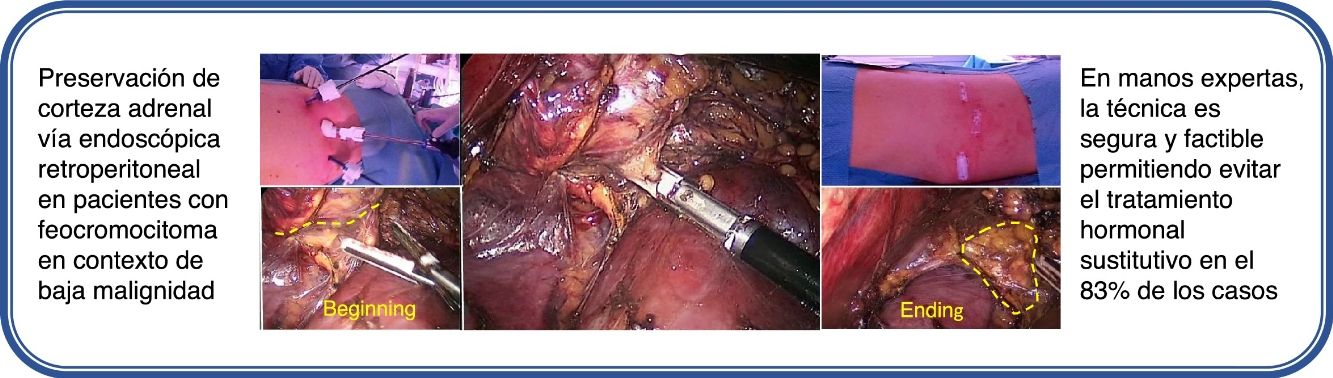
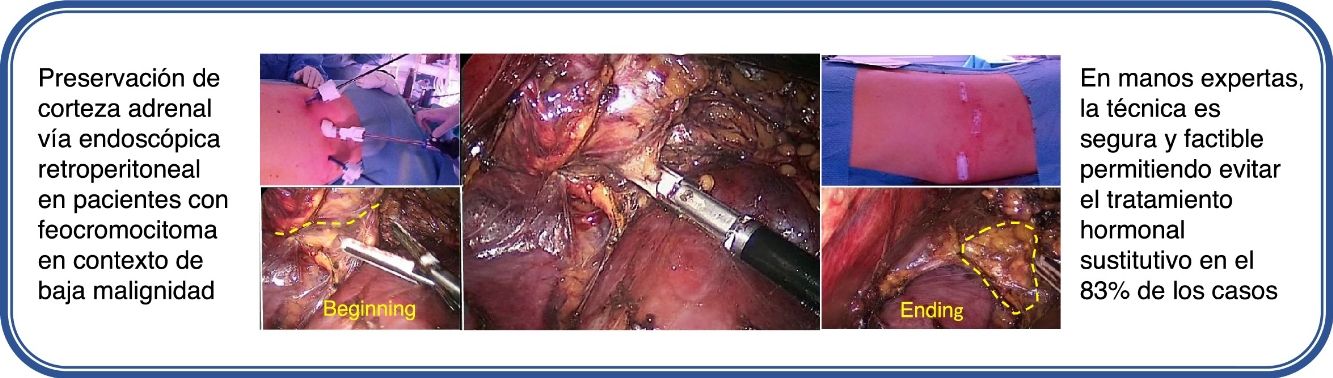
Cortical-sparing adrenalectomy is a suitable treatment for hereditary and sporadic bilateral pheochromocytoma, in cases of low risk of malignancy, to reduce the possibility of adrenal insufficiency assuming the chance of local recurrence. The aim of the study is to analyze the functional results of partial adrenalectomy by retroperitoneal endoscopic approach in single-adrenal patients or patients requiring bilateral adrenalectomy.
MethodsProspective study between January 2015 and February 2016 including pheochromocytoma patients diagnosed with low risk of malignant mutations. All patients agreed to be included in the study. Experienced endocrine surgeons who have been trained in minimally invasive endocrine surgery performed the procedure using the same surgical technique. Demographic variables and clinical characteristics were collected, subsequently carrying out the descriptive analysis of the data.
ResultsA total of 6 patients were registered, four associated with MEN type 2 syndrome and two in the context of VHL syndrome. Retroperitoneoscopic resection was performed without laparoscopic or open conversion and no postoperative complications; the average hospital stay was 2.5 days. Preservation of the functional cortex without corticosteroids was achieved in 5 (83%) of out 6 cases with a follow-up of 26.2±6 months. Today, these 5 patients have a preserved adrenal function without hormone replacement.
ConclusionsCortical-sparing adrenalectomy by the retroperitoneal endoscopic approach, in expert hands, is safe and feasible for the treatment of hereditary and sporadic pheochromocytoma in a context of low malignancy, making it possible to avoid the need for corticoid replacement in most cases.
La adrenalectomía con preservación cortical se indica como tratamiento del feocromocitoma bilateral hereditario y esporádico, en casos de bajo riesgo de malignidad, para reducir la posibilidad de insuficiencia suprarrenal asumiendo la eventualidad de una recidiva local. El objetivo del estudio es analizar los resultados funcionales de la adrenalectomía parcial por vía endoscópica retroperitoneal en pacientes monoadrenales o que necesiten una adrenalectomía bilateral.
MétodosEntre enero de 2015 y febrero de 2016 se incluyeron de forma prospectiva pacientes con feocromocitoma asociado a mutaciones con bajo riesgo para malignidad, que aceptaron participar en el estudio. Todos fueron operados por cirujanos especialmente entrenados en este tipo de cirugía, utilizando la misma técnica quirúrgica. Se recogieron variables demográficas y características clínicas, realizando posteriormente el análisis descriptivo de dichas variables.
ResultadosSe registraron un total de 6 pacientes, cuatro asociados al síndrome MEN tipo 2 y dos en contexto del síndrome VHL. No fue precisa ninguna conversión a abordaje laparoscópico o abierto y tampoco complicaciones postoperatorias, la estancia hospitalaria media fue de 2,5 días. Se logró la preservación de corteza adrenal funcionante sin requerimiento corticoideo en 5 (83%) de 6 casos. Con un seguimiento medio de 26,2 ± 6 meses, estos 5 pacientes presentan una función adrenal conservada sin aporte hormonal sustitutivo.
ConclusionesLa adrenalectomía con preservación cortical por vía endoscópica retroperitoneal, en manos expertas, es segura y factible para el tratamiento del feocromocitoma hereditario y esporádico en contexto de baja malignidad, permitiendo evitar la necesidad de aporte corticoideo en la mayoría de los casos.
Pheochromocytomas are rare neuroendocrine tumors originating from the chromaffin cells in the adrenal gland medulla.1 These tumors appear bilaterally in patients with genetic alterations, most associated with syndromes such as neurofibromatosis type 1 (NF-1) or von Recklinghausen disease, multiple endocrine neoplasia type 2 (MEN2), Von Hippel-Lindau disease (VHL) or hereditary paraganglioma-pheochromocytoma syndrome with high-penetrance mutations for developing benign adrenal lesions.2 50% of patients with MEN2 and 20% with VHL develop bilateral pheochromocytoma before the fifth decade of life, and the majority of these patients require complete adrenalectomy of both glands, either metachronous or synchronous.3 For patients who develop bilateral disease, complete removal of both adrenal glands leads to life-long adrenal insufficiency, with an increased risk of death due to Addisonian crisis, even in patients with adequate hormone replacement therapy.4 In this context, the idea has arisen to conduct partial excision of the gland in order to preserve correct adrenal function.
Cortical-sparing adrenalectomy is based on the identification of tumors with low risk for malignancy, assuming a reasonable risk of tumor recurrence that can be easily diagnosed and treated during conventional follow-up5; as a result, correct patient selection is especially relevant. Although the highest percentage of bilateral pheochromocytomas occur mainly in the context of MEN type 2 or VHL, whose profile is usually benign, pheochromocytomas in patients with mutations in genes encoding SDHB (succinate dehydrogenase subunit B) or MAX (viral myeloid proto-oncogene associated with factor X) have a higher risk of malignancy6 and should be excluded. Furthermore, it is important to note that the risk of recurrence is much higher in hereditary bilateral pheochromocytoma than in sporadic pheochromocytoma, since it is diffuse in the adrenal medulla. The aim of this study was to evaluate whether the retroperitoneal approach is able to preserve the functioning adrenal cortex in a safe and reproducible way in patients at low risk for malignancy with indication for bilateral adrenalectomy (metachronous or synchronous) and to evaluate its advantages based on our results.
MethodsA prospective study was designed to include patients with pheochromocytoma who had been operated on between January 2015 and February 2016 at our hospital. The study was approved by the ethics and clinical research committee of our hospital. All patients were included after having given specific consent for the preservation of adrenal tissue. Eligible patients had to present at least one-third of healthy adrenal gland tissue on magnetic resonance imaging studies that could remain in situ. The diagnosis of pheochromocytoma had to be associated with mutations with low risk for malignancy, based on clinical/family history and genetic study.6–8 In no case should signs of malignancy be detected during the preoperative study. Patients who did not meet these criteria or were not suitable to undergo the intervention were excluded from the study. Following the protocol at our hospital and current international guidelines,7–9 the diagnosis of pheochromocytoma was based on specific hormonal and biochemical tests, increased plasma metanephrine and normetanephrine levels in MEN2 and normetanephrine levels in VHL, and on imaging studies (adrenal CT scan and adrenal scintigraphy with I123-MIBG). All patients received treatment with alpha-blockers (Doxazosin®) in preoperatively-adapted doses to control blood pressure and secretion blockade. In two patients, it was necessary to add low doses of beta-blockers (Bisoprolol®) to control heart rate. Preoperative adrenal function (cortisol, ACTH, electrolytes) was normal in all included cases.
All patients were offered posterior retroperitoneal endoscopic adrenalectomy (a standardized technique that we have used since 2011), and informed consent was obtained. In terms of the surgical technique, the modified jack-knife prone position of the patient should be highlighted.
Initially, an incision was made below the 12th right or left rib (depending on laterality) and a small space was created in the retroperitoneal area. Afterwards, another 5-mm lateral trocar was inserted. Carbon dioxide was insufflated at a pressure of about 20mmHg into the retroperitoneal space. The dissection was carried out through the renal fascia until the paravertebral muscles were identified. A third medial trocar measuring 12mm was inserted. After descending the superior renal pole, the adrenal gland was located. The next step involved partial resection of the gland with endoscopic sealant, preserving the healthy adrenal cortex as well as its main draining vein and part of the arterial pedicle. As a last step, the tumor was extracted by means of a bag through a 12-mm port. Drains were not routinely inserted.
The variables analyzed included: patient characteristics (age, sex, body mass index, syndrome with the genetic mutation and laterality of the lesion), data obtained for the diagnosis (plasma metanephrine, imaging tests, adrenal function and symptoms), intraoperative data (approach, surgical time, blood loss and incidents during the intervention) and finally the data obtained in the postoperative period (monitoring of adrenal function, adrenal hormone replacement requirements, complications, hospital stay, recurrence of pheochromocytoma on imaging and hormonal studies). Once all the information was registered in a database in an anonymous and coded form, the statistical analysis was completed using the SPSS® 12.0 for Windows program. The results are expressed as median (range) or mean±standard deviation (SD), as appropriate.
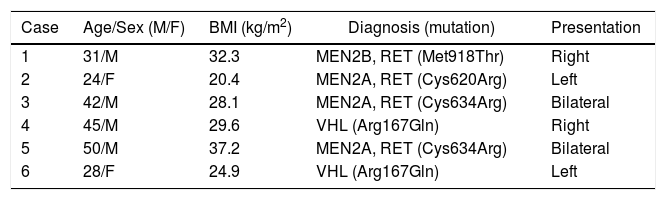
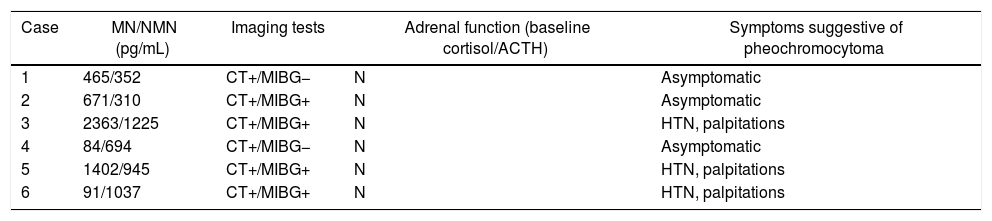
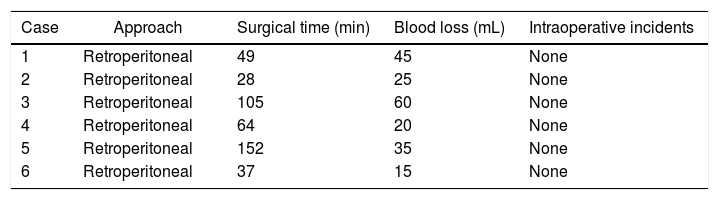
ResultsA total of 6 patients were included in the study, with a mean age of 36±16 years and a mean BMI of 28.7kg/m2 (range 20.4–37.2). Pertinent medical history included three patients who had had previous abdominal surgery. Regarding the etiology of the adrenal lesions, two patients presented bilateral pheochromocytoma at diagnosis in the context of the MEN 2A syndrome, so it was decided to perform a double approach during one operation. The four other patients had previous total adrenalectomy of the contralateral gland. Two were associated with VHL syndrome and two were in the context of the MEN 2A syndrome (Table 1). Diagnosis was based on blood analysis, and increased plasma metanephrine and normetanephrine levels were detected according to their etiology (MEN 2 versus VHL) in all cases. In the imaging study, the adrenal lesion was observed on CT and, if alterations were confirmed both analytically and by imaging studies, an adrenal scintigraphy was performed with I123-MIBG as well as magnetic resonance (Table 2). In all cases, adrenal surgery was completed by the retroperitoneal endoscopic approach, without the need for conversion to open or laparoscopic surgery. The average surgical time was 45±26min for unilateral adrenalectomy and 128±23min for bilateral. Blood loss was 33±14mL. There were no intra- or postoperative complications and there was no mortality in the series (Table 3).
Clinical Characteristics of the Patients Treated.
| Case | Age/Sex (M/F) | BMI (kg/m2) | Diagnosis (mutation) | Presentation |
|---|---|---|---|---|
| 1 | 31/M | 32.3 | MEN2B, RET (Met918Thr) | Right |
| 2 | 24/F | 20.4 | MEN2A, RET (Cys620Arg) | Left |
| 3 | 42/M | 28.1 | MEN2A, RET (Cys634Arg) | Bilateral |
| 4 | 45/M | 29.6 | VHL (Arg167Gln) | Right |
| 5 | 50/M | 37.2 | MEN2A, RET (Cys634Arg) | Bilateral |
| 6 | 28/F | 24.9 | VHL (Arg167Gln) | Left |
Arg: arginine; Cys: cysteine; Gln: glutamine; M: male; BMI: body mass index; F: female; MEN2: multiple endocrine neoplasia type 2; Met: methionine; Thr: threonine; VHL: Von Hippel-Lindau disease.
Preoperative Characteristics in the Diagnosis of Pheochromocytoma.
| Case | MN/NMN (pg/mL) | Imaging tests | Adrenal function (baseline cortisol/ACTH) | Symptoms suggestive of pheochromocytoma |
|---|---|---|---|---|
| 1 | 465/352 | CT+/MIBG− | N | Asymptomatic |
| 2 | 671/310 | CT+/MIBG+ | N | Asymptomatic |
| 3 | 2363/1225 | CT+/MIBG+ | N | HTN, palpitations |
| 4 | 84/694 | CT+/MIBG− | N | Asymptomatic |
| 5 | 1402/945 | CT+/MIBG+ | N | HTN, palpitations |
| 6 | 91/1037 | CT+/MIBG+ | N | HTN, palpitations |
ACTH: adrenocorticotropic hormone; HTN: hypertension; MIGB: scintigraphy with meta-iodobenzylguanidine; MN/NMN: metanephrine/normetanephrine, normal values: MN<90 and NMN<200pg/mL; mL: milliliters; N: normal; pg: picograms; CT: computed tomography.
Intraoperative Characteristics of the Patients Treated.
| Case | Approach | Surgical time (min) | Blood loss (mL) | Intraoperative incidents |
|---|---|---|---|---|
| 1 | Retroperitoneal | 49 | 45 | None |
| 2 | Retroperitoneal | 28 | 25 | None |
| 3 | Retroperitoneal | 105 | 60 | None |
| 4 | Retroperitoneal | 64 | 20 | None |
| 5 | Retroperitoneal | 152 | 35 | None |
| 6 | Retroperitoneal | 37 | 15 | None |
min: minutes; mL: millilitres.
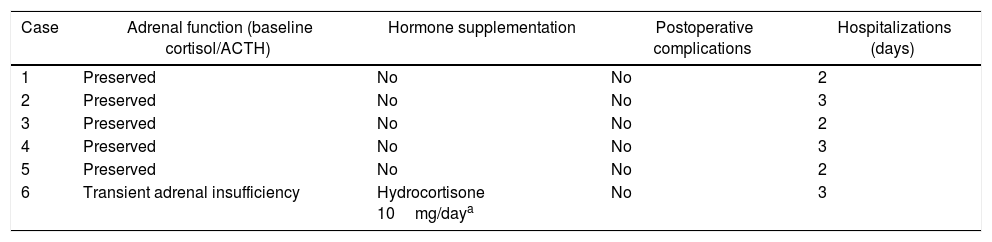
Immediate postoperative monitoring was conducted in the intermediate care unit. Patients were able to initiate oral intake the same afternoon of the surgery, and after spending 24h in observation, all were transferred to the hospital ward. The six patients presented rapid normalization of plasma metanephrine and normetanephrine levels, as well as, if present, remission of symptoms secondary to pheochromocytoma. Patients with preservation of the adrenal cortex maintained adrenal function (basal cortisol, ACTH, Na, K) within normal ranges, in both unilateral and bilateral cases. In one case, complete unilateral adrenalectomy was performed, with transient adrenal insufficiency observed during the immediate postoperative period with the need for partial replacement therapy with glucocorticoids for 3 months. No postoperative complications were recorded, and there was no mortality in the series. Mean hospital stay was 2.5 days (range 2–4). Cortical-sparing adrenalectomy was possible in all patients except one, whose lesion was greater than 5cm, making it impossible to preserve healthy tissue (Table 4). The definitive pathology study confirmed the presence of benign pheochromocytoma in all cases, with an average size of 3.7cm (range 1.7–5.1).
Postoperative Characteristics of the Patients Treated.
| Case | Adrenal function (baseline cortisol/ACTH) | Hormone supplementation | Postoperative complications | Hospitalizations (days) |
|---|---|---|---|---|
| 1 | Preserved | No | No | 2 |
| 2 | Preserved | No | No | 3 |
| 3 | Preserved | No | No | 2 |
| 4 | Preserved | No | No | 3 |
| 5 | Preserved | No | No | 2 |
| 6 | Transient adrenal insufficiency | Hydrocortisone 10mg/daya | No | 3 |
ACTH: adrenocorticotropic hormone.
During a mean follow-up period of 26.2±6 months, no patients had recurrence on hormone studies or imaging tests. Therefore, the remission rate for patients with spared adrenal cortex was 100%. In terms of mid-term adrenal function, the 5 patients in whom unilateral adrenal cortex preservation was possible, as well as the patient who underwent unilateral total adrenalectomy, experienced preserved hormonal function without replacement therapy.
Presently, the patients continue to be followed up by the endocrinology department at our hospital. Annual studies are done of the adrenal axis function and any possible recurrence of pheochromocytoma using hormone tests with plasma metanephrine, baseline cortisol, ACTH, serum biochemistry (Na, K, FG, etc.) and imaging tests (adrenal CT). To date, no tumor recurrence has been observed in any of the patients with cortical preservation of the adrenal gland.
DiscussionCurrently, the indications for cortical-sparing adrenalectomy have not been clearly defined. However, its implementation is accepted in patients with hereditary bilateral pheochromocytoma, mainly in the context of genetic syndromes that associate benign pheochromocytomas. While there is a risk of recurrence in the adrenal remnant, the cortical-sparing technique is increasingly requested by well-informed patients to prevent corticosteroid replacement therapy and the danger posed by Addisonian crises. There is also consensus that a family history of malignant pheochromocytoma10 or the presence of associated mutations6 would represent an absolute contraindication to this procedure. In our series, there have been no cases of malignant pheochromocytoma. Since the first laparoscopic adrenalectomy due to pheochromocytoma performed in the early 1990s,11 the transperitoneal laparoscopic technique has been replacing the open approach to become the current gold standard12 for the treatment of patients with adrenal tumors. This method has demonstrated clear advantages over open surgery,13 including less blood loss as well as shorter hospitalization time, faster recovery and lower healthcare costs.
Although partial adrenal resection is considered to have advantages in certain patients, especially in those with bilateral tumors, preservation using the anterior laparoscopic approach is considered technically difficult. It implies an elevated risk of parenchymal hemorrhage and, according to most authors, it requires eccentric location of the lesion on the gland, together with a tumor diameter of less than 3cm and preservation of around 30% of the gland.14 In series published by groups that have conducted this procedure, functional results have not been as expected, requiring corticoid replacement therapy after surgery in up to 60% of cases.15 As Sasagawa et al.16 have shown, the retroperitoneal endoscopic approach seems to have specific advantages compared with the transperitoneal laparoscopic approach. Access to the peritoneal cavity is completely avoided and, as there is no manipulation or mobilization of the intestine, functional postoperative recovery is faster. The technique would also be of choice for patients with intraperitoneal adhesions secondary to previous abdominal surgery, eliminating the risk of intestinal injuries and reducing operative time. In our series, 3 (50%) out of 6 patients had undergone previous surgery, two of them (33%) by laparotomy.
According to the Walz group,17 cortical preservation using retroperitoneal endoscopy provides a magnified view of the gland and its vascularization, which allows the surgeon to perform a meticulous dissection and draw a safe resection plane to preserve healthy tissue, while removing the tumor without breaking it. In addition, the operative time for the posterior retroperitoneal endoscopic approach reported in large patient series is less than 70min.17,18 In our series, it was 45min on average. In both instances, the operation is shorter than the surgical times published for transabdominal adrenalectomy.19 Another relevant aspect is the limited blood loss that occurs in the retroperitoneal approach, which was less than 50mL in all patients in our series, similar to reports of other groups using the same approach20 and clearly lower than the anterior laparoscopic approach.21 Similarly, the postoperative morbidity published in retroperitoneal endoscopy series is very low; in fact, our group of patients did not present any complications. All these benefits provide for excellent patient recovery in a short period of time. Thus, hospital admission is short, as in our study (mean stay of 2.5 days), which should imply a lower healthcare costs, as stated by Kiriakopoulos et al.22
Except for the Professor Walz et al. study,23 the series published to date are small in patient numbers. Despite this, when both approaches are compared, some benefits of the posterior retroperitoneal endoscopic approach are confirmed, such as prompt postoperative recovery.24,25 There do not seem to be significant differences if complications are compared with total adrenalectomy, provided it is performed by surgeons with extensive experience in minimally invasive techniques as well as endocrine surgery.26
As demonstrated in our group, the functional results obtained after the preservation of the adrenal cortex are excellent after retroperitoneal endoscopy. Five (83%) out of our 6 patients continue to have no need for hormone replacement therapy. These results coincide with those from other groups using the same approach27 and are superior to the results from published series using a laparoscopic approach.28 Retroperitoneal endoscopic adrenalectomy with preservation of the adrenal cortex is a safe and feasible technique in the hands of experienced surgeons. It is also an appropriate technical option for patients with bilateral pheochromocytoma in whom we have ruled out mutations associated with a high malignancy index (mutations for SDHB or MAX) in order to avoid the need for life-long hormone replacement therapy with corticosteroids, with no increased risk of recurrence in these patients.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Vidal Ó, Delgado-Oliver E, Díaz del Gobbo R, Hanzu F, Squarcia M, Martínez D, et al. Preservación de corteza adrenal funcionante. Una buena razón para realizar abordaje endoscópico retroperitoneal posterior. Cir Esp. 2018;96:488–493.