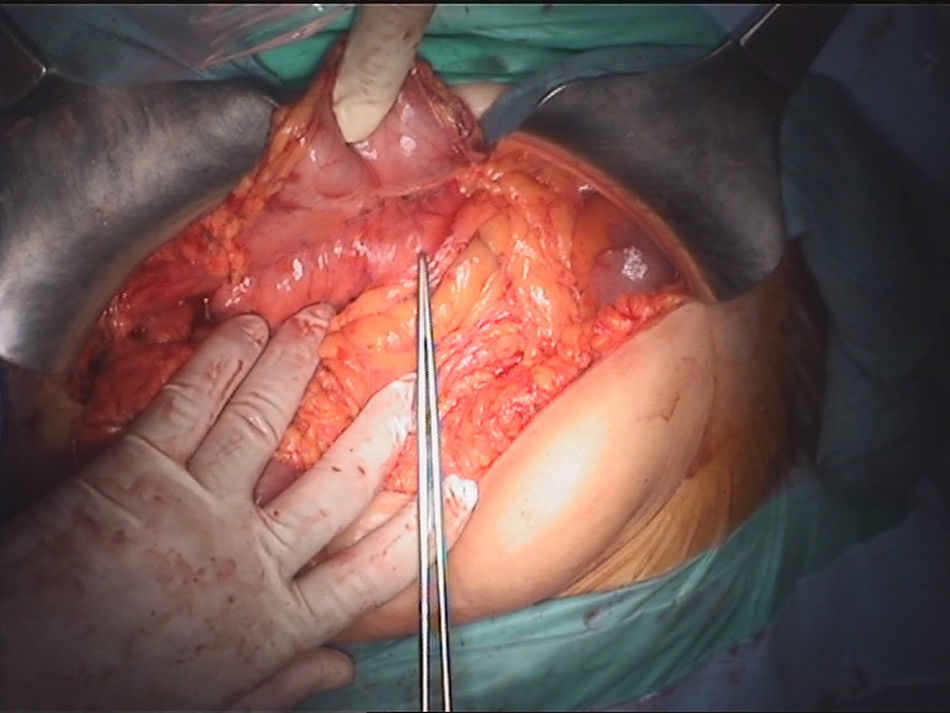
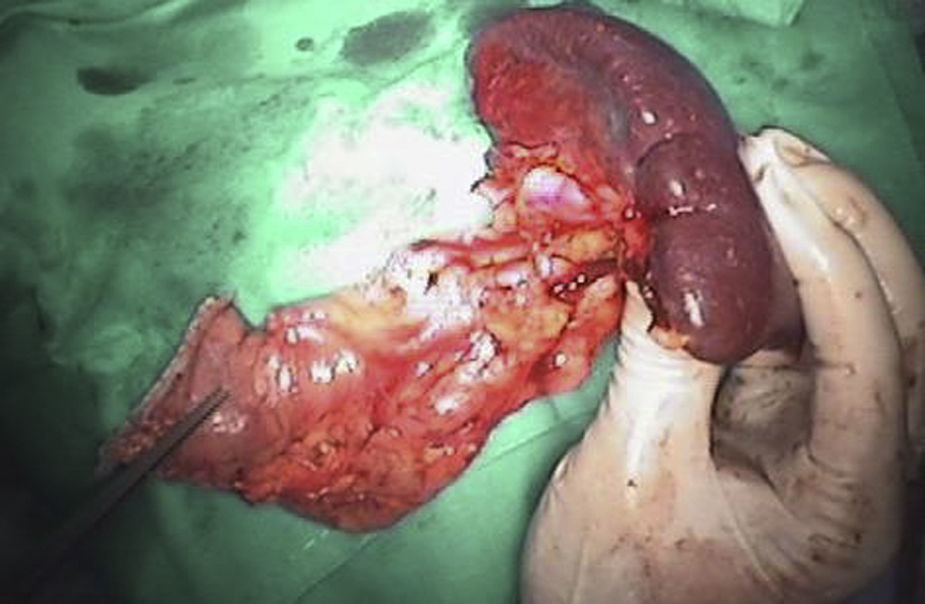
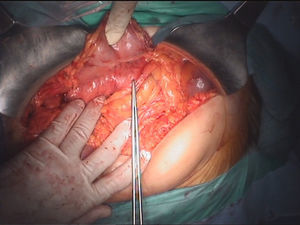
As a result of these findings, a study with complete hormonal markers and a scan were performed to rule out the primary pancreatic neuroendocrine tumour. The study of the tumour and hormonal markers tested normal. No abnormal accumulations of activity showed up in the scan to indicate the existence of lesions which express somatostatin receptors. On suspicion of pancreatic metastases due to the previous surgical background of the patient, a first diagnostic possibility was indicated to be the performing of a corporocaudal pancreatectomy with open splenectomy. During the operation and with use of a scan, a tumour of approximately 1cm in diameter was confirmed in the body of the pancreas (Fig. 3), which was later observed as a surgical specimen (Fig. 4).
The postoperative period was free from any complications and the patient was discharged 6 days after the operation. The histopathology report later confirmed metastases of renal clear cell carcinoma, with pancreatic surgical margins free from tumour infiltration. Immunohistochemical techniques were used and showed immunoreactivity in tumours cells to CD10, vimentin and CK AE1-3.
DiscussionRenal cell cancer affects patients in the sixth decade of life. The pancreas is a rare site for metastases of kidney cancer, as they are usually metachronous.5,11
There is some disagreement regarding which tumour of the body metastasises most frequently to the pancreas. Several data has been published on its distribution which are based on incidental findings during autopsies or during surgery. In one series of autopsies it was reported that the tumours which cause the most pancreatic metastases were: lung (42%), followed by gastrointestinal (24.7%) tract and kidney cancer (4%).12 However, the most frequently found tumours during surgery were mainly secondary to kidney cancer.8 Pancreatic metastasis may be located in the head of the pancreas (41%), be multifocal (22%) or diffusely affect (15%), and are usually single and large.1
The production mechanism of isolated pancreatic metastases of a renal carcinoma may be haematogenous, through porto-renal or lymphatic shunts but not for direct extension.4
Diagnosis of isolated pancreatic metastases is generally an incidental findings during follow-up of kidney cancer, since in up to 50% of cases it may be asymptomatic.1,5–10 The remainder may present as: weight loss, obstructive jaundice, abdominal pain or gastrointestinal bleeding.2
In an imaging study there are elements which may also guide diagnosis. The scan describes them as well-defined, hypoechoic nodules. Computed tomography and magnetic resonance are the techniques of choice for examining them1,3–5 and they are observed as highly vascularised tumours, the most representative of neuroendocrine or metastasic tumours, as may be appreciated in our case. In contrast, the adenocarcinoma of the pancreas is characteristically hypovascular. In our case, the main differential diagnosis within the imaging study was a tumour of neuroendocrine origin, despite there being no elements in the clinical anamnesis to warrant suspicion. Hormonal and scan tests for somtatostatin receptors enable an approximation to diagnosing this type of tumours. Positron emission tomography is used to rule out extra-pancreatic disease, and may be of great use.
When the diagnosis is uncertain, percutaneous or endoscopic biopsy with fine needle aspiration is performed, a high performance method, but there is a high risk of bleeding during the procedure and for this reason it is not usually indicated and these patients must be operated on.1,10
With the immunohistochemisty techniques these cells are immunoreactive to CD10, vimentin and CK AE1-3,1 which in our case was positive and demonstrated the metastasic origin of the renal clear cells carcinoma.
Survival of patients with kidney cancer with metastasis is poor without resection, around 10% after 5 years. The treatment of choice in pancreatic metastasis from kidney cancer is therefore radical resection, since this considerably improves the patient's chances of survival.5,6 If isolated pancreatic metastasis without extra-pancreatic extension which may be technically resected presents, it should be resected.1,2,4 The type of technique (cephalic duodeno-pancreatectomy or corporocaudal pancreatectomy) should be adapted to each case, with preservation of a maximum quantity of pancreatic parenchyma as one of the objectives and good margin resection, based on oncological criteria. No adjuvant treatment is effective in kidney cancer metastases.1
Survival rates published, after pancreatic metastases resection from kidney cancer oscillate between 12 months and 6 years with a mean of 1.3 years (the most favourable outcome is in patients with a primary pancreatic tumour).1,2
ConclusionsIsolated pancreatic metastases of kidney cancer are rare and should be distinguished from primary pancreatic tumours, especially of the neuroendocrine type since they have implications in management and prognosis. Their treatment is surgical resection, which has been shown to significantly increase survival in these patients.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Fernández RL, Fernández-González M. Diagnóstico y tratamiento de una metástasis pancreática única de un cáncer renal de células claras: a propósito de un caso y revisión de la literatura. Cir Cir. 2017;85:436–439.