Almost 40% of women who undergo breast surgery are dissatisfied with the decision-making process as well as cosmetic results. Our objective was to demonstrate the usefulness of the BREAST-Q™ preoperative questionnaire to evaluate the satisfaction and health-related quality of life in women with diagnosis of breast cancer prior to surgery, as well as identifying satisfaction profiles.
MethodsProspective cohort observational study in women with breast cancer, evaluating preoperative quality of life using the BREAST-Q™ questionnaire. Percentile measures for each domain and baseline physical characteristics were assessed for posterior analysis.
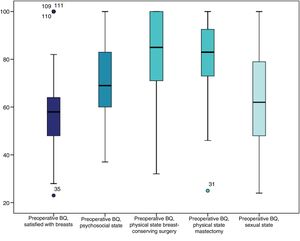
ResultsThe average score in the breast satisfaction domain was 58.9±16.9. The average score in the preoperative psychosocial well-being domain was 70.5±16.1. Patients who were offered conservative surgery had a mean physical well-being score of 80.7±18.5, and those who were offered mastectomy had an average score of 79.9±17.7. The sexual well-being average score was 63.2±20.7. No statistically significant differences were found between low-score and high-score groups regarding epidemiological and clinical characteristics.
ConclusionsPreoperative evaluation in breast cancer patients provides correct assessment of the effect of surgical treatment on patient satisfaction and quality of life. This information is useful for communicating with patients about their expectations and postoperative results.
Cerca del 40% de las mujeres intervenidas por un carcinoma mamario refieren estar insatisfechas con la toma de decisiones y con el resultado cosmético de la cirugía. El objetivo del estudio es demostrar la utilidad del cuestionario prequirúrgico BREAST-Q™ para evaluar la satisfacción y calidad de vida de las mujeres con cáncer de mama en un estado basal previo a la cirugía e identificar perfiles de satisfacción.
MétodosEstudio observacional de una corte prospectiva en mujeres con carcinoma de mama donde se evaluó la calidad de vida antes y después de la intervención propuesta mediante el cuestionario prequirúrgico BREAST-Q™. Se presentan los resultados preliminares del estudio, con el análisis de la fase prequirúrgica. Se calcularon los percentiles para cada dominio del cuestionario y se evaluaron las características físicas basales para su posterior análisis.
ResultadosLa satisfacción media de las pacientes con sus mamas fue de 58,9±16,9. La media de bienestar psicosocial prequirúrgico fue de 70,5±16,1. A las pacientes que se les propuso una cirugía conservadora presentaron una media de bienestar físico de 80,7±18,5 y a las pacientes que se les propuso una mastectomía con reconstrucción fue de 79,9±17,7. La media de score para el bienestar sexual fue de 63,2±20,7. No se encontraron diferencias estadísticamente significativas entre el grupo de mujeres con score bajo y el grupo con score medio o alto en cuanto a las características clinicoepidemiológicas de las pacientes.
ConclusionesLa evaluación preoperatoria de las pacientes con cáncer de mama permite una correcta valoración del impacto de la cirugía sobre la satisfacción y calidad de vida, siendo de utilidad para orientar el proceso informativo acerca de las expectativas de los resultados postoperatorios.
Until now, the assessment of breast cancer treatment results has been based on biomedical measures and parameters, including morbidity and mortality, overall and disease-free survival, tumor response and recurrence. However, in recent years, interest has increased in the impact the disease and its treatment have on the quality of life of women suffering from breast cancer.1
In recent decades, there have been reports that about 40% of women treated surgically for breast carcinoma report being unsatisfied with the decision-making process and the cosmetic results of surgery.2,3 Klassen et al. concluded that breast surgery can affect women in multiple spheres, potentially altering their quality of life and satisfaction.4
Several studies have been published5–9 that evaluate the quality of life in women treated surgically for breast cancer, using various questionnaires and different surgical approaches. The BREAST-Q™ questionnaire was developed at the Memorial Sloan-Kettering Center and Columbia University in the United States to provide a patient-reported outcome (PRO) tool with a high degree of validity, reliability and sensitivity for measuring the perception and experience of patients with different types of breast surgery. In addition, its use in Spain has been available since its linguistic validation in 2016. This questionnaire creates a conceptual structure comprised of 6 main themes or domains: psychosocial, sexual and physical well-being; and satisfaction with the breasts, the final results of surgery and the medical care process.4 However, most publications make a single assessment when the patient has already undergone surgery, and no consideration is given to baseline status before surgery. This prevents us from having useful information both for daily clinical practice and for understanding changes in patient satisfaction during the treatment process.
The main objective of the BREAST-Q™ questionnaires is to compare quality of life scores before and after surgery. The objective of this study, however, is to show the importance of the pre-operative BREAST-Q™ module administered in women at a baseline state prior to surgery. This would determine the satisfaction and quality of life of these patients and identify satisfaction profiles, which would allow surgeons to decide which procedure is best for each patient.
MethodsWe present an observational study of a prospective cohort between February 2014 and February 2019. We included in the study all women over the age of 18 with a diagnosis of invasive ductal or in situ carcinoma of the breast treated in the Breast Unit of our hospital in order to evaluate their quality of life both before the proposed procedure and after treatment for comparison. The sample size was calculated for the pre- and postoperative comparative study, defined as a minimum of 57 patients, which would allow for significant statistical differences to be detected with a power of 80%. This first article shows the preliminary results of the study from the preoperative analysis of the data. Male patients, patients with benign disease, and women who chose not to participate in the study were excluded. The patients were invited to participate in the study during their first office visit with the breast surgeon.
BREAST-Q™ questionnaires are comprised of two modules: preoperative and postoperative. In this study, only the preoperative BREAST-Q™ questionnaires for breast-conserving surgery and mastectomy were analyzed, depending on the procedure proposed. The questionnaires were completed at home in paper format and given to researchers prior to the surgical procedure.
According to the guidelines for use of the BREAST-Q™,10 the results of each domain of the questionnaire were converted to a score of 0–100, indicating the percentage of satisfaction. Because some items in the physical well-being domain are different in the mastectomy and breast-conserving surgery questionnaires, we decided to carry out the analysis individually for this domain.
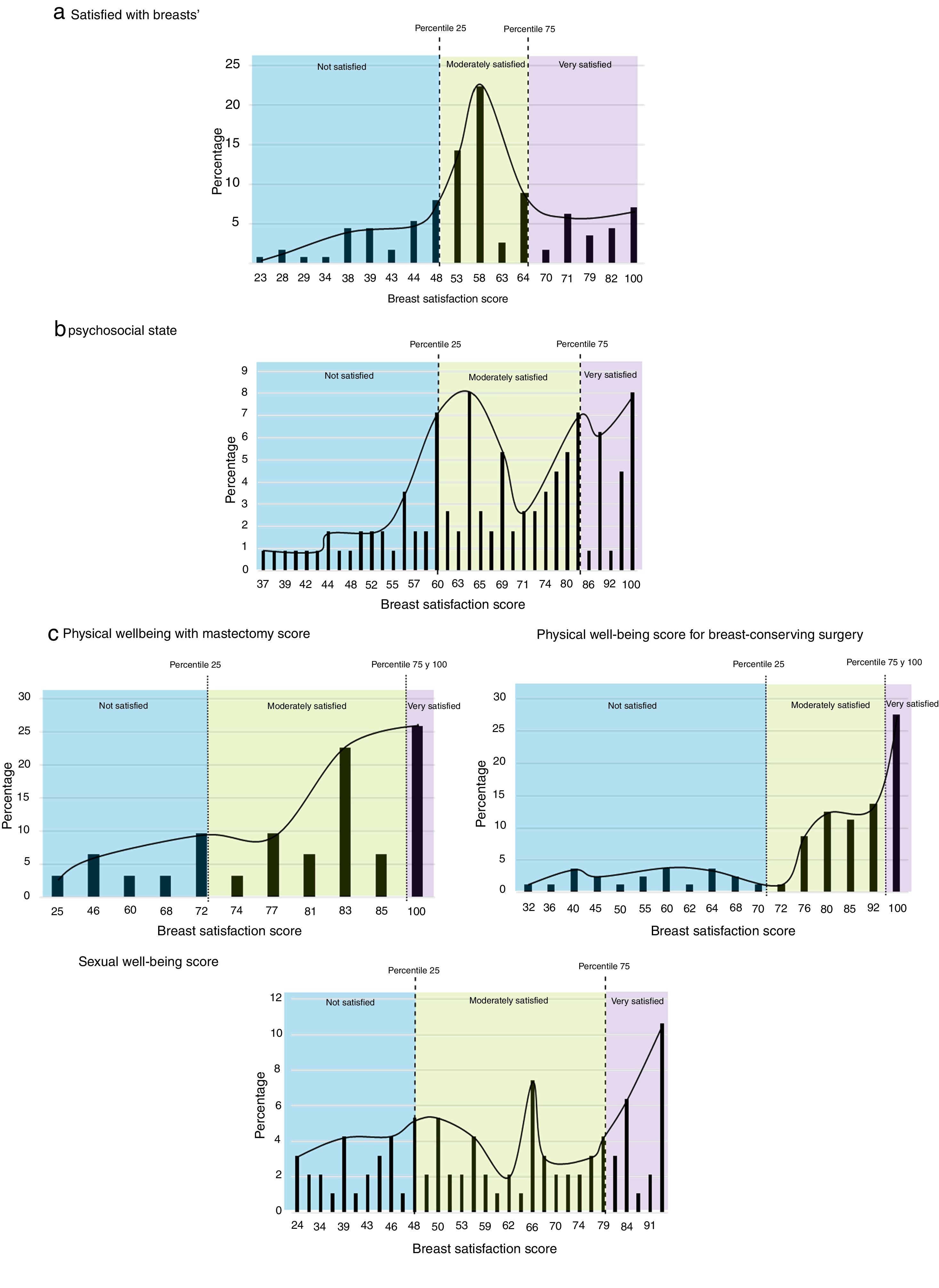
The quantitative variables were expressed with mean±standard deviation, and the qualitative variables with numbers and percentages. The percentiles for each domain of the questionnaire were calculated, and a qualitative analysis of the scores was performed based on these percentiles, defining 3 groups in each domain. Scores below the 25th percentile were called ‘low satisfaction’; scores between the 25th and 75th percentiles ‘moderate satisfaction’, and scores greater than the 75th percentile ‘high satisfaction’.
These groups were compared in terms of their baseline physical characteristics (weight, height, body mass index [BMI], distance between clavicle and nipple-areola complex [NAC], menstrual status and age). The association between qualitative variables was analyzed with the chi-squared or Fisher's exact test. After verifying the normality of the quantitative variables, the Student's t-test, ANOVA for independent groups, the Mann–Whitney U or Kruskal–Wallis tests were used as needed. Data were retrieved and analyzed using the SPSS program (SPSS v22; SPSS, Inc., Chicago, USA).
This study was approved by the research ethics committee of our hospital with registration code number 2016/028.
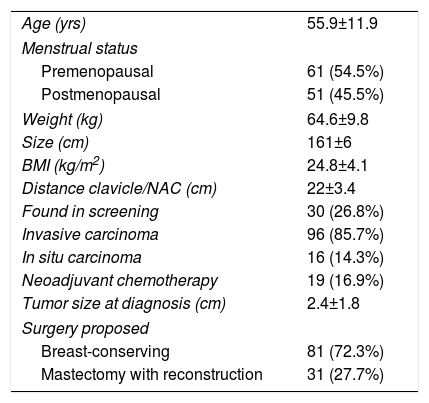
ResultsPatient CharacteristicsDuring the study period, 752 breast surgeries were performed, and 112 patients met the inclusion criteria. At the time of consultation, breast-conserving surgery was proposed for most patients (81 patients; 72.3%) included in the study, and mastectomy with immediate reconstruction was proposed for the remaining 27.7%. Mean patient age was 52.9±11.9 years (range: 28–84 years), and 54.46% were premenopausal.
Table 1 summarizes the main clinical characteristics of the study patients. Most women (85.7%) had invasive breast cancer, and the remaining 14.3% had in situ carcinoma. Mean weight and height were 64.6±9.8kg and 161±6cm, respectively, with a mean BMI of 24.8±4.1kg/m2. The average clavicle/NAC distance was 22±3.4cm, ranging from 15 to 30cm.
Clinical Characteristics of Patients.
| Age (yrs) | 55.9±11.9 |
| Menstrual status | |
| Premenopausal | 61 (54.5%) |
| Postmenopausal | 51 (45.5%) |
| Weight (kg) | 64.6±9.8 |
| Size (cm) | 161±6 |
| BMI (kg/m2) | 24.8±4.1 |
| Distance clavicle/NAC (cm) | 22±3.4 |
| Found in screening | 30 (26.8%) |
| Invasive carcinoma | 96 (85.7%) |
| In situ carcinoma | 16 (14.3%) |
| Neoadjuvant chemotherapy | 19 (16.9%) |
| Tumor size at diagnosis (cm) | 2.4±1.8 |
| Surgery proposed | |
| Breast-conserving | 81 (72.3%) |
| Mastectomy with reconstruction | 31 (27.7%) |
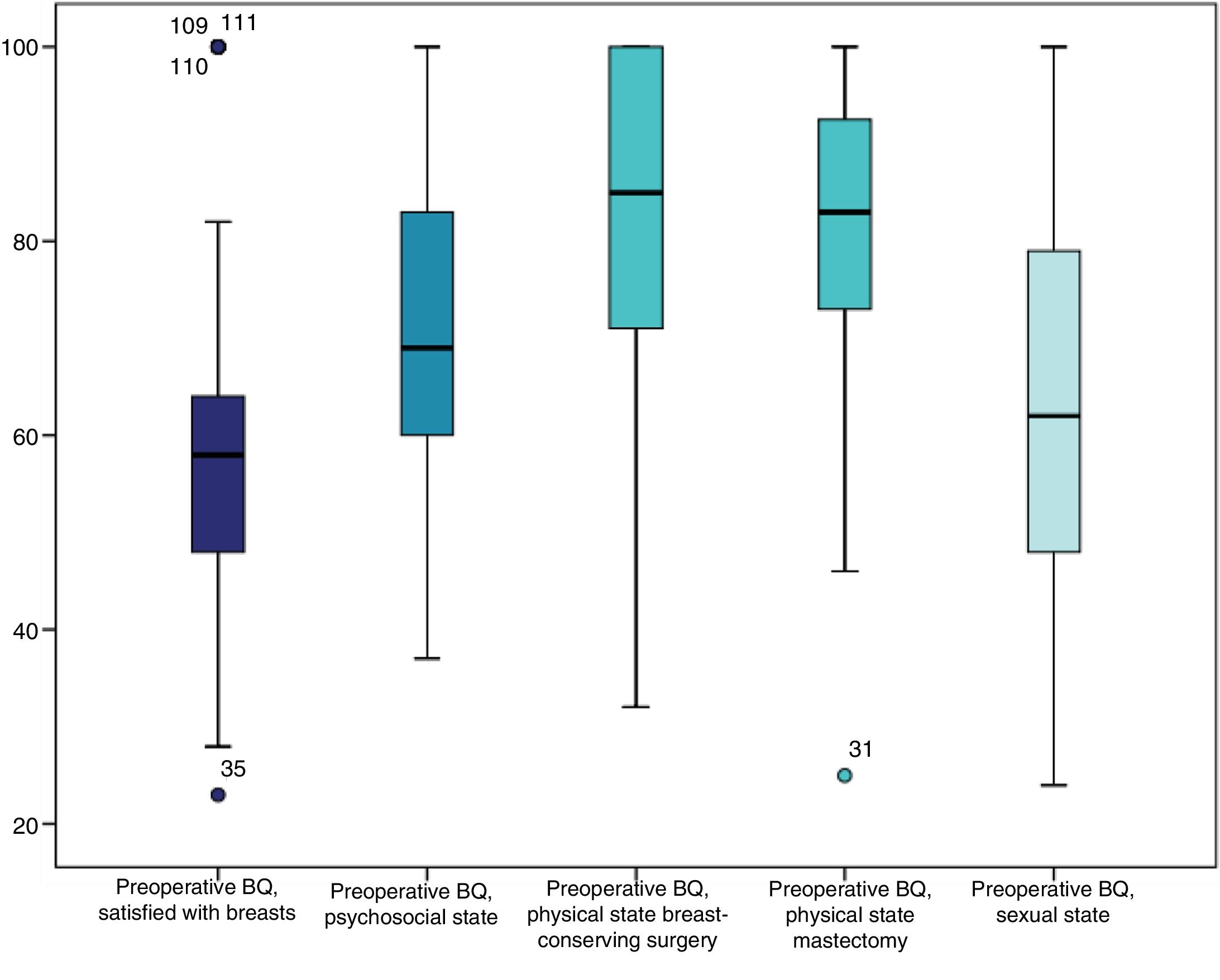
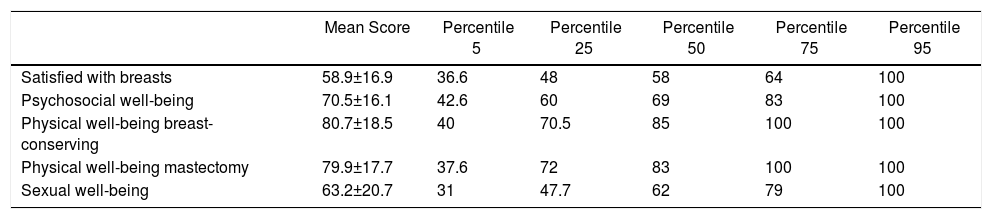
The results of the scores of all the domains present a heterogeneous distribution, even with some extreme values in the domains of ‘satisfied with breasts’ and ‘physical well-being’ (Fig. 1). Table 2 shows the means and percentiles for the scores of all the domains evaluated. Lower values were found in the domain ‘satisfied with breasts’ compared to the ‘physical well-being’ domain.
- –
Satisfied with breasts. The mean satisfaction of the patients with their breasts was 58.9±16.9 (Table 2). The individual analysis of the questions in this domain determined that most women were satisfied or very satisfied with their appearance in front of the mirror, dressed or undressed, as well as with their bra and tight clothing (Fig. 2a). As seen in Fig. 2a, in this domain the interval between the 25th and 75th percentiles is narrow, meaning that the majority of patients (56.2%) have a score between 48 and 64.
- –
Psychosocial well-being. The mean preoperative psychosocial well-being of the patients was 70.5±16.1 (Table 2) (Fig. 2b). Heterogeneous distribution was observed in the responses of this domain. Most of the patients responded that they always or almost always have adequate psychosocial well-being; 63.4% always feel as valued as other women, and 48.8% feel emotionally healthy. In contrast, 14.6% of the patients answered that they never feel attractive (7.3%) or rarely (7.3%).
- –
Physical well-being. The physical well-being questionnaire is different for mastectomy and breast-conserving surgery, so the analysis was performed individually. The patients who were proposed breast-conserving surgery had a mean physical well-being of 80.7±18.5, while in patients scheduled for mastectomy with reconstruction it was 79.9±17.7 (Table two). 25.8% of the group of patients with a mastectomy and 27.5% of the patients with conservative surgery had high satisfaction (Fig. 2c and d, respectively). Most patients report little or no related discomfort or pain in the breast or the arm (item evaluated in the preoperative questionnaire). It should be noted that 33.3% of women sometimes reported sharp breast pain, although this data could be related with the puncture-biopsy performed in all patients during the diagnostic process. In addition, 31 and 29.6% of women sometimes reported pain in the upper back and arm, respectively.
- –
Sexual well-being. 83.9% of the patients completed the sexual well-being questionnaire. The mean score for sexual well-being was 63.2±20.7, showing a heterogeneous distribution in the responses (Table 2) (Fig. 2e). Most of the patients answered ‘almost always’ to all questions about sexuality, noting that 28.2% and 23.5% of the patients answered that they ‘sometimes’ feel sexually attractive when dressed or undressed, respectively.
Means and percentiles of the domains evaluated.
| Mean Score | Percentile 5 | Percentile 25 | Percentile 50 | Percentile 75 | Percentile 95 | |
|---|---|---|---|---|---|---|
| Satisfied with breasts | 58.9±16.9 | 36.6 | 48 | 58 | 64 | 100 |
| Psychosocial well-being | 70.5±16.1 | 42.6 | 60 | 69 | 83 | 100 |
| Physical well-being breast-conserving | 80.7±18.5 | 40 | 70.5 | 85 | 100 | 100 |
| Physical well-being mastectomy | 79.9±17.7 | 37.6 | 72 | 83 | 100 | 100 |
| Sexual well-being | 63.2±20.7 | 31 | 47.7 | 62 | 79 | 100 |
No statistically significant differences were found between the group of women with a low score and the group with a moderate or high score in terms of the clinical–epidemiological characteristics of patients (age, weight, height, BMI, clavicle/NAC distance), so it was possible to determine a physical-clinical profile of women with low or high satisfaction.
DiscussionSatisfaction and quality of life have become very important in evaluating the treatment results of patients with breast cancer. Several multidimensional global assessment tools have been developed to evaluate aspects of physical, communicational, cognitive and psychosocial function.11 In breast cancer treatment, women should participate in the therapeutic decision (based on satisfaction results and real information from patients who have already experienced the same condition) and choose the treatment option that best suits their situation.12
The first health-related quality of life (HRQoL) measurement tools focused mainly on the assessment of the basic and instrumental activities that patients could perform. Today, the evaluation aims to be much broader and takes into account physical, functional and psychosocial results. Information is obtained through structured questionnaires that combine a number of items or closed questions to evaluate each of the dimensions or domains. Subsequently, the responses to each item can be grouped into a single global score.13 These instruments or questionnaires that collect the state of health-related conditions directly from the patient, without interpretation by medical staff, are known as patient-reported outcomes (PRO).14
BREAST-Q™ questionnaires have been shown to be useful in evaluating satisfaction and HRQoL in patients undergoing surgery for breast cancer.10 Several studies15–21 have been published that evaluate the quality of life of women operated on with conservative surgery using the BREAST-Q™ questionnaire. However, all of them are retrospective studies that only evaluate postoperative data, and none of them include baseline data for satisfaction and quality of life prior to surgery. Until today, only Mundy et al.22 in 2017 used the preoperative BREAST-Q™ questionnaire to obtain the baseline results of women with breast carcinoma and then compared them with postoperative results from previous publications, to be used as a clinical reference point for the interpretation of the data.
Although the main objective of BREAST-Q™ questionnaires is to compare pre- and postoperative quality of life, our study provides highly relevant information on the baseline status of patients with breast cancer prior to therapeutic procedures. This allows us to determine their starting point before planning surgery, while objectively predicting the possible improvement in satisfaction at the end of treatment. Another objective of our study was to define patient profiles in order to guide surgeons in choosing the type of procedures. However, we have found no relevant clinical-pathological characteristics to identify these profiles. In addition, we find it necessary that each medical center or region must obtain its own population data for preoperative evaluation since, as our study shows, there are no anthropometric or clinical variables related to previous satisfaction, which may indicate that local cultural or social factors affect this preoperative evaluation.
The results of our series are variable and express an intermediate level of satisfaction and well-being. The highest values are seen in the physical well-being domain, which may be explained by most patients being diagnosed in initial stages when the disease still has not had physical repercussions. It is important to bear in mind that high satisfaction rates are more difficult to maintain after surgical treatment, chemotherapy and radiotherapy, and it is in these domains where the impact of the therapies established is more clearly observed.
It is important to highlight that the women evaluated with the questionnaire were already aware of their diagnosis of breast cancer. This may have had an influence, especially on psychosocial well-being, although in our series the average satisfaction in this domain was also high. Conducting this evaluation with women who are aware of their diagnosis may be more objective since the negative effect of the diagnosis has already been previously assessed, and surgical therapy is the only variable.
Several studies have shown sexual dysfunction in up to 90% of patients with breast cancer, and breast surgery is a negative factor.23–25 Lagendijk et al.21 conclude that the evaluation of postoperative sexual well-being has little clinical applicability due to the low response rate of the items and the lack of longitudinal analysis. The baseline data in this domain can help to partially improve the subsequent analysis, since we can learn about possible sexual dysfunctions that would change little with breast surgery or, conversely, detect new alterations in sexual function that appear after surgical intervention.
One of the limitations of this study is that it could not identify a patient profile related to satisfaction and quality of life prior to surgery. This is perhaps because other social or environmental factors that directly affect these variables have not been taken into account, such as marital status, employment status, etc. It is possible that future studies may resolve this limitation with the use of generic questionnaires (such as the SF36 or EORTC C30), which provide additional information about these external factors.
In our opinion, the creation of satisfaction percentiles more objectively defines high, moderate and low levels of satisfaction for each domain and allows us to know the starting point of each patient prior to the procedure in order to subsequently assess the impact of surgery. Thus, with this information, we can preoperatively identify women with high satisfaction with their breasts in whom surgery can only worsen that satisfaction, and, conversely, women with low satisfaction with their breasts in whom surgery will not significantly affect their opinion.
In conclusion, our study does not identify variables related to satisfaction and quality of life in women with breast cancer before their surgical procedure. However, this preoperative assessment is useful for guiding the informative process of postoperative results, especially in those patients with high satisfaction levels prior to surgery. Finally, we consider that the preoperative evaluation of patients with breast cancer provides a correct assessment of baseline quality of life in this group of patients and can help in decision-making and in data processing prior to surgery.
It also opens a possible line of research where our results can be used for comparison with other patient groups, be they healthy women, where the role of breast cancer diagnosis is evaluated in terms of satisfaction and quality of life, or in postoperative patients, where the results were evaluated but there is no previous measurement with which to compare.
Please cite this article as: Builes Ramírez S, Acea Nebril B, García Novoa A, Cereijo C, Bouzón A, Mosquera Oses J. Evaluación de la percepción preoperatoria de la calidad de vida y satisfacción de la mujer con cáncer de mama mediante el cuestionario BREAST-Q™. Cir Esp. 2020;98:212–218.