Currently, intersphincteric ultralow anterior resection of the rectum with manual coloanal anastomosis is accepted treatment in selected cases of Rullier II and III neoplasms of the lower rectum.1,2
Prolapse of the coloplasty after anterior rectal resection is a rare complication, with an incidence close to 2.2% in the open approach. The incidence is slightly higher when the approach is done laparoscopically or robotically (6.4%).3
Classically, the treatment for coloanal anastomosis prolapse consisted of abdominoperineal resection.
We report the case of a 61-year-old woman with a history of smoking, grade I obesity and tubal ligation, who was diagnosed with low rectal cancer after a fecal occult blood test. Colonoscopy revealed a lesion, whose biopsy was compatible with low-grade adenocarcinoma, 1 cm proximal to the pectineal line. On pelvic MRI, the lesion was observed to be a bilateral posterior and anterolateral tumor of more than 75% of the circumference and 3.5 cm in length. There was invasion of the entire thickness of the internal anal sphincter, but no signs of invasion of the intersphincteric space, and 5 mesorectal lymphadenopathies were in contact with the mesorectal fascia (Rullier III cT3N2M0). Endoanal ultrasound could not be performed due to pain. In the directed anamnesis, the patient reported good baseline continence (0 points on the Wexner scale) and history of an uneventful vaginal delivery. Upon physical examination, which was limited due to pain, the patient presented good tone, contractility, and preserved reflexes.
The patient received neoadjuvant radiochemotherapy. The restaging MRI showed reduction of the tumor and lymphadenopathy (persisting extramural extension). Distant metastatic involvement was ruled out (Rullier II and cT3N0M0). Surgery was indicated, and we proposed two options: Miles’ abdominoperineal resection or sphincter-preserving surgery with total transanal mesorectal excision (TaTME). The patient opted for the latter.
Complete intersphincteric resection was performed by TaTME surgery, including a manual end-to-end coloanal anastomosis with protective ileostomy. The postoperative patient progress was good, without complications, and she was discharged on the seventh day.
During the subsequent follow-up, the patient presented a good general condition but poor adaptation to the ileostomy. The physical examination was normal. Pathology results reported free margins and optimal mesorectal quality, with final staging ypT1N0.
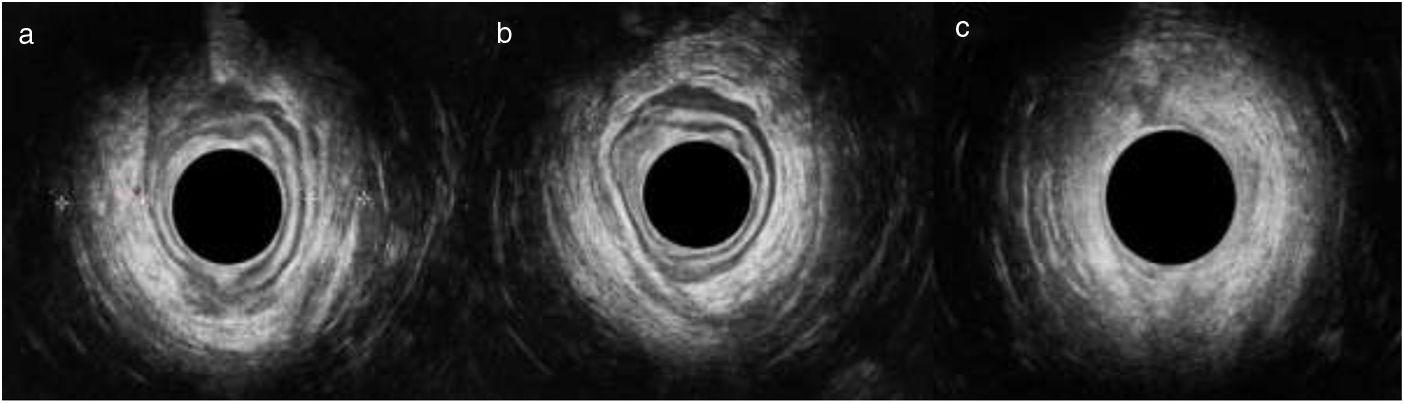
Four months later, the patient presented with spontaneous rectal prolapse, complete with the Valsalva maneuver. Rectal examination revealed the absence of masses and, together with manometry, severe hypotonia. A colonoscopy study ruled out other lesions, and the endoanal ultrasound showed asymmetry of the puborectalis branches (right 12 mm and left 9 mm), absence of an internal anal sphincter and a complete external anal sphincter, with thinning of the left quadrants (Fig. 1).
Endoanal ultrasound for the study of the prolapse: a) upper anal canal showing asymmetry between the right and left branches of the puborectalis muscle; b) middle anal canal showing thinning of the external anal sphincter in the left quadrants; c) lower anal canal showing no alterations.
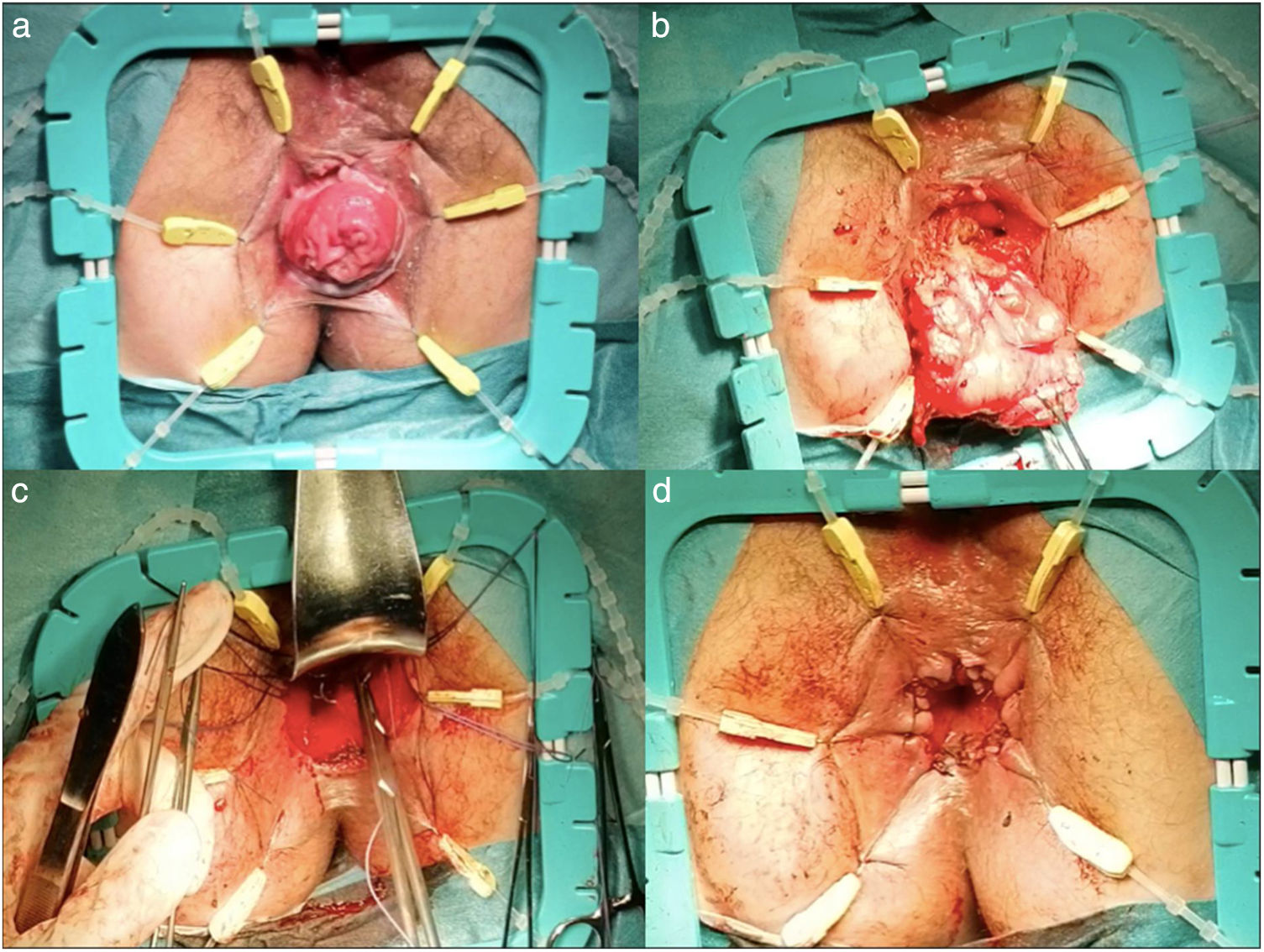
Given the coloplasty prolapse together with the severe hypotonia, we performed prolapse surgery without a definitive colostomy, in accordance with the Altemeier technique.4 The surgery involved resection of the coloplasty about 7−8 cm below the previous anastomosis and end-to-end coloanal anastomosis with posterior levatorplasty, with no incidents and good retraction of the repair (Fig. 2). The patient was discharged on the second postoperative day, and the ileostomy was closed 3 months later. In subsequent check-ups, the patient has been in good general health, with a score on the LARS scale of 23 points (minor LARS).5
Sphincter-preserving surgery for lower rectal cancer is an option whose use is increasing in our setting, with different approaches that include the robotic approach and the TaTME approach.6 TaTME surgery should be performed by teams with established training.7 Even when the criteria are met, related complications have been reported. Rectal prolapse related with ultra-low resections is a rare complication, associated with poor anorectal function, including incontinence, exudation, and anal pain.8
Factors related to the incidence of colon prolapse after intersphincteric resection have been described, such as advanced age, female sex, and neoadjuvant radiotherapy.3
When treating a patient with rectal prolapse, especially after cancer surgery, the study before surgical indication should rule out recurrence and make a dynamic sphincter evaluation.
There are multiple surgical approaches for the treatment of similar cases, whose objectives are to preserve anorectal function and avoid a definitive colostomy. The techniques described by Delorme and Altemeier, rectopexies, or another resection via the abdominal route are examples.9,10 In our experience, the Altemeier technique could be one to keep in mind, although there are no randomized clinical trials or case series with long-term follow-up.
Please cite this article as: Maldonado Marcos E, Planellas Giné P, Gil Garcia J, Farrés Coll R, Codina Cazador A. Procedimiento de Altemeier para la reparación de prolapso rectal tras resección anterior de recto interesfinteriana con escisión mesorrectal total por vía transanal. Cir Esp. 2021;99:389–391.