The access of surgeons to liver transplant teams in Spain is heterogeneous. This study aims to portray the current human resources of Spanish transplant teams, distribution of transplant duties among team members, how transplant team members acquire their skills, their leaders’ view of their future, as well the motivations of Spanish General Surgery residents to choose transplantation as their future career choice.
MethodsTwo different surveys were created, one for head surgeons and one for residents, about the number of team members and their training, recruitment, organization of tasks and motivation to work in transplantation. The questionnaires were e-mailed to both the transplant program directors and the surgical residents.
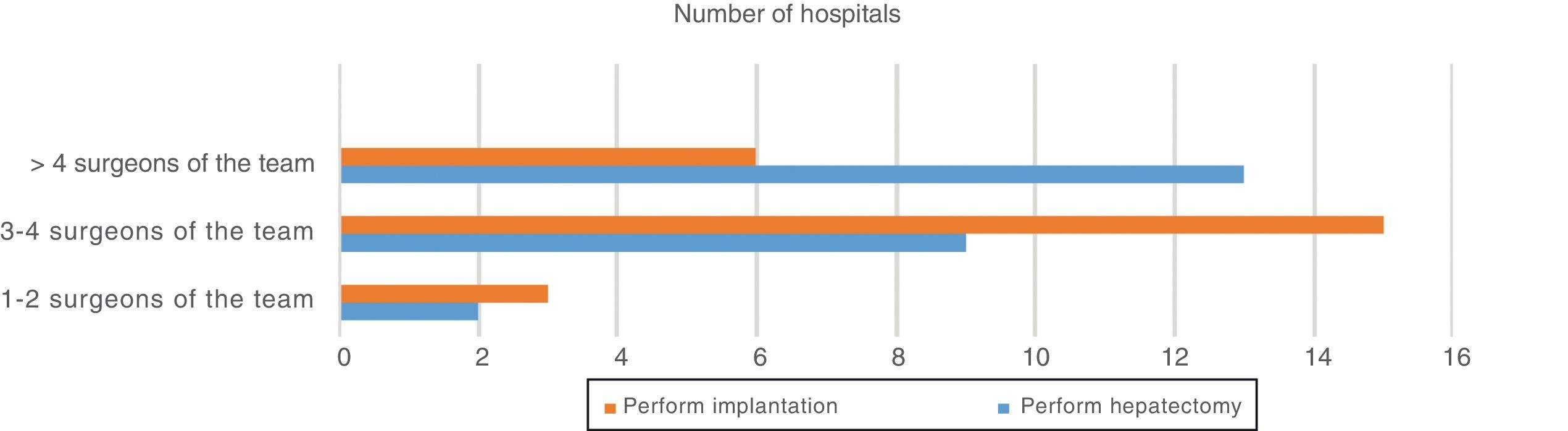
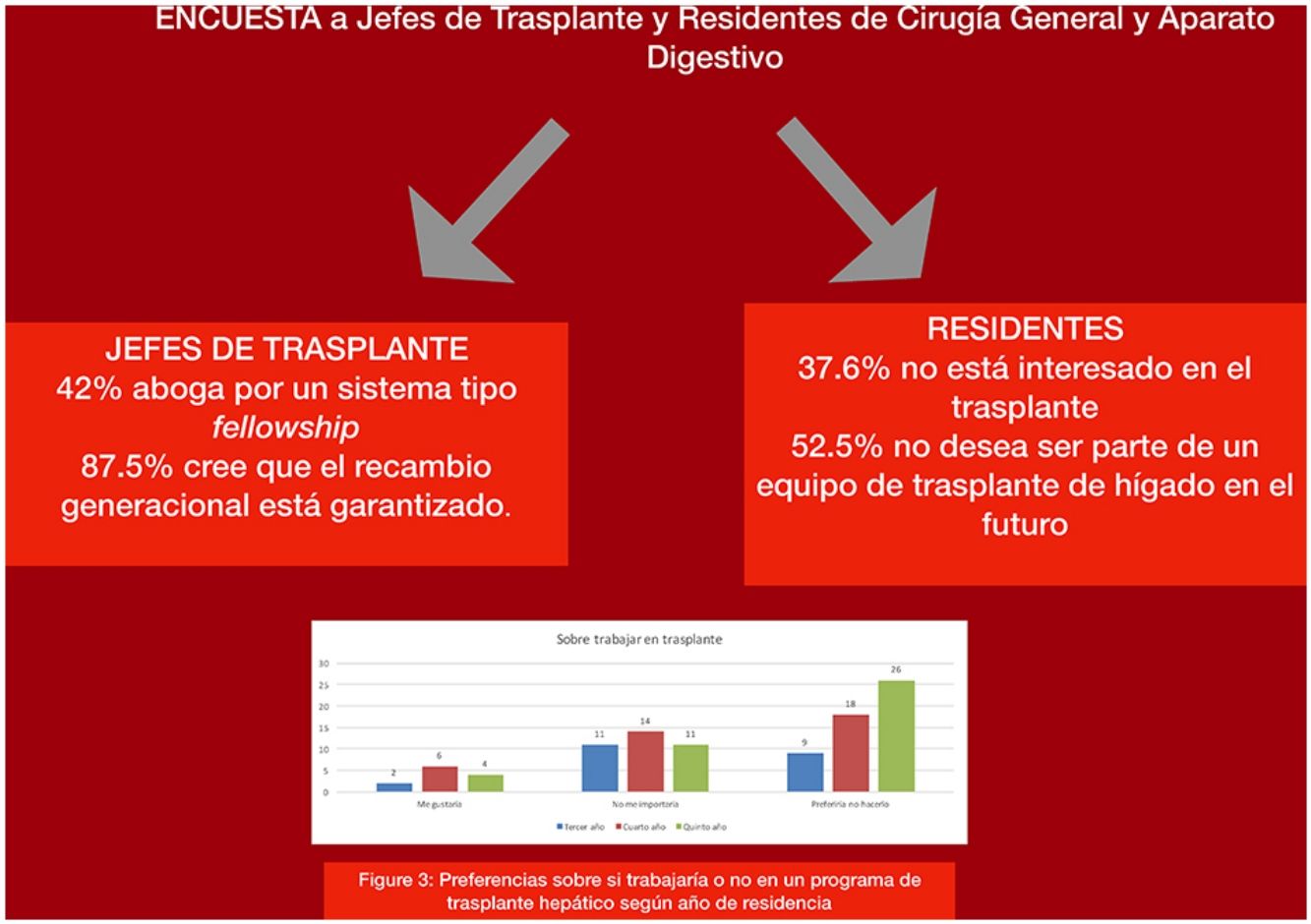
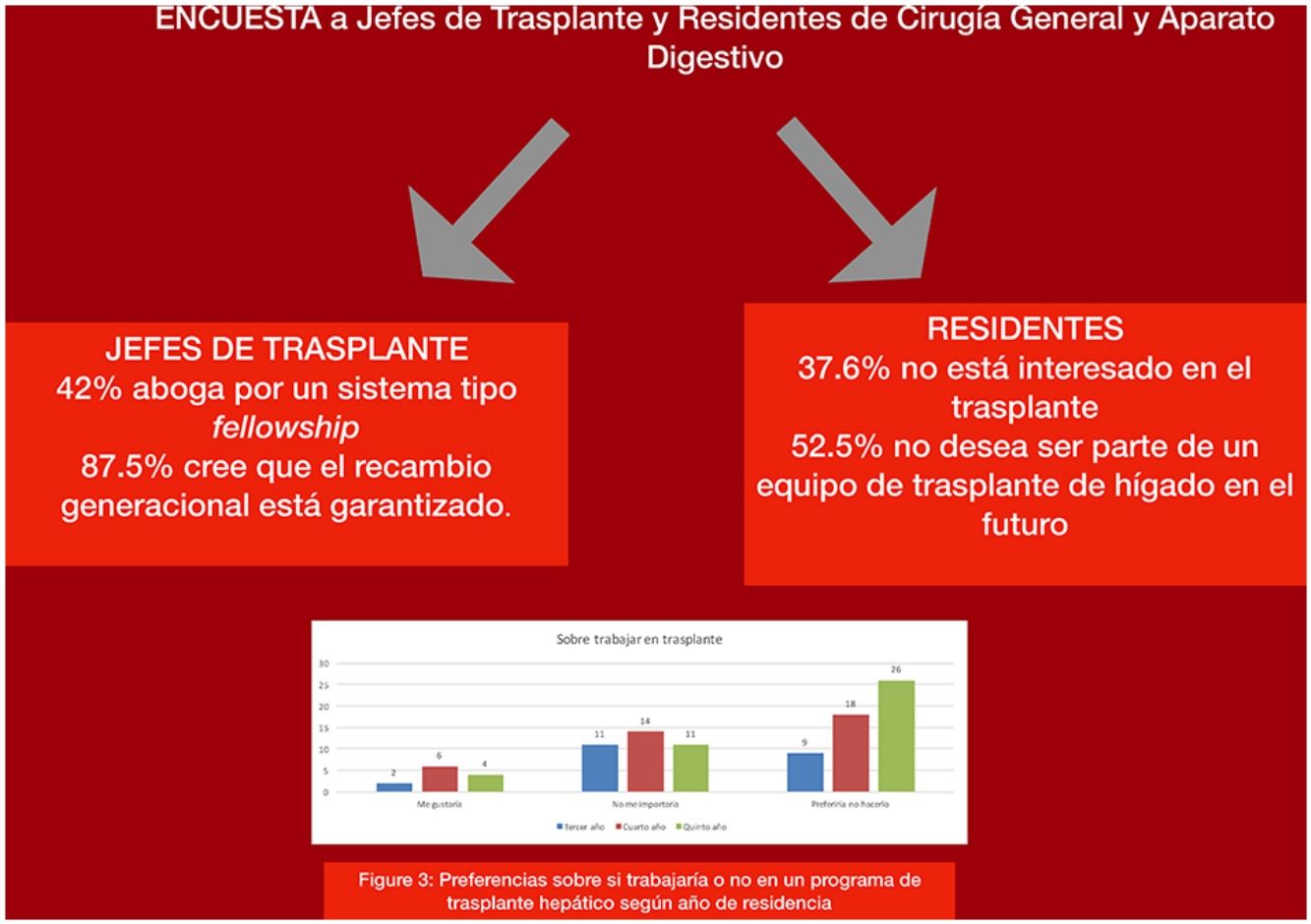
ResultsThere are on average 8 surgeons in each transplant unit. More than four surgeons perform the hepatectomy in 54.2% of the groups, while the graft implantation is performed by more than 4 surgeons at just 25% of the centers. Forty-two percent of the transplant chiefs advocated a fellowship training system, and 87.5% believe that generational turnover is guaranteed.
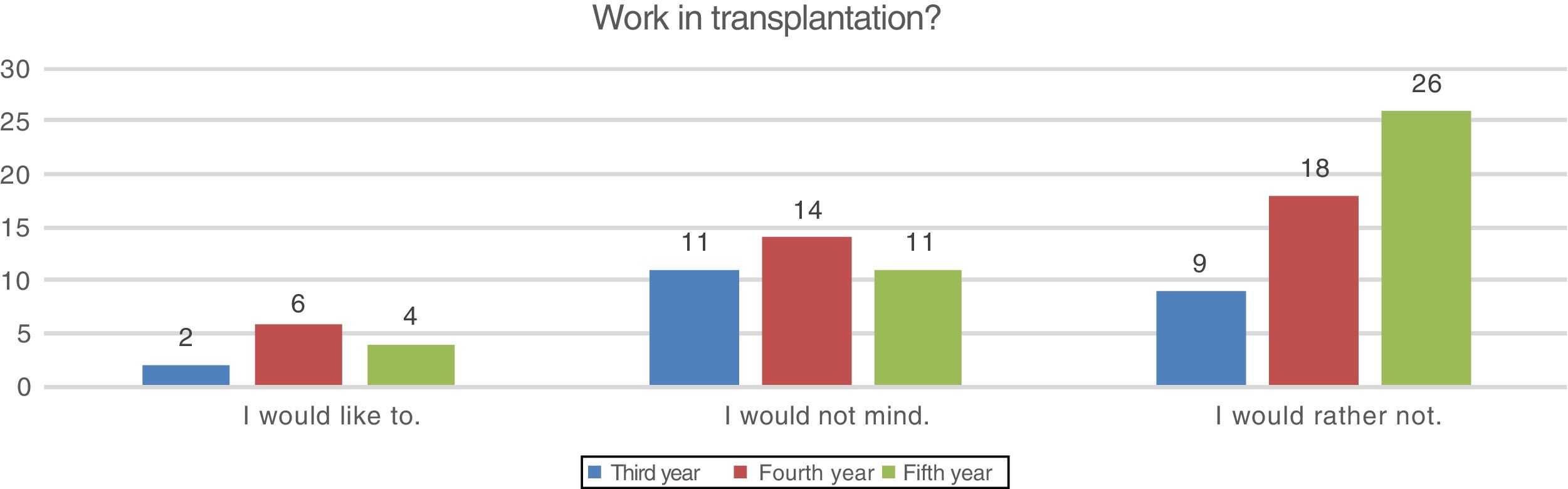
Out of 525 residents, 101 responded. Regarding training, 12.8% had no interest in transplantation. Concerning their work preferences, 37.6% were not interested in transplantation because it is excessively demanding, and 52.5% would not like to be part of a liver transplant team in the future.
ConclusionsThe generational turnover seems to be guaranteed according to liver transplant program directors. The new generations of surgeons generally opt for other areas of surgery other than transplantation. Studies with a greater number of responses are necessary to validate these results.
El acceso de los cirujanos a los equipos de trasplante hepático en España se realiza de manera heterogénea. El objetivo de este estudio ha sido cuantificar los recursos humanos de los equipos de trasplante españoles, la distribución de las diferentes tareas del trasplante entre los miembros del equipo, el mecanismo mediante el cual se adquieren las habilidades, la visión de sus líderes sobre su continuidad, así como las motivaciones de los residentes de cirugía general españoles para elegir el trasplante como su futura carrera profesional.
MétodosSe elaboraron dos encuestas diferentes, para los jefes de equipo y para residentes, sobre número de personas, capacitación, reclutamiento, organización de tareas y motivación para trabajar en trasplantes. Los cuestionarios se enviaron por correo electrónico tanto a los directores de programa de trasplante como a los residentes de cirugía.
ResultadosHay en promedio 8 cirujanos en cada unidad de trasplante. Más de 4 cirujanos realizan la hepatectomía en el 54,2% de los grupos, mientras que el implante lo realiza más de 4 cirujanos en solo el 25% de los centros. El 42% de los jefes de trasplante hepático aboga por un sistema tipo fellowship y el 87,5% cree que el recambio generacional está garantizado.
De los 525 residentes, 101 respondieron. Respecto a la formación, un 12,8% no tiene interés en el trasplante. En cuanto a sus preferencias laborales, el 37,6% no está interesado en el trasplante por ser excesivamente exigente, y el 52,5% no desea ser parte de un equipo de trasplante de hígado en el futuro.
ConclusionesEl recambio generacional parece estar garantizado según los directores de programa de trasplante de hígado. Las nuevas generaciones de cirujanos generalmente optan por otras áreas de cirugía diferentes al trasplante. Son necesarios estudios con mayor número de respuestas para validar estos resultados.
There are currently 25 active liver transplant programs in Spain that perform approximately 1200 transplantations each year.1 Unlike countries with fellowship-based training programs, where transplantation is a recognized subspecialty2 (Canada and USA), training in Spain system and other European countries is conducted by incorporating a new surgeon into the transplant team, which usually occurs according to the demand for these positions.3
Several aspects of interest related to human resources in transplant programs have caused concern,4 such as the composition of transplant teams, the availability of new, younger surgeons to be incorporated and the problem of the turnover rate. In the same way, it would be interesting to know what motivates future surgeons to choose specialization in transplantation. Likewise, it would be interesting to determine why the turnover rate is so high.5
The objective of this study was to determine the human resources of Spanish transplant teams, the distribution of different transplant tasks among the team members, the mechanism through which skills are acquired, the vision of transplant unit directors about future employment in this specialty, as well as the motivations of Spanish general and digestive surgery residents to choose transplantation as their future professional career.
MethodsA 16-question survey was created and sent to the directors of liver transplantation programs in Spain (25 surgeons). Likewise, a 12-question survey was written and sent to residents of general and digestive surgery in their last 3 years of residence (525 residents in total). Both surveys addressed issues that are considered important for accessing liver transplant programs (see Supplementary Material in Appendix B). The survey covered the structure of the program, degree of specialization, several aspects of the training process, the recruitment of new surgeons, and professional expectations and preferences. A space was included for participants to make their own comments and suggestions. Once they had been designed and discussed by the working group, both surveys were created on Google Forms. Contact with the directors of the liver transplant programs was established through the Spanish Society of Liver Transplantation (Sociedad Española de Trasplante Hepático, SETH). Contact with residents was made possible by the database maintained by the Spanish Association of Surgeons (AEC).
In a cover letter addressed to both scientific societies and potential participants, we explained the purpose of the study and encouraged their participation in the survey. Together with the cover letter, we sent an email with the link to the online survey with a request to forward it to the participating surgeons. The request for participation was sent twice, in July and September 2017.
The number of annual transplantations per hospital was collected from the annual reports of the Spanish National Transplant Organization.
The data analysis was performed using the standard descriptive statistical methodology using Microsoft Excel for Mac 15.14. The comparison between qualitative variables was performed with the chi-squared test using IBM SPSS Statistics, version 22.
ResultsSurvey for Liver Transplant Program DirectorsOut of the 25 surgeons leading the 25 liver transplant units in Spain, 24 (one woman and 23 men) answered the survey. The mean number of surgeons per transplant program is 7.20±1.75, and most units have 8 surgeons. There are no differences in the average number of surgeons in the unit according to the annual volume of transplants being less than or greater than 50 cases (7 vs 7.5; P=.49). Regarding the age of surgeons, in 13 of the 25 teams there are more than 3 surgeons over the age of 55, and in one unit all the surgeons are younger than 55. In terms of experience, 78.9% of the teams have only one or 2 surgeons with less than 5 years of experience.
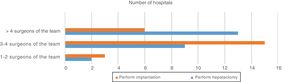
Considering the role of surgeons within the transplant team, 83.3% of the teams have surgeons who no longer regularly perform organ procurement surgery. In most teams, donor surgery is performed by any of the team members, or there is an independent group of surgeons for this purpose. As for recipient surgery, in 54.2% of the groups, more than 4 surgeons can perform hepatectomy (42.9% vs 70% [P=.29] when we consider groups that perform less than 50 transplants per year or more than 50, respectively). However, the liver implantation is performed by more than 4 surgeons in only 25% of the teams (21.4% vs 30% [P=.291] when we consider groups that perform less than 50 transplants per year or more than 50, respectively) (Fig. 1). Half of the respondents consider that the appropriate number of surgeons on each team capable of performing liver transplantation autonomously should be 4, 25% think the correct number is 3, 20.8% more than 4 and only 4.2% think that 2 surgeons are enough.
The hiring of a new surgeon for the team depends on the decision of the head of the service, the head of the transplant unit or the hospital administration in 62.5% of the cases. Hiring through a job bank without considering the former occurs in 20.8% of hospitals. Only 10 medical centers claim to have the capability to hire surgeons independently to fill positions in order to attract talent.
With regard to training, 41.7% of the directors of transplant units advocate a fellowship-type training system to generate a group of trained surgeons suitable for hiring. Another 41.7% think that training should be carried out in accordance with employment needs as they arise. Furthermore, 52.2% of program directors acknowledge having facilities to send a surgeon from their group to another place for a period of time to train.
When asked about the generational turnover, 87.5% of the respondents believe that this is guaranteed in the transplant program they manage, and 54.2% had met with hospital administrators to discuss this matter. Four directors think that the younger surgeons and residents at their hospital have no interest in joining the transplant team.
In the comments section of the survey, the issues that were repeated most frequently were training, effort, dedication, continuity and progressivity.
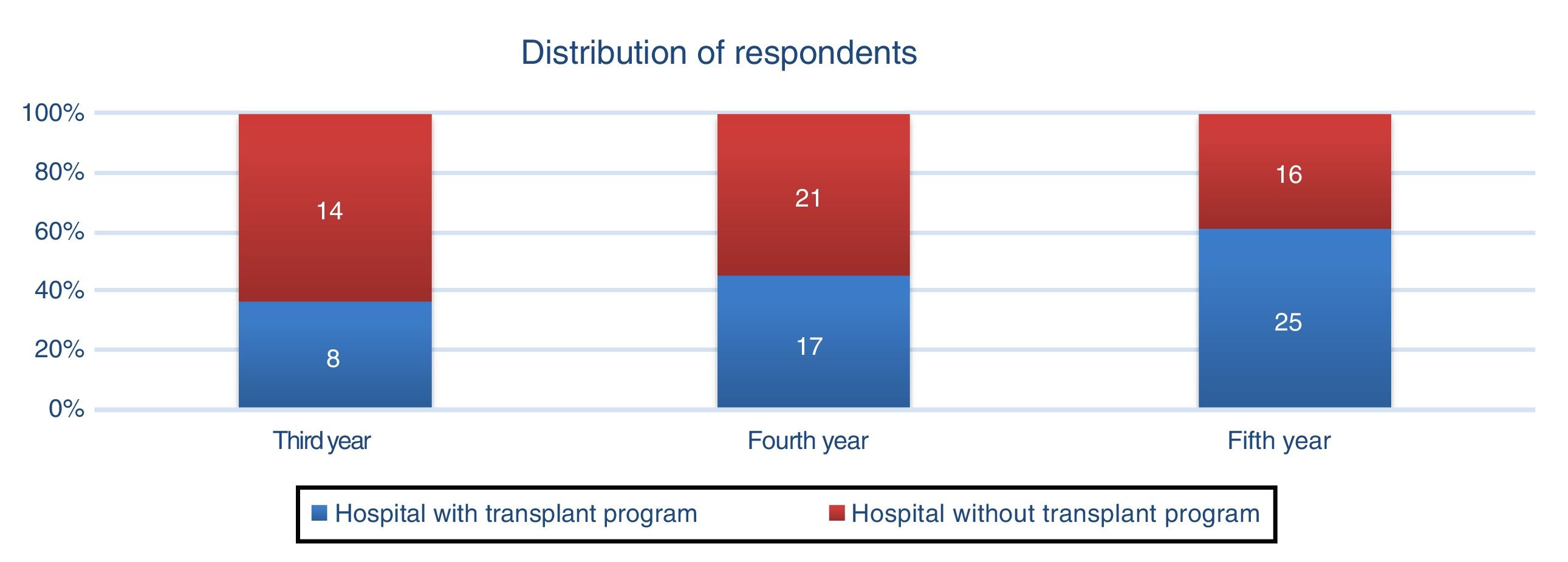
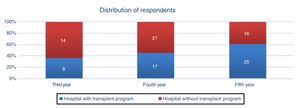
Survey for Surgery ResidentsOut of the 525 residents to whom the survey was sent, 126 reviewed it and only 101 (19.24% of the total residents and 80.16% of those interested) returned it completed. Interestingly, 51 (50.5%) of the 101 respondents were residents at hospitals without a liver transplant program. The distribution by year of residence and type of hospital is presented in Fig. 2.
As for liver transplantation training during residency, 87.2% had had some sort of contact with a transplant program, either at their own hospitals or rotating at another hospital through commissioned training programs. Even so, 12.8% said they had no interest in training in transplantation and did not plan to do any related rotations.
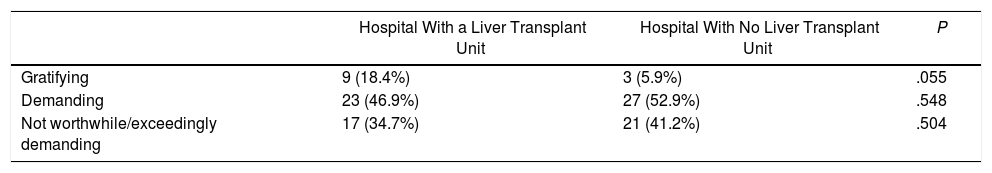
A series of questions were asked to explore opinions about transplantation and the possibility of considering it a career option. Opinions about transplantations were evaluated through 3 possible answers: it is a rewarding activity (11.9%), it is demanding (50.5%), and it is not worthwhile because it is exceedingly demanding (37.6%). There were no statistically significant differences in the responses from residents, regardless of whether or not they had a liver transplant unit at their hospital (Table 1).
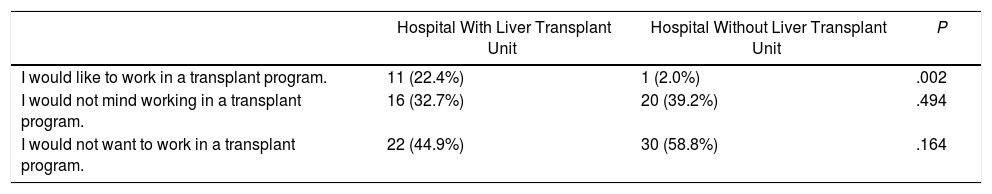
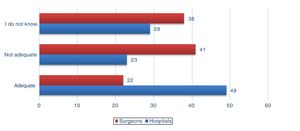
Participants were also asked whether they considered transplantation a well-paid activity. While 19.8% considered that it is, half of the residents (50.8%) said they did not know. When we asked about what aspect they would value most when choosing to work in a transplant program, economic compensation was the option chosen by only 13%, while 45% would choose it for potential professional development. Teamwork was the least valued factor (8%). Regarding whether they would like to work in a liver transplant unit in the future, 52.5% of residents said they would rather not (Fig. 3). Differences of opinion, depending on whether the residents were training in a hospital with or without a transplant program, are shown in Table 2.
Opinion About Working With a Liver Transplant Program in the Future According to the Type of Hospital Where the Resident Is Completing Their Residency.
| Hospital With Liver Transplant Unit | Hospital Without Liver Transplant Unit | P | |
|---|---|---|---|
| I would like to work in a transplant program. | 11 (22.4%) | 1 (2.0%) | .002 |
| I would not mind working in a transplant program. | 16 (32.7%) | 20 (39.2%) | .494 |
| I would not want to work in a transplant program. | 22 (44.9%) | 30 (58.8%) | .164 |
Regarding the availability of work at the end of residence in a liver transplant unit, 10% responded that they considered it accessible, specifically 12.2% of hospital residents with a transplant program and 7.8% of those residents without a transplant program at their hospital (P=.463).
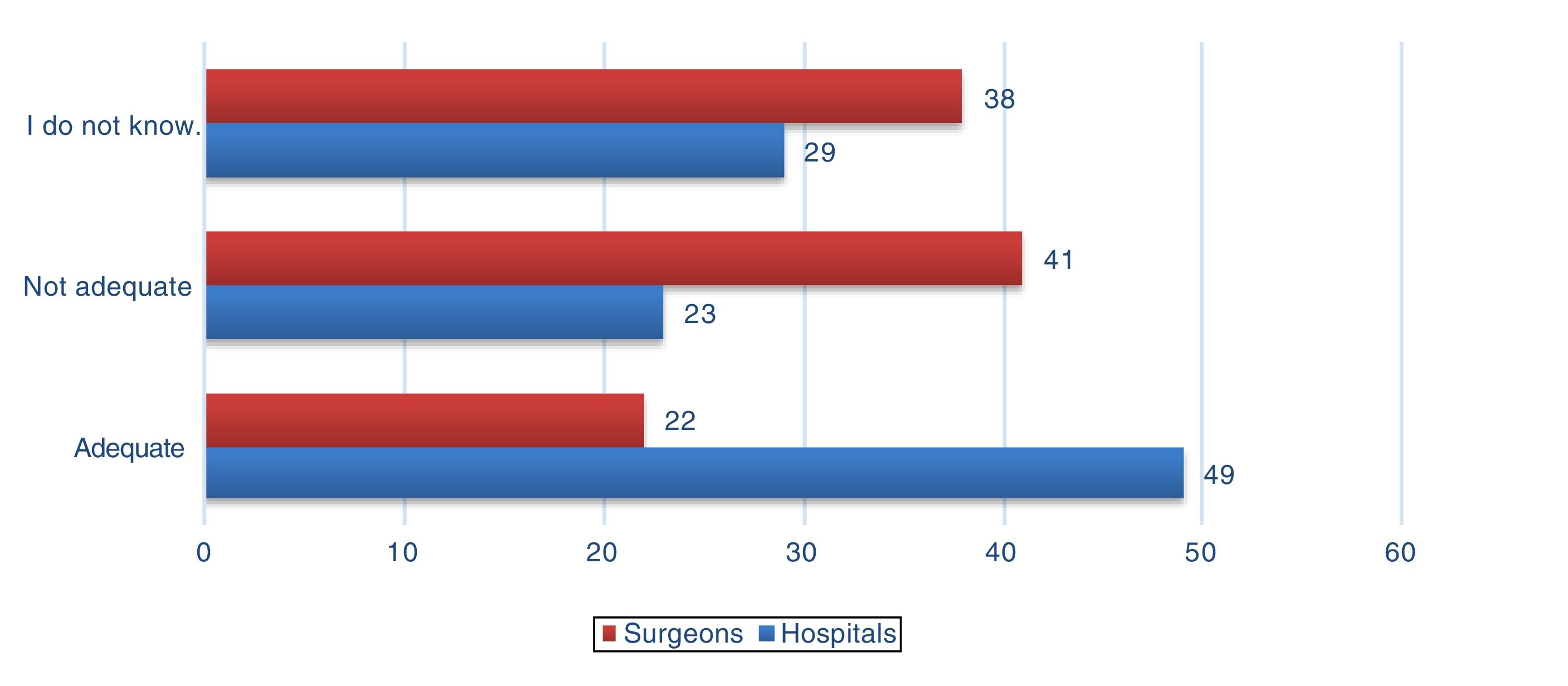
Finally, we investigated the opinion on whether the number of medical centers and surgeons performing liver transplantation in Spain are considered adequate (Fig. 4).
In the comments section of the survey, the most frequently mentioned aspects were: quality of life, reconciling their professional and personal lives, night shifts and access for young surgeons.
DiscussionIn Spain, transplant surgery is currently not an officially-recognized specialty and remains a subspecialty of general surgery. This situation is similar to that of other European countries like Germany, for example.3 There are few training opportunities as training in transplant surgery is mainly provided as part of general surgical training.
The way in which a surgeon agrees to work in a transplant unit and the distribution and organization of work within each unit is not officially regulated and can vary widely from place to place. To our knowledge, a survey on these factors has not been conducted with liver transplant directors in Spain. The survey was created for unit directors because they are a well-defined and easily-located group, and because, for most of the questions asked of an objective nature about the operation and structure of the groups, we thought it was sufficient for one person from each unit to respond. On the other hand, it seems important to determine the opinion of future surgeons about liver transplantation as a career option. It is known that a major problem worldwide in the field of liver transplantation is to ensure our patients the continuity of surgical skills and competence,6 a concern that is likely shared by other medical disciplines.
The number of surgeons who are part of adult liver transplant teams throughout Spain is 173. We do not know the total number of surgeons currently working in Spain, but there are about 6000 members of the Spanish Association of Surgeons, which is the main association in this country, so it probably includes most of them. The low number of transplant surgeons compared to the total could be indicative of the high level of specialization that is necessary in this area of surgery.
As for the distribution of work within the teams, it is staggered with initial access through donor surgery, which is performed by most surgeons in transplant units in Spain. A smaller number of surgeons perform the hepatectomy in the recipient, and this number is further reduced when we consider the graft. Almost 10 years ago, it was considered necessary to initiate certification mechanisms for programs and surgeons.7 However, to date, the accreditation of surgeons remains voluntary. The mechanism by which the members of the transplant team in Spain acquire their skills is not through a fellowship system, in which there is regulated content and an established schedule, but instead the system of knowledge transmission by veteran surgeons in the specific transplant group, with no associated training program.
In Spain, according to our study, more than half of the teams have 3 or more surgeons over the age of 55. Taking into account the average number of surgeons per unit and that the retirement age is 65, within the next 10 years almost half of the current human resources will leave transplant surgery teams and will need to be replaced. We should realize that there will be problems to train and certify this new staff in such a period of time; in fact, the Florence et al. study concludes that, among surgeons, the transplant subspecialty group is highly trained and qualified, as reflected in the more than 15 years of higher education and formal clinical training.8 However, in Spain, given that there are few surgeons with less than 5 years of experience on the teams (more than 80% of them only with one or 2 of the surgeons with less than 1–2 years of experience), it is also inferred that there is staff with high experience time and that could guarantee continuity.
In general, the directors of transplant units consider that generational turnover (natural replacement of retirees with younger surgeons) is guaranteed at their hospitals, since there are young surgeons interested in liver transplantation; meanwhile, 17% believe that young surgeons have no interest. In our opinion, the generational turnover should not be considered completely resolved. Instead, it should be periodically reassessed to avoid problems in the future. Normally, to hire a new surgeon to join the team, the opinion of the head of the transplant program is considered, although it is alarming that in 20% of hospitals that opinion is not taken into account and a new contract is established from a job bank, in which the merits and skills related to transplantation are hardly considered, if at all. The potential impact of this factor is unknown, since a career in transplantation requires a great deal of motivation and dedication, especially given the long work hours, burnout rates, work-related conflicts at home, etc.9,10
Regarding the training of future transplant surgeons, half of the unit directors think that there should be a group of surgeons trained in transplantations who can be hired when necessary, while the remainder argue that they should only be trained when the need to fill a position on the team arises, or if the need is anticipated. The main risk of having a shortage of surgeons trained in organ transplantation is not being able to meet an unexpected demand in the near future. In contrast, if we train too many transplant surgeons, the market may become saturated and there will not be enough jobs to fill the demand.11 The question of whether a country is training an adequate number of transplant surgeons is not easy to answer. In their study, Scarborough et al. estimated the current and future number of surgeons performing liver transplantation in the US.12 They concluded that the number of liver transplant procedures per surgeon and the relationship between the supply and demand of surgeons would remain relatively stable until 2020. However, other authors have considered that there could be too many training positions for future demand.13
As for the residents’ survey, we decided to send it to residents who are toward the end of their residency, thinking that most of them, by that time, would have already completed a transplant training period or would have planned to do so in the near future. As far as we know, a survey has not yet been conducted in which Spanish residents are asked their opinion on working in liver transplantation.
It is surprising that 12.8% of respondents had not done nor planned to do a training rotation in transplantation. This makes us wonder whether this training should be promoted, and how. The opinion of most residents about transplantation is that it is demanding and even that it does not compensate for being exceedingly demanding. Certainly, the quality of life of transplant surgeons is a very frequently repeated argument in the literature as one of the limiting factors to make it more professionally attractive.8,9,14
Another interesting aspect of this survey is that very few residents consider teamwork a motivation to specialize in transplantation (8%). The reason why most would choose it is because of the potential for professional development. In fact, it is known that transplantation has a significant impact on the development of other complex surgeries and on the treatment of more complicated patients in general.15
In addition, there is a clear difference in the response to the desire to work in the future in a liver transplant program between the residents at hospitals with a transplant program and residents at hospitals with no program, as more positive responses were given by those at hospitals with a transplant unit. This response leads us to believe that it is necessary to provide surgical residents in Spain more information and a better explanation of liver transplantation activities.
More than half of the residents stated they would not want to make transplantation their future career. When they were asked to explain why, and what aspects of transplantation work they would change, the main arguments given were night shifts, reconciling their personal/professional life, and quality of life. These same arguments have also been reported by other authors.5,15,16 Access to specialized medical training in Spain is currently carried out based on the level of theoretical knowledge determined by an entrance exam. However, other qualities are not contemplated, which may be essential for professional practice in general or specific to each of the specialties. This can occasionally lead to frustration and dissatisfaction because the expectations are not satisfied.
Regarding the limitations of our study, we must state that, although we have obtained a high response rate from the directors of liver transplant programs (nearly 100%), the low response rate obtained from residents is a very important limitation that could generate biased results due to non-response bias. Therefore, the strength of our conclusions is affected. While it is true that the low survey response rate is in the range reported for other surgical human resources surveys (3%–34%),8 having such a small number of responses can seriously modify the results. The actual cause of this low response rate could not be determined as it is not because of a refusal to respond to a part of the survey, as in some studies with survey methodology.17 Instead, there was an overall lack of completion of the survey. We cannot determine how many of the 525 residents to whom it was sent actually received the email or the reason why they did not respond; all we know is that 101 of the 126 (80.16%) residents who were interested in opening it responded. It probably reflects a certain degree of distancing from transplantation due to the reasons previously stated or due to the few positions available in transplantation, which makes it unattractive even to answer a survey on employment aspects. Another limitation is not having compiled the gender of the residents, since there could be certain gender-related differences of opinion.18 In addition, due to the anonymous nature of the questionnaire, we cannot directly link the responses to a particular transplant center. Moreover, in the survey for unit directors, there are certain questions of a subjective nature for which the responses from more participants would add value; thus, a survey addressed to all transplant surgeons, regardless of their position, should be a future line of study.
Access to employment in transplant units is limited due to the small number of surgeons involved in these programs. The generational turnover seems to be guaranteed according to the opinion of liver transplant program directors in Spain. Nevertheless, new generations of surgeons seem to prefer specialization in other areas of surgery because of the lifestyle and the difficult reconciliation between work and family life. Thus, future strategies should be developed to resolve these issues in order to ensure that surgeons choose a career in transplantation.
These results should be interpreted with caution, and more studies are needed with higher response rates.
FundingThis study has received no specific funding from public, commercial or non-profit entities.
Conflict of InterestsThe authors have no conflict of interests to declare.
The authors would like to thank the Spanish Society for Liver Transplantation (Sociedad Española de Trasplante Hepático, SETH) and the Spanish Association of Surgeons (Asociación Española de Cirujanos, AEC).
Spanish Working Group for Liver Transplantation:
Diego López-Guerra: Servicio de Cirugía Hepatobiliopancreática y Trasplante Hepático, Hospital Universitario de Badajoz, Spain
Gonzalo Rodríguez-Laiz: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital General Universitario de Alicante, Spain
Jesús Villar-del-Moral: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Universitario Virgen de las Nieves, Granada, Spain
Fernando Pardo Sánchez: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático. Clínica Universitaria de Navarra, Pamplona, Spain
Julio Santoyo: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Regional Universitario de Málaga, Spain
Rafael López Andújar: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Universitario y Politécnico La Fe, Valencia, Spain
Javier Nuño: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Universitario Ramón y Cajal, Madrid, Spain
Víctor Sánchez Turrión: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Universitario Puerta de Hierro, Majadahonda, Spain
Ignacio González Pinto: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Universitario Central de Asturias, Oviedo, Spain
Carlos Jiménez: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante de Órganos Abdominales, Hospital Universitario 12 de Octubre, Madrid, Spain
José Ángel López Baena: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital General Universitario Gregorio Marañón, Madrid, Spain
Manuel Gómez Gutierrez: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Complejo Hospitalario Universitario La Coruña, Spain
Joan Fabregat Prous: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Universitario de Bellvitge, L’Hospitalet de Llobregat, Spain
David Pacheco Sánchez: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Universitario Río Hortega, Valladolid, Spain
Manuel Barrera: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Universitario Nuestra Señora de la Candelaria, Santa Cruz de Tenerife, Spain
Agustín García-Gil: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Clínico Universitario Lozano Blesa, Zaragoza, Spain
Pablo Ramírez: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Clínico Universitario Virgen de la Arrixaca, Murcia, Spain
Evaristo Varo: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante de Órganos Abdominales, Hospital Clínico Universitario de Santiago, Santiago de Compostela, Spain
Itxarone Bilbao: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Universitario Vall d’Hebron, Barcelona, Spain
Constantino Fondevila: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Clínic, Barcelona, Spain
Juan Carlos Rodríguez-Sanjuan: Servicio de Cirugía General y del Aparato Digestivo, Unidad de Trasplante Hepático, Hospital Universitario Marqués de Valdecilla, Santander, Spain
Please cite this article as: Blanco Fernández G, Gómez Bravo MÁ, Briceño Delgado J, Valdivieso López A, Grupo Español de Trabajo sobre Trasplante Hepático. Encuesta a los jefes de Unidad y residentes de Cirugía sobre la accesibilidad y el trabajo en los equipos de trasplante hepático en España. Cir Esp. 2019;97:560–567.
The names of the components of the Spanish Working Group for Liver Transplantation are listed in Annex 1.