Vital signs indicate the presence of bleeding only after large amounts of blood have been lost, with high morbidity and mortality. The Shock Index (SI) is a hemorrhage indicator with a cut-off point for the risk of bleeding at 0.9. The aim of this study is to assess whether a cut-off of ≥0.8 is more sensitive for detecting occult bleeding, providing for early initiation of therapeutic maneuvers.
MethodsSI analytical validation study of severe trauma patients older than 16 years of age. Vital signs were recorded, and scales for predicting bleeding included: SI, Assessment of Blood Consumption score, and Pulse Rate Over Pressure score. The relationship between the SI and 5 markers for bleeding was analyzed: need for massive transfusion, angiographic embolization, surgical bleeding control, death due to hypovolemic shock, and the overall predictor “active bleeding” (defined as the presence of at least one of the 4 markers above).
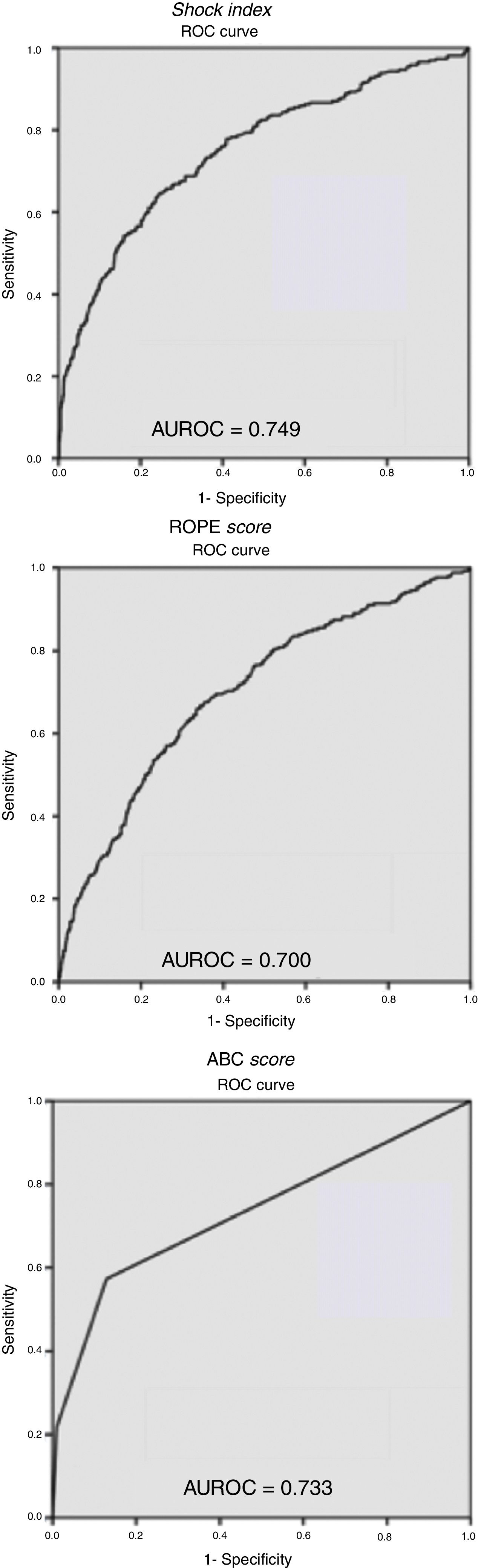
ResultsData from 1402 trauma patients were collected prospectively over a period of 10 years. The mean Injury Severity Score was 20.9 (SD 15.8). The mortality rate was 10%. The mean SI was 0.73 (SD 0.29). “Active bleeding” was present in 18.7% of patients. The SI area under the ROC curve for “active bleeding” was 0.749.
ConclusionsAn SI cut-off point ≥0.8 is more sensitive than ≥0.9 and allows for earlier initiation of resuscitation maneuvers in patients with occult active bleeding.
Las constantes vitales detectan la presencia de hemorragia al perder grandes cantidades de sangre, lo que comporta una gran morbimortalidad. El Shock Index (SI) es un parámetro que detecta el sangrado con puntos de corte de 0,9. El objetivo de este estudio es valorar si un punto de corte de ≥0,8 es más sensible para detectar sangrado oculto, permitiendo iniciar maniobras terapéuticas más precoces.
MétodosEstudio analítico de validación del SI que incluye pacientes politraumatizados graves mayores de 16 años. Se registran constantes vitales y escalas predictivas de sangrado: SI, Assessment of Blood Consumption score y Pulse Rate Over Pressure score. Se analiza la relación del SI con 5 marcadores predictivos de sangrado: necesidad de transfusión masiva, embolización angiográfica, control del sangrado quirúrgico, muerte por shock hipovolémico y «sangrado activo» (presencia de al menos uno de los 4 marcadores anteriores en un paciente).
ResultadosRecogida prospectiva de datos de 1.402 pacientes politraumatizados durante 10 años. El Injury Severity Score medio fue de 20,9 (DE 15,8). Hubo una mortalidad del 10%. El SI medio fue de 0,73 (DE 0,29). En total presentaron «sangrado activo» el 18,7% de la serie. El SI medio en los pacientes con «sangrado activo» fue de 0,87, mientras que las constantes vitales estaban dentro de la normalidad. El área bajo la curva ROC del SI para el «sangrado activo» fue de 0,749.
ConclusionesEl SI con un punto de corte ≥0,8 es más sensible que aquel con el punto de corte ≥0,9 y permite iniciar maniobras de reanimación más precoces en los pacientes con sangrado oculto.
Polytrauma is one of the main causes of death in the population between the ages of one and 44.1 Hemorrhagic shock is the leading cause of avoidable death after trauma and causes approximately one-third of the 6 million annual trauma-related deaths.2 After severe trauma injuries, early detection of shock is necessary for adequate management to help reduce morbidity and mortality.3 The classic markers of hemodynamic stability are skin characteristics, heart rate, blood pressure and diuresis.4 Unfortunately, these parameters can be altered due to pain, hypothermia, neurogenic shock, cardiogenic shock, analgesic medication or beta-blockers; as a result, the interpretation of vital signs may become altered.5 Another limitation that can be found when analyzing these parameters is their later modification: elevated heart rate above 100–120bpm is recorded when patients have lost around 750–1500mL of blood volume, while decreased blood pressure is observed when patients have lost between 1500 and 2000mL of blood volume.6 The delay in the early identification of patients with active hemorrhage often delays the application of therapies that are essential for the control of bleeding (activation of the massive transfusion protocol [MTP], angiographic embolization, urgent surgery, etc.) and is a cause of mortality during initial care.7 For this reason, in recent years, different mechanisms have been proposed to identify patients with a high probability of bleeding, such as the Trauma Associated Severe Hemorrhage Score,8 Assessment of Blood Consumption score (ABC),9 McLaughlin score,10 Pulse Rate Over Pressure Evaluation score (ROPE)11,12 and the Shock Index (SI).13
Defined as heart rate divided by systolic blood pressure, the SI has been proposed as a simple and early tool to identify patients with hemorrhagic shock. It is considered a good indicator of the need for massive transfusion,14 the need to control the bleeding point15 and even mortality.16 Initially, the cut-off point of ≥1 was defined for established hypovolemic shock, which has a greater specificity and is more recommended for prehospital use. Over time, the threshold has been lowered to increase its predictive capacity, and a controversy has developed between 2 cut-off points: ≥0.93,13,16 and ≥0.8,15,17 the former being most often used in the current literature. The main drawback of the ≥0.9 cut-off point is that, when used, we run the risk of losing patients who have occult bleeding. Therefore, the ≥0.8 cut-off point is now being proposed, which is less restrictive and can detect patients with undetected bleeding, although it makes a wider selection of patients, among them a greater number of false positives. The aim of this study was to assess whether the ≥0.8 cut-off point is more sensitive than ≥0.9 for predicting hypovolemic shock.
MethodsWe conducted an analytical study for SI validation at a single medical center including polytrauma patients treated at a tertiary hospital who were over the age of 16 and had either entered the critical care unit or died before admission to the unit (intrahospital). All patients were registered prospectively in a protected database designed in Access® in order to avoid the entry of erroneous or out-of-range values. Spanish laws for the protection of personal data were followed at all times. The registered variables included: sex, age, mechanism of injury, severity criterion (Injury Severity Score), hospital vital signs (heart rate, systolic blood pressure) and causes of mortality. All data were reviewed clinically at a later date and in a cyclical manner by a committee specialized in polytrauma patient care. Definitions of the prediction scales for bleeding:
- 1.
SI: heart rate divided by systolic blood pressure.18 Normal values range between 0.5 and 0.7.19
- 2.
ROPE: heart rate divided by the difference between the systolic blood pressure and the diastolic blood pressure. Values ≥3 are considered a predictor of massive transfusion.11,12
- 3.
ABC: calculated by assigning a value of 0 or 1 to the presence of penetrating trauma, focused assessment with sonography in trauma (FAST), systolic blood pressure <90mmHg and heart rate >120bpm. Values ≥2 are defined as predictors of massive transfusion.9,20
The following markers for bleeding were used:
- 1.
Activation of MTP
- 2.
Angiographic embolization: conducted with endovascular access
- 3.
Surgery to control bleeding
- 4.
Mortality due to hypovolemic shock
For the regression analysis, a binary categorical variable was required. The variable must reflect that the patient is bleeding or has been bleeding. To construct this variable, the previously described bleeding markers were used. If a patient presented one or more of the bleeding markers, the bleeding was defined as “active” in this variable that we created de novo. Obviously a patient could have one, 2, 3 or 4 markers. The correlation between the SI, ROPE and ABC was analyzed with the markers described above, with different age groups (16–64 years; over 65) and the mechanism of injury (penetrating or blunt). Data are presented as mean and standard deviation (SD) for the continuous variables and as percentages for the categorical variables.
Statistical AnalysisFor the univariate study, the Student's t test was used for continuous variables and the Chi-squared for categorical variables.
Receiver operating characteristic (ROC) curves were obtained (as a graphic representation of the discriminative capacity of a certain scale with all its cut-off points), and the areas under the ROC curve (AUROC) were calculated for the scales, presented with their 95% confidence intervals.
The sensitivity, specificity, positive predictive value and negative predictive value were calculated for the variable “active bleeding”, using the SI cut-off points of ≥0.8 and ≥0.9.
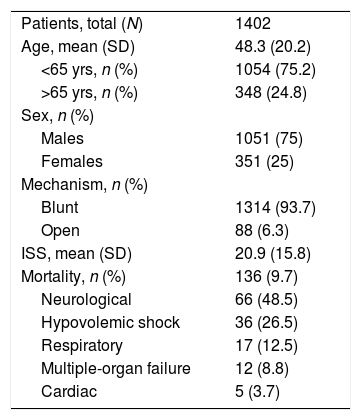
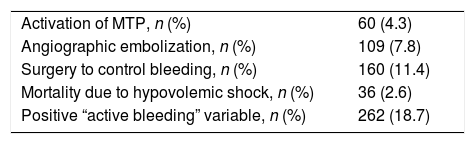
ResultsFrom March 2006 to September 2016, 1402 polytrauma patients were treated at our hospital. Average age was 48.3 years, and the average Injury Severity Score was 20.9 (SD 15.8). The series mortality rate was 10% (136 patients), the most frequent cause being neurological (48.5%) (Table 1). Mean SI was 0.73 (SD 0.29); 266 patients (19%) had an SI greater than 0.9 and 395 patients (28.2%) had an SI greater than 0.8. Mean ROPE was 2 (SD 1.3), and mean AUC was 0.3 (SD 0.6). MTP was activated in 60 patients (4.3%). Angiography with embolization was performed in 109 patients (7.8%), and 160 patients required surgery to control bleeding (11.4%). In total, 262 patients presented “active bleeding”, representing 18.7% of the series. 2.6% of the patients died due to hypovolemic shock (Table 2). The correlation between vital signs (heart rate and systolic blood pressure) and the different predictive scales for bleeding with the bleeding markers are shown in Table 3, together with their significance. The mean value of the SI was above the cut-off point defined in the literature (≥0.9) in all patients with bleeding.
General Data.
| Patients, total (N) | 1402 |
| Age, mean (SD) | 48.3 (20.2) |
| <65 yrs, n (%) | 1054 (75.2) |
| >65 yrs, n (%) | 348 (24.8) |
| Sex, n (%) | |
| Males | 1051 (75) |
| Females | 351 (25) |
| Mechanism, n (%) | |
| Blunt | 1314 (93.7) |
| Open | 88 (6.3) |
| ISS, mean (SD) | 20.9 (15.8) |
| Mortality, n (%) | 136 (9.7) |
| Neurological | 66 (48.5) |
| Hypovolemic shock | 36 (26.5) |
| Respiratory | 17 (12.5) |
| Multiple-organ failure | 12 (8.8) |
| Cardiac | 5 (3.7) |
SD: standard deviation; ISS: Injury Severity Score.
Relationship of Bleeding Markers With Vital Signs Using the Scales Analyzed.
| N Total: 1402 | HR | SBP | SI | ROPE | ABC | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes/No | N (%) | Mean (SD) | P | Mean (SD) | P | Mean (SD) | P | Mean (SD) | P | Mean (SD) | P | |
| “Active bleeding” variable | Yes | 262 (18.7) | 98 (25) | <.001 | 110 (31) | <.001 | 0.97 (0.41) | <.001 | 2.77 (1.84) | <.001 | 0.82 (0.85) | <.001 |
| No | 1140 (81.3) | 86 (19) | 132 (25) | 0.67 (0.22) | 1.85 (1.05) | 0.12 (0.38) | ||||||
| Activation of massive transfusion protocol | Yes | 60 (4.3) | 111 (25) | <.001 | 92 (29) | <.001 | 1.31 (0.44) | <.001 | 3.78 (2.36) | <.001 | 1.33 (0.90) | <.001 |
| No | 1342 (95.7) | 87 (20) | 130 (26) | 0.70 (0.25) | 1.94 (1.16) | 0.22 (0.50) | ||||||
| Angiographic embolization | Yes | 109 (7.6) | 96 (23) | .04 | 113 (33) | <.001 | 0.93 (0.38) | <.001 | 2.69 (2.17) | <.001 | 0.60 (0.72) | <.001 |
| No | 1293 (92.2) | 87 (20) | 129 (27) | 0.71 (0.28) | 1.96 (1.17) | 0.2 (0.5) | ||||||
| Surgery to control bleeding | Yes | 160 (114) | 100 (24) | <.001 | 107 (30) | <.001 | 1.03 (0.43) | <.001 | 2.94 (1.71) | <.001 | 1.04 (0.89) | <.001 |
| No | 1242 (88.6) | 86 (19) | 131 (26) | 0.69 (0.24) | 1.90 (1.17) | 0.16 (0.4) | ||||||
| Death due to hypovolemic shock | Yes | 36 (2.6) | 104 (27) | <.001 | 102 (39) | <.001 | 1.16 (0.48) | <.001 | 3.44 (2.22) | <.001 | 1.25 (0.87) | <.001 |
| No | 1366 (97.4) | 87 (20) | 129 (27) | 0.71 (0.27) | 1.98 (1.23) | 0.24 (0.53) | ||||||
ABC: Assessment of Blood Consumption; SD: standard deviation; HR: heart rate; ROPE: Pulse Rate Over Pressure Evaluation; SI: Shock Index; SBP: systolic blood pressure
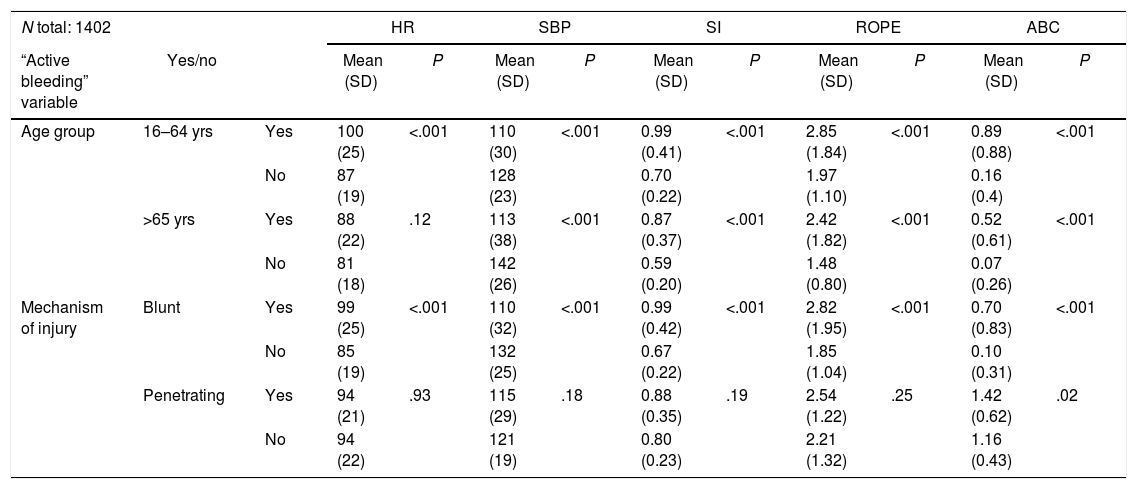
When the “active bleeding” variable was applied to the 2 age groups (young patients, 16–64 years old; and seniors, >65 years old), we observed that the vital signs and the scales evaluated had a statistically significant relationship, except for heart rate in the seniors, which was not significant (Table 4). It should be noted that, in the older patient group, mean vital signs remained within the ranges for clinical normality, while the SI was ≥0.8. The relationship between vital signs and the scales evaluated with the mechanism of injury showed a statistically significant relationship with blunt trauma, but with penetrating trauma this was only statistically significant using the ABC score. When we analyzed the SI cut-off points studied, we observed how they correlated in a statistically significant way with all the variables, showing a non-significant relationship with penetrating trauma (Table 5).
Relationship Between the “Active Bleeding” Variable With the Age Group and Mechanism of Injury.
| N total: 1402 | HR | SBP | SI | ROPE | ABC | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| “Active bleeding” variable | Yes/no | Mean (SD) | P | Mean (SD) | P | Mean (SD) | P | Mean (SD) | P | Mean (SD) | P | |
| Age group | 16–64 yrs | Yes | 100 (25) | <.001 | 110 (30) | <.001 | 0.99 (0.41) | <.001 | 2.85 (1.84) | <.001 | 0.89 (0.88) | <.001 |
| No | 87 (19) | 128 (23) | 0.70 (0.22) | 1.97 (1.10) | 0.16 (0.4) | |||||||
| >65 yrs | Yes | 88 (22) | .12 | 113 (38) | <.001 | 0.87 (0.37) | <.001 | 2.42 (1.82) | <.001 | 0.52 (0.61) | <.001 | |
| No | 81 (18) | 142 (26) | 0.59 (0.20) | 1.48 (0.80) | 0.07 (0.26) | |||||||
| Mechanism of injury | Blunt | Yes | 99 (25) | <.001 | 110 (32) | <.001 | 0.99 (0.42) | <.001 | 2.82 (1.95) | <.001 | 0.70 (0.83) | <.001 |
| No | 85 (19) | 132 (25) | 0.67 (0.22) | 1.85 (1.04) | 0.10 (0.31) | |||||||
| Penetrating | Yes | 94 (21) | .93 | 115 (29) | .18 | 0.88 (0.35) | .19 | 2.54 (1.22) | .25 | 1.42 (0.62) | .02 | |
| No | 94 (22) | 121 (19) | 0.80 (0.23) | 2.21 (1.32) | 1.16 (0.43) | |||||||
ABC: Assessment of Blood Consumption; SD: standard deviation; HR: heart rate; ROPE: Pulse Rate Over Pressure evaluation; SI: Shock Index; SBP: systolic blood pressure.
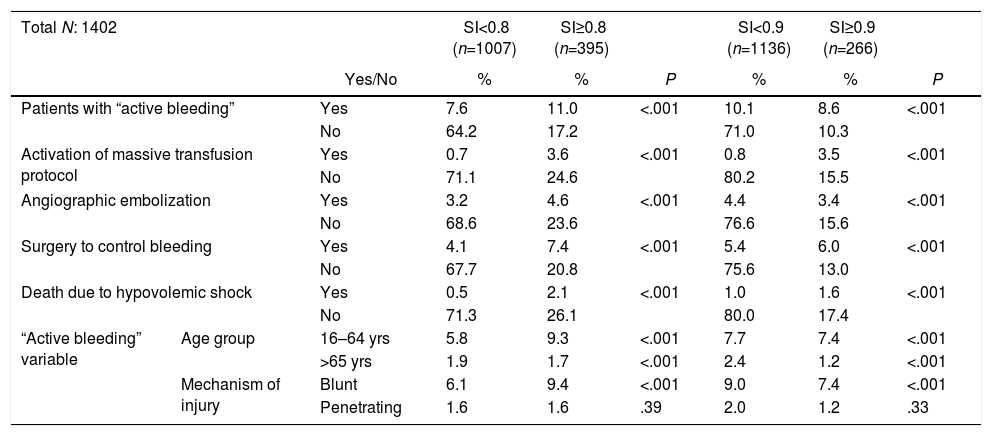
Correlation Between the Shock Index Cut-Off Points and the Different Variables Analyzed.
| Total N: 1402 | SI<0.8 (n=1007) | SI≥0.8 (n=395) | SI<0.9 (n=1136) | SI≥0.9 (n=266) | ||||
|---|---|---|---|---|---|---|---|---|
| Yes/No | % | % | P | % | % | P | ||
| Patients with “active bleeding” | Yes | 7.6 | 11.0 | <.001 | 10.1 | 8.6 | <.001 | |
| No | 64.2 | 17.2 | 71.0 | 10.3 | ||||
| Activation of massive transfusion protocol | Yes | 0.7 | 3.6 | <.001 | 0.8 | 3.5 | <.001 | |
| No | 71.1 | 24.6 | 80.2 | 15.5 | ||||
| Angiographic embolization | Yes | 3.2 | 4.6 | <.001 | 4.4 | 3.4 | <.001 | |
| No | 68.6 | 23.6 | 76.6 | 15.6 | ||||
| Surgery to control bleeding | Yes | 4.1 | 7.4 | <.001 | 5.4 | 6.0 | <.001 | |
| No | 67.7 | 20.8 | 75.6 | 13.0 | ||||
| Death due to hypovolemic shock | Yes | 0.5 | 2.1 | <.001 | 1.0 | 1.6 | <.001 | |
| No | 71.3 | 26.1 | 80.0 | 17.4 | ||||
| “Active bleeding” variable | Age group | 16–64 yrs | 5.8 | 9.3 | <.001 | 7.7 | 7.4 | <.001 |
| >65 yrs | 1.9 | 1.7 | <.001 | 2.4 | 1.2 | <.001 | ||
| Mechanism of injury | Blunt | 6.1 | 9.4 | <.001 | 9.0 | 7.4 | <.001 | |
| Penetrating | 1.6 | 1.6 | .39 | 2.0 | 1.2 | .33 | ||
SI: Shock Index.
Pearson's Chi-squared for Shock Index values ≥0.8 and ≥0.9 for the variables studied.
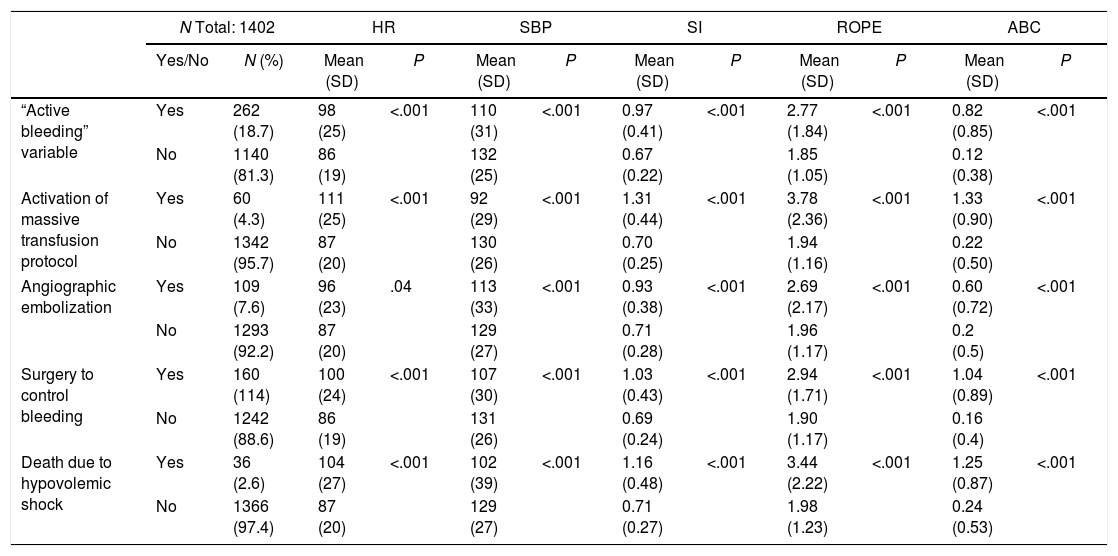
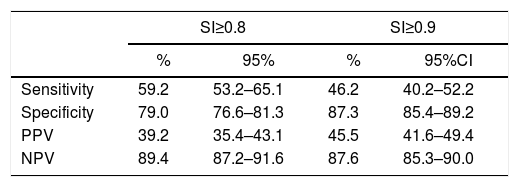
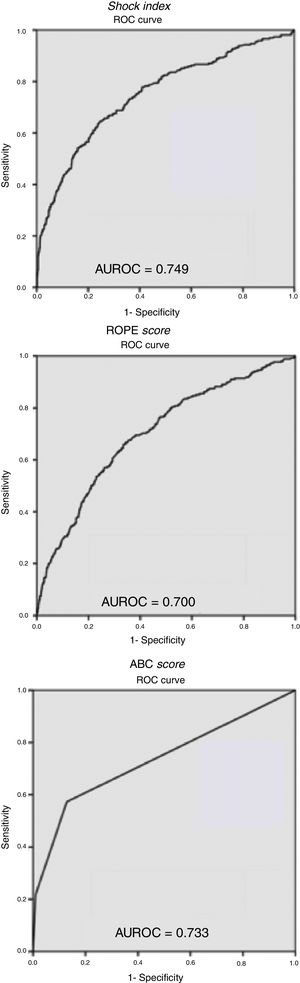
The ROC curves (Fig. 1) obtained for the studied scales showed a greater predictive capacity for SI, with an AUROC of 0.749, while the ABC score and the ROPE score had lower AUROCs of 0.733 and 0.700, respectively. Finally, when assessing the predictive capacity as a test of the 2 SI cut-off points analyzed, we can see how the ≥0.8 cut-off point presented a higher sensitivity than ≥0.9, at 59.2 and 46.2%, respectively.
ROC curves and areas under the curve (AUROC) for the Shock Index, ROPE score and ABC score. This figure includes Table 6, representing the values of sensitivity, specificity, positive predictive value and negative predictive value of the 2 Shock Index cut-off points analyzed.
The management of polytrauma patients has improved over the years thanks to a more thorough knowledge of the mechanisms contributing to increased morbidity and mortality. Since the first definition of SI in 1967 by Allgöwer and Burri,18 several authors have studied its predictive value for different outcomes (mortality, MTP, days of hospitalization, septic complications, etc.).14–16,21 With our study, we have shown that the SI cut-off point ≥0.8 correlates with all the variables analyzed (“active bleeding”, MTP activation, angiographic embolization, surgery to control bleeding and death from hypovolemic shock). The clinical applicability of these results is of great importance, since patients with SI values above 0.8 have a high probability of bleeding, even when vital signs are within normal limits.
Different publications have analyzed the applicability of SI in elderly patients, whose vital signs may seem normal even with hemorrhagic shock.22,23 Varying results have been obtained, as some publications considered it a good marker,24 while others propose the use of different cut-off points according to age group.4,21 If we analyze the results obtained by differentiating 2 age groups (16–64 of age and >65), we observe how SI ≥0.8 has the same predictive capacity as the other variables analyzed. Maximum heart rate decreases as patients age, so the ability to produce tachycardia in response to bleeding is less. This population has a higher incidence of hypertension, and a systolic blood pressure lower than 110mmHg after trauma is considered hypotensive in seniors.23 For this reason, vital signs are not considered reliable in the evaluation of geriatric patients, and the use of SI in these cases would be recommended.
Certain publications have analyzed the different markers for hemodynamic resuscitation for penetrating and closed trauma separately,25,26 without finding significant differences. The variables studied and the SI cut-off point of 0.8 are good predictors of bleeding in patients with blunt trauma, but no statistically significant results have been detected when applied to penetrating trauma. These differences may be due to a lower incidence of penetrating trauma in our series, representing only 6.3% of the patients treated, compared to 50%–70% of the publications that compare both mechanisms.25,26 If we also consider that patients with penetrating trauma undergo more surgical explorations, regardless of hemodynamic stability, it is more probable that the relationship is not statistically significant. For this reason, we cannot consider the SI a good predictor of bleeding in patients with penetrating trauma in our series. The evaluation of the ROC curves for the different scales evaluated shows how the SI has a greater predictive capacity for bleeding than the others, obtaining an AUROC of 0.749.
Differentiating the 2 SI cut-off points analyzed, SI ≥0.8 presents a sensitivity of 59.2, a specificity of 79 and a negative predictive value of 89.4. By lowering the cut-off point, we increase the sensitivity to detect bleeding while maintaining acceptable specificity levels; this allows us to affirm that the cut-off point of 0.8 enables us to correctly identify bleeding.15 As shown in Table 6, included in Fig. 1, SI with a cut-off point of 0.8 achieves an even higher negative predictive value than the cut-off point of 0.9 and can therefore affirm with a higher level of certainty that a patient with an SI less than 0.8 is not actually bleeding.
Values for Sensitivity, Specificity, PPV and NPV for the Cut-Off Points Analyzed (for a Prevalence of 18.7).
| SI≥0.8 | SI≥0.9 | |||
|---|---|---|---|---|
| % | 95% | % | 95%CI | |
| Sensitivity | 59.2 | 53.2–65.1 | 46.2 | 40.2–52.2 |
| Specificity | 79.0 | 76.6–81.3 | 87.3 | 85.4–89.2 |
| PPV | 39.2 | 35.4–43.1 | 45.5 | 41.6–49.4 |
| NPV | 89.4 | 87.2–91.6 | 87.6 | 85.3–90.0 |
PPV: positive predictive value; NPV: negative predictive value.
The limitation of this study is the loss of data during collection. At our hospital, patient base excess is not recorded in a protocolized manner. Therefore, we have not been able to apply the Trauma-Associated Severe Hemorrhage Score (currently considered one of the best) for comparison with the rest of the scales used. In conclusion, in the care of polytrauma patients with a blunt mechanism of injury, it is better to set an SI ≥0.8, thereby avoiding the loss of potentially serious patients with apparently normal vital signs.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Campos-Serra A, Montmany-Vioque S, Rebasa-Cladera P, Llaquet-Bayo H, Gràcia-Roman R, Colom-Gordillo A, et al. Aplicación del Shock Index como predictor de sangrado en el paciente politraumático. Cir Esp. 2018;96:494–500.