Circular mucosal anopexy (CMA) achieves a more comfortable postoperative period than resective techniques. But complications and recurrences are not infrequent. This study aims to evaluate of the efficacy of CMA in the treatment of hemorrhoids and rectal mucosal prolapse (RMP).
MethodFrom 1999 to 2011, 613 patients underwent surgery for either hemorrhoids or RMP in our hospital. CMA was performed in 327 patients. Gender distribution was 196 male and 131 female. Hemorrhoidal grades were distributed as follows: 28 patients had RMP, 46 2nd grade, 146 3rd grade and 107 4th grade. Major ambulatory surgery (MAS) was performed in 79.9%. Recurrence of hemorrhoids was studied and groups of recurrence and no-recurrence were compared. Postoperative pain was evaluated by Visual Analogical Scale (VAS) as well as early complications.
ResultsA total of 31 patients needed reoperation (5 RMP, 2 with 2nd grade, 17 with 3rd grade, 7 with 4th grade). No statistically significant differences were found between the non-recurrent group and the recurrent group with regards to gender, surgical time or hemorrhoidal grade, but there were differences related to age. In the VAS, 81.3% of patients expressed a postoperative pain ≤2 at the first week. Five patients needed reoperation for early postoperative bleeding. Six patients needed admission for postoperative pain.
ConclusionsRecurrence rate is higher in CMA than in resective techniques. CMA is a useful technique for the treatment of hemorrhoids in MAS. Pain and the rate of complications are both low.
La anopexia mucosa circular (AMC) condiciona un postoperatorio menos molesto que las técnicas resectivas, pero no está exenta de complicaciones y presenta una mayor recidiva. El objetivo del presente estudio es evaluar la eficacia de la AMC en el tratamiento de las hemorroides y del prolapso mucoso rectal (PMR).
MétodosEntre 1999 y 2011 fueron intervenidos en nuestro hospital 613 pacientes por hemorroides o PMR: en 327 casos se realizó AMC (PMR en 28 casos, grado II en 46, grado III en 146 y grado IV en 107 casos). La AMC se realizó en régimen de cirugía mayor ambulatoria (CMA) en el 79% de los casos. Consideramos la recidiva y comparamos los grupos de no recidiva y recidiva. Evaluamos el dolor medido por Escala Visual Analógica (EVA) y las complicaciones postoperatorias.
ResultadosEn 31 pacientes se registró recidiva de la sintomatología que precisó algún tipo de intervención: PMR en 5 pacientes, grado II en 2, grado III en 17 y grado IV en 7. No existieron diferencias significativas entre los pacientes con reccidiva y los pacientes sin recidiva en cuanto a género, tiempo operatorio ni grado hemorroidal, pero sí respecto a la edad. El 81,3% de los pacientes expresó dolor ≤2 en EVA a la semana. Cinco pacientes se reintervinieron por sangrado postoperatorio inmediato. Seis pacientes precisaron ingreso por dolor postoperatorio.
ConclusionesLa recidiva en la AMC es superior a la de las técnicas resectivas. La AMC es una técnica útil para el tratamiento de la enfermedad hemorroidal en régimen de CMA. El grado de dolor y las complicaciones son bajos.
The resection of prolapsed tissue has been the surgical treatment of choice for hemorrhoid pain since its initial description by Milligan in 1937,1 with the addition of later technical variations such as that by Ferguson.2 Resection techniques are highly effective in terms of later recurrences,3,4 but they are associated with intense postoperative pain.
Stapled anopexy (SA) was described by Longo in 1996 for the treatment of hemorrhoids and rectal mucosal prolapse (RMP) with the aim to reduce postoperative pain.5 It is based on the theory by Thompson,6 who proposed that the appearance of symptomatic hemorrhoids was caused by the degeneration of the hemorrhoidal support tissue and the anal mucosa itself.
The objective of SA is to re-establish the anatomic physiology of the anal canal in order to correct the prolapse of the rectal mucosa. This stapling is done above the pectineal line and far from the pain receptors situated in the anoderm.5 SA involves shorter hospitalisation, less postoperative pain, higher patient satisfaction,7,8 greater cost-effectiveness and shorter absences from work.8 In fact, SA is done in the Major Ambulatory Surgery (MAS) unit at many hospitals.9
Nonetheless, SA has a recurrence rate that is higher than resection techniques8,9 and serious complications have been reported.10 These circumstances have led several groups to be critical of this technique.11,12
The objective of this present study is to evaluate the efficacy of SA in the treatment of hemorrhoids and RMP. As secondary objectives, we also assessed pain and the incidence of postoperative complications, specifically haemorrhage requiring intervention and alterations in defaecation or urination.
MethodsWe conducted a retrospective, longitudinal, observational study of our experience in the treatment of hemorrhoids and RMP with SA. RMP was defined as the protrusion of the rectal mucosal and submucosal layers, with absence of hemorrhoidal tissue. Between February 1999 and December 2011, 613 patients were treated at Hospital de Mataró, 327 of which (53%) underwent SA. In 278 cases, the surgical interventions were performed by 2 members of the Colorectal Surgery Unit of the General and Digestive Surgery Department who had initiated the implementation of this technique at our hospital (either by performing the surgery themselves or by supervising residents). The remaining operations were done by other members of the unit.
The surgical technique utilised has been previously published by our group,13 based on the initial technique by Longo.5 For SA, the PPH-01 device (Ethicon-EndoSurgery, Bracknell, United Kingdom) was used, which was later substituted by the PPH-03 device. Antibiotic prophylaxis was always administered (80mg gentamicin and 500mg metronidazole). Routine histopathology studies were done of the resected tissue.
The operations were conducted in the MAS setting in 261 cases (79.8%). The postoperative analgesia protocol involved 50mg of oral diclofenac every 8h or 2g of oral metamizole every 8h, alternating with 1g of oral paracetamol every 8h, with the administration of 50mg of tramadol as rescue analgesia. The treatment was maintained for 3 days, and the patient was free to stop treatment beforehand if he/she felt no pain. The degree of pain was quantified with a Visual Analogic Scale (VAS) one week after the intervention.
The postoperative follow-up included visits in the outpatient office after one week, one month, 3 months and one year; patients were examined and clinical symptoms were recorded. Long-term patient follow-up was at least 4 years. If patients were lost to follow-up, they were interviewed over the phone about the persistence of symptoms. If these persisted, patients were scheduled for office visits.
In order to assess the factors implicated in the recurrence of hemorrhoid symptoms, the patients were divided into 2 groups according to whether they were asymptomatic or had experienced recurrence. As potential influential factors, sex, age, hemorrhoid grade and operative time (as a measurement of technical difficulty) were compared.
The study was conducted in accordance with the guidelines of the Declaration of Helsinki; patient data remained confidential and the regulations of the local Ethics Committee were followed.
Statistical AnalysisThe statistical analysis was computed with the X2 test, Fisher's exact test when necessary, and the Mann–Whitney U test. A P<.05 was considered statistically significant.
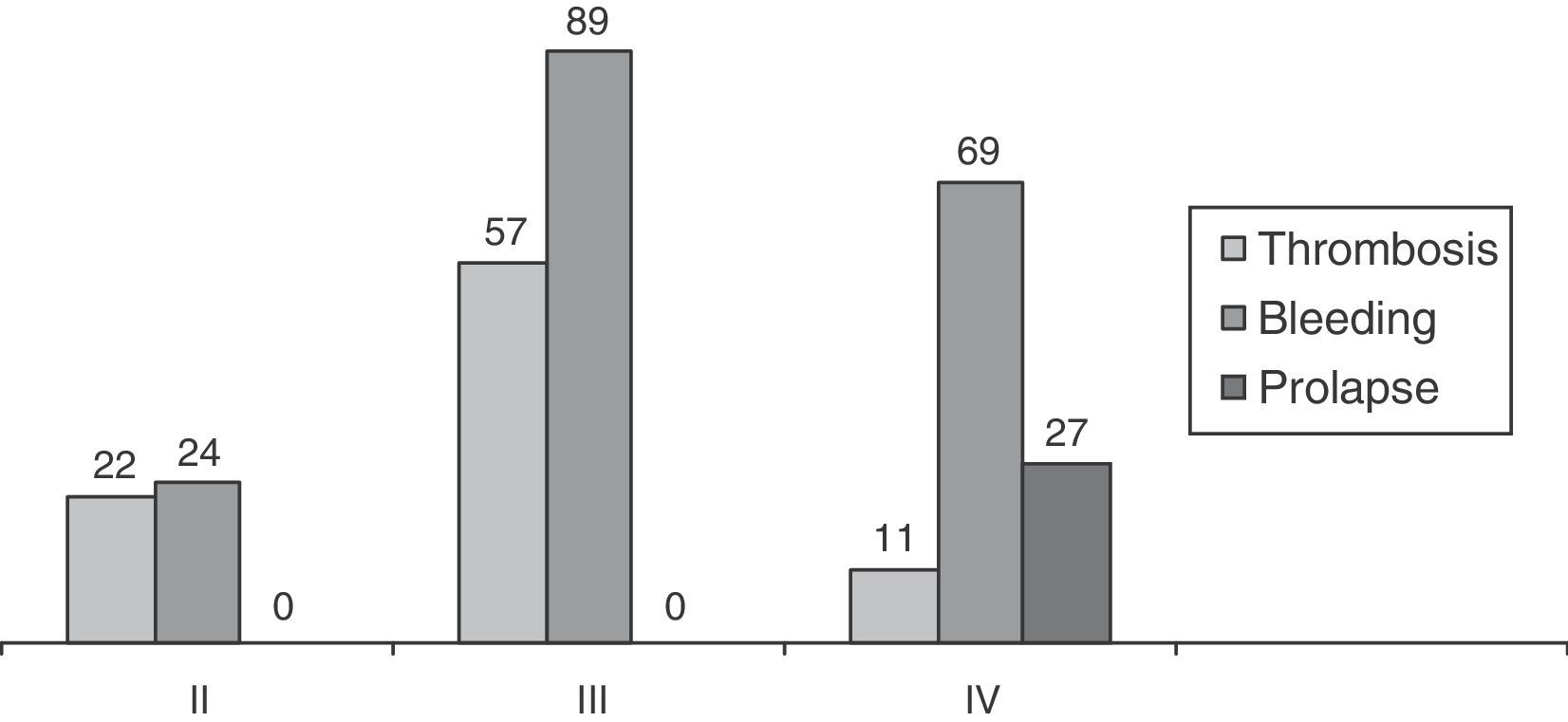
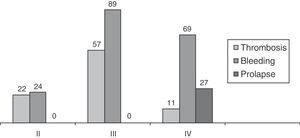
ResultsMean patient age was 48.5 (16–95). There was a predominance of men (196; 60%) over women (131; 40%): 29 patients with RMP, 48 patients with grade II hemorrhoids, 146 with grade III and 104 grade IV. The patients with grade II corresponded with treatment failure with elastic bands or sclerosis. SA was also proposed for patients with grade III and grade IV hemorrhoids with limited external fibrous component, or rather if they accepted its persistence after the intervention. Patients were always informed of the postoperative advantages of SA and its recurrence rate. Fig. 1 shows the predominating clinical signs according to hemorrhoid grade.
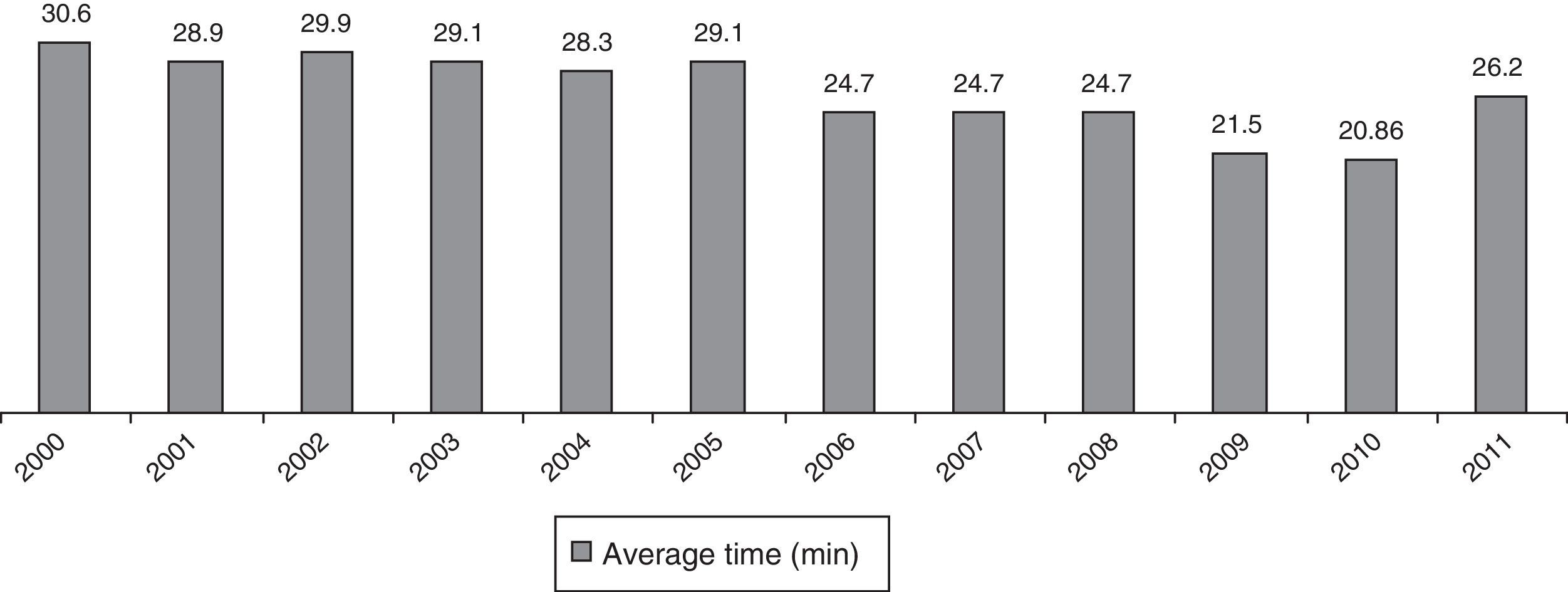
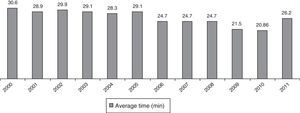
As for surgery, intradural anaesthesia was used in 301 cases (92%) and general anaesthesia was used in 26 (8%). Mean surgical time and its evolution are demonstrated in Fig. 2.
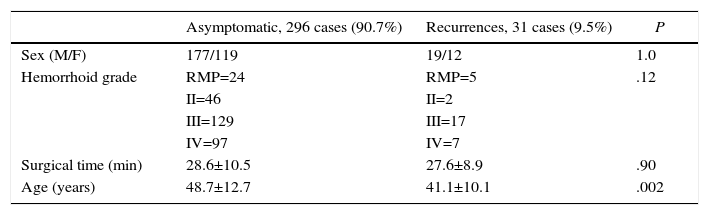
A total of 31 patients (9.5%) presented persistence of symptoms: 5 cases of RMP (recurrence 17.2%), 2 cases of grade II hemorrhoids (recurrence 4.2%), 17 cases of grade III hemorrhoids (recurrence 11.6%) and 7 cases of grade IV hemorrhoids (recurrence 6.7%). In 21 patients (67.8%), the predominant symptom that led to further treatment was prolapsed hemorrhoids or mucosa, while in 10 patients (32.2%) the cause was persistent rectal bleeding. Milligan–Morgan hemorrhoidectomy was performed in 21 patients (67.7%) and another SA was done in 3 patients (9.7%). We used elastic bands in 7 cases (22.6%), all of which were patients with persistent postoperative grade II hemorrhoids. Therefore, 24 patients (7.3%) required re-operation. As for surgical treatment, another SA was proposed in 2 cases of RMP and one case of hemorrhoids. Table 1 shows the results of the comparative study between the recurrence and asymptomatic groups. There were no significant differences between patients with or without recurrence in terms of sex, operative time or hemorrhoidal grade, but a difference was observed with regards to age.
Comparison of Asymptomatic Patients and Recurrence.
| Asymptomatic, 296 cases (90.7%) | Recurrences, 31 cases (9.5%) | P | |
|---|---|---|---|
| Sex (M/F) | 177/119 | 19/12 | 1.0 |
| Hemorrhoid grade | RMP=24 | RMP=5 | .12 |
| II=46 | II=2 | ||
| III=129 | III=17 | ||
| IV=97 | IV=7 | ||
| Surgical time (min) | 28.6±10.5 | 27.6±8.9 | .90 |
| Age (years) | 48.7±12.7 | 41.1±10.1 | .002 |
RMP: rectal mucosal prolapse.
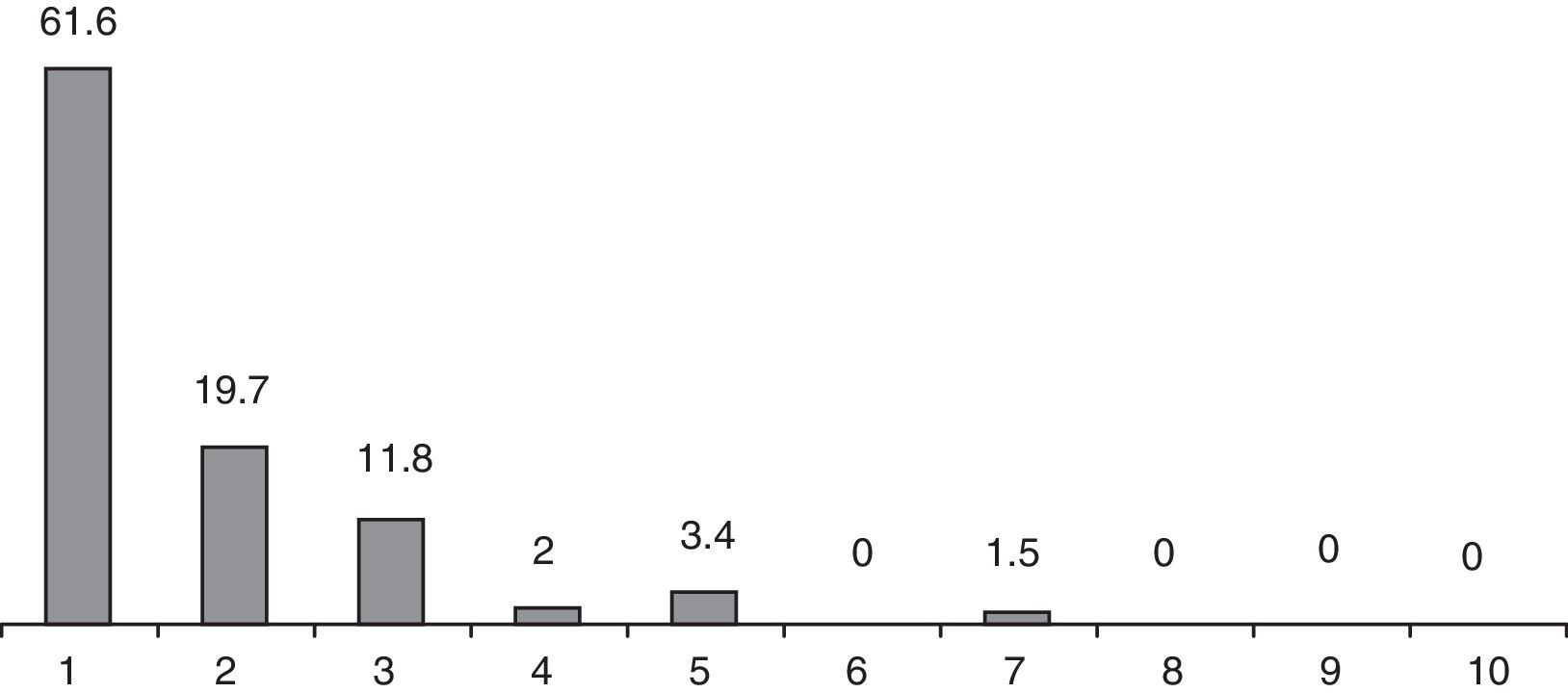
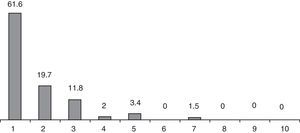
Postoperative pain levels recorded after one week are shown in Fig. 3. Most patients (81.3%) expressed a degree of pain below 2 according to a VAS and only in 2 patients did it reach 7. At the postoperative visit one month after surgery, none of the patients reported a need for analgesia for more than 10 days.
Five patients (1.6%) required reoperation due to bleeding during the immediate postoperative period (initial 24h), 3 of which were within the first 30 patients. One patient (0.3%) presented symptoms of abdominal pain and hypotension as a consequence of a pelvirectal haematoma, which was resolved with conservative therapy. Four patients (1.2%) required hospitalisation because of their pain: 3 from the MAS unit and the remaining patient just a few hours after having been discharged. In addition, there were also 7 patients (2.1%) who experienced acute urinary retention.
Defaecation urgency and tenesmus were almost constant in all patients, although this did not last more than 2 weeks post-op. Mild incontinence (gas or liquid faeces) was present in 26 patients (7.9%), but it was self-limiting and resolved within 3 months, except in one case (previous internal lateral sphincterotomy due to anal fissure that responded well to sphincter training).
In 323 cases (98.7%), the postoperative histology study of the rectal tissue resected in SA showed the presence of smooth muscle cells. Only in 4 cases was there no muscle tissue.
DiscussionSA is not a hemorrhoidectomy; instead, it is a hemorrhoidopexy.14 At the start of the technique, what became popular in the English-speaking literature was the concept of “stapled hemorroidectomy”,15–22 which is a mistaken perception. The resection and stapling of the mucosa and submucosa should achieve a “pexy” or fixation of the hemorrhoidal tissue, far from the area of the hemorrhoid insertion (dentate line) and the pain receptors of the anoderm.21,22
SA is a functional treatment used to resolve the symptoms of hemorrhoid disease. The prolapsed mucosal and submucosal layers are resected, as in rectal intussusception, and the edges are later stapled to affix the tissue. The concept defended by Longo that the arterial flow is interrupted by a mechanism of action of SA5 is probably less exact, which has been confirmed by some studies.23
The SA surgical technique is not complex, but it should be systematic.13,24,25 The NICE study defined the learning curve of this technique to be 10–12 procedures.7 In our opinion, this number is low and we believe that some 30 cases are necessary, as argued by Jorgen et al. and Slawik et al.26,27 The progressive reduction observed in surgical times reflects this learning curve.
We have always allowed patients to choose the technique to be performed, after having been properly informed. An overall recurrence rate of 9.3% is acceptable and similar to that of most groups who utilise SA, although the results in the literature are disparate.13,16,18,28–31 The indications for SA are limited to cases with failed conservative treatment in grade II hemorrhoids (sclerosis, infrared or elastic bands) and in grade III hemorrhoids.32 Its use in grade IV is more controversial. In cases of RMP, we obtained deficient results, probably due to insufficient tissue resection. There are authors who also suggest the option of double stapling in the initial intervention.33–36
The recurrence rate in grade IV hemorrhoids was 6.7%, but in selected patients.37 Patients who are offered treatment with SA should understand that it is a functional treatment. Furthermore, the fibrous perianal formations present in patients with grade III and IV hemorrhoids are rarely reduced with SA, and the patient should be made aware of this fact before surgery.38–41 The aim of the intervention is to control the predominant symptom (for example, bleeding).42
In the comparative study between the group with success and the group with recurrence after SA, only patient age seemed to provide significant differences. This may be due to the RMP rate in the recurrence group, with a predominance of younger patients. We have found no differences for sex, hemorrhoid grade or surgical time (as a measurement of technical difficulty). Festen et al.43 show a lower prolapse recurrence rate in patients treated with previous banding, in patients with the presence of muscle fibres in the tissue doughnuts, and in those operated on by surgeons who have experience in the management of the PPH stapler. We had a high percentage of muscle fibres in the postoperative histopathology study of the resected tissue (98.7%), which is similar to the report by Maw et al.44
SA causes significantly less postoperative pain than resection techniques.12,14,15,17,45 Our results along these lines are similar to those of other studies.11,21,22,32 Pain after hemorrhoidal resection is important, even in spite of using analgaesic techniques.46 Some groups perform resection techniques in major ambulatory surgery units,47,48 but the level of postoperative pain in these patients seems excessively high in our opinion, even when cases are selected according to risk factors.49 We only do this when treating hemorrhoid groups.
Persistent pain after SA is due to resection and stapling excessively close to the dentate line.5 At the start, we performed the technique 5 or 6cm from the dentate line to minimise postoperative pain. We later lowered this limit to a distance of at least 2cm.13 Pain is most likely not related with muscle fibres being included in the stapling50 since, in our experience and that of other reports, the percentage of cases with resected mucosa-submucosa including muscle fibres is higher than 90%,44,51 without this fact affecting pain levels. In our series, only 2 patients complained of pain higher than 7; however, we did have to hospitalise 4 patients (1.2%) treated in MOS due to uncontrolled pain.
The earliest complication after SA is postoperative bleeding of the staple line in the first 24h, which can require immediate reoperation.52,53 It is a serious complication that needs to be re-explored under anaesthesia. We have had 5 cases (1.5%) in which we achieved haemostasis of the bleeding vein with absorbable sutures, with no later complications. Three of these situations occurred within the first 30 cases treated, during the learning curve. As our tendency is to conduct these interventions in the MAS setting, we pay special attention to intraoperative haemostasis.
The most serious complication of SA is pelvic sepsis. Since the first description by Molloy and Kingsmore in 2000,54 29 articles have reported 40 patients, with a total of 4 deaths. They all may possibly be due to complete transection of the rectal wall, which would also be the cause of other recently published complications.55–57 We have not had cases of pelvic sepsis, although there was one unusual complication: a perirectal haematoma with hypovolemic shock, which was successfully treated conservatively.58 In women, it is important to check that the posterior vaginal wall is not included in the staple line in order to avoid rectovaginal fistulas.59 The histopathologic study of the resected rectal tissue segment can warn us, as there is probably quite a difference between identifying isolated muscle fibres and finding areas of the entire rectal wall.
Complications related with the mechanics of defaecation, such as urgency and rectal tenesmus, were constant but mild. Incontinence (7.9%) reached an important rate, but we observed that it disappeared over time. As for acute urinary retention, which affected 7 patients, we believe that this may be more related with the intradural anaesthesia than the surgery itself.60–62
New techniques are appearing, such as Doppler-guided transanal hemorrhoidal dearterialisation, which has provided promising results.63,64 The effective basis of the technique also makes reference to the hypothesis by Thompson.6 It is clear that the immediate postoperative period is less painful than when resection techniques are used, rather similar to SA.65 Nonetheless, postoperative follow-up times are still too short to determine its actual efficacy66–68 and studies are needed with more patients, high-grade hemorrhoids and longer follow-up times.66
In conclusion, the study we present shows that SA is a useful technique for the treatment of hemorrhoidal disease in select cases. It can be conducted in the MAS unit due to the low levels of postoperative pain, although the recurrence rate is higher than resection techniques. There is no ideal surgical treatment available for hemorrhoids, but SA does play a part. Its success is based on proper patient selection and providing appropriate information about the results expected, together with the surgical team's proven experience in this technique.
Conflict of InterestThe authors have no conflict of interests to declare.
Please cite this article as: Hidalgo Grau LA, Ruiz Edo N, Llorca Cardeñosa S, Heredia Budó A, Estrada Ferrer Ó, del Bas Rubia M, et al. Anopexia mucosa grapada: experiencia y consideraciones sobre la técnica. Cir Esp. 2016;94:287–293.